 Common Femoral Artery
Common Femoral ArterySurgical Anatomy of the Femoral Region
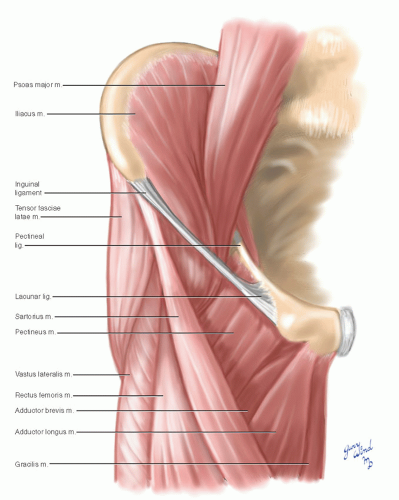
The femoral artery is the principal channel supplying blood to the lower extremity. The boundary marking the transition between the external iliac and common femoral arteries is the inguinal ligament. The artery lies just medial to the midpoint of the inguinal ligament, within a triangular passage between the pelvis and thigh. This femoral vascular aperture is bounded laterally by the iliopsoas muscles, medially by the reflected fibers of the inguinal ligament (forming the lacunar ligament), and posteriorly by the superior ramus of the pubis (Fig. 15-1).
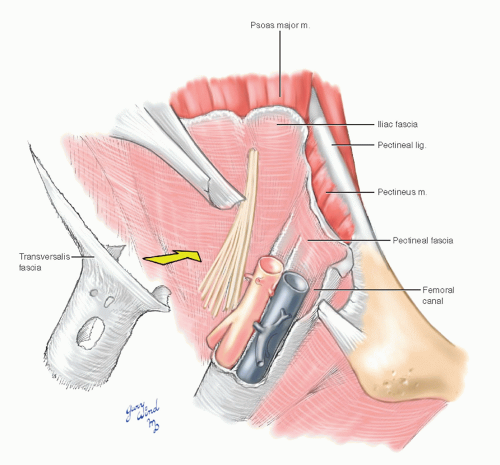
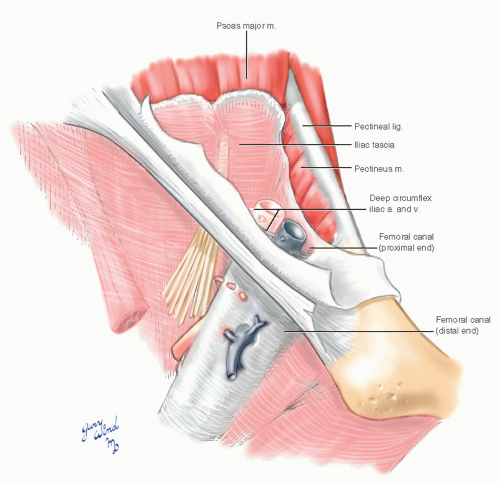
The proximal femoral artery and vein are wrapped in a fibrous covering called the femoral sheath. This sheath is made up of several components (Fig. 15-2). The lateral part of the sheath adjacent to the femoral nerve is the continuation of the iliac fascia covering the iliopsoas muscle. The posterior portion of the sheath is the fascia covering the pectineus muscle. Anteriorly and medially, the sheath is a tubular extension of the transversalis endoabdominal fascia lining the anterior abdominal wall. Within the sheath, there is a well-developed septum separating the artery from the vein. The sheath fits snugly around the vessels except on the medial side, where a narrow channel (femoral canal)
accommodates the passage of lymphatics. The pelvic end of this channel is covered with weak fascia and is the site through which a femoral hernia passes (Fig. 15-3). The femoral sheath becomes continuous with the adventitia of the vessels at the origin of the deep femoral artery and vein. The sheath is perforated by small arterial branches and the great saphenous vein.
accommodates the passage of lymphatics. The pelvic end of this channel is covered with weak fascia and is the site through which a femoral hernia passes (Fig. 15-3). The femoral sheath becomes continuous with the adventitia of the vessels at the origin of the deep femoral artery and vein. The sheath is perforated by small arterial branches and the great saphenous vein.
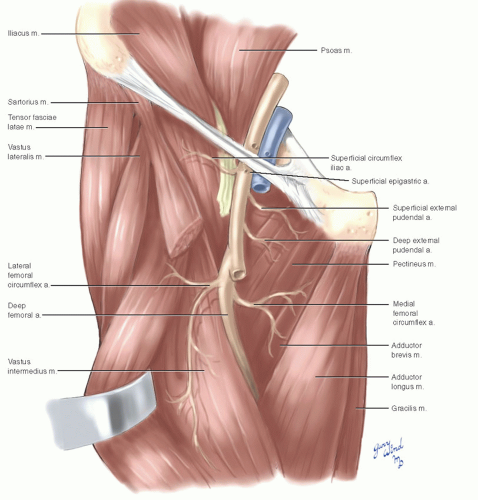
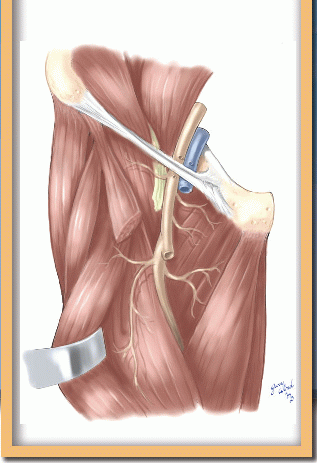
Wrapped in their sheath, the femoral vessels lie cradled in a bed of muscles (Fig. 15-4). The course of the vessels in the proximal third of the thigh lies within another triangular space defined by muscular boundaries (Scarpa’s triangle). The lateral margin of the triangle is formed by the sartorius muscle, the medial margin by the adductor longus muscle, and the cephalad base of the
triangle by the inguinal ligament. Between these boundaries, the triangle appears as a depressed plane when the thigh is flexed in external rotation (Fig. 15-5).
triangle by the inguinal ligament. Between these boundaries, the triangle appears as a depressed plane when the thigh is flexed in external rotation (Fig. 15-5).
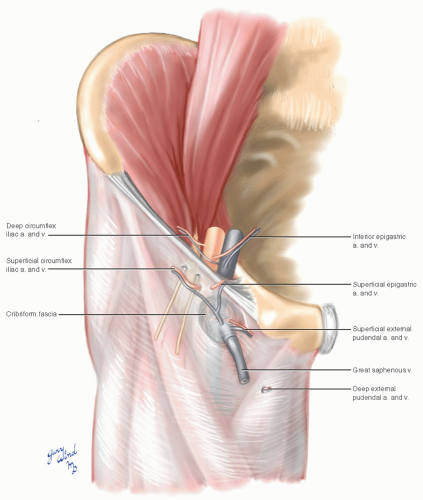
The fascia lata forms an anterior roof over the femoral triangle and attaches to the inguinal ligament. It is breached by an oval opening (fossa ovalis) through which lymphatics and the great saphenous
vein pass (Fig. 15-6). The fossa ovalis is covered by the poorly defined cribriform fascia, which supports one of two groups of superficial subinguinal lymph nodes (Fig. 15-7). The more cephalad group of nodes parallels the inguinal ligament. These nodes lie in the path of an anterior groin incision onto the femoral artery, and the rich plexus of lymphatic channels surrounding these nodes increases the
risk of lymphocele after incisions in this area. Both groups of nodes drain to the deep subinguinal nodes found in the fatty areolar tissue within the femoral triangle, and from there lymph drains through the femoral canal to the external iliac chain.
vein pass (Fig. 15-6). The fossa ovalis is covered by the poorly defined cribriform fascia, which supports one of two groups of superficial subinguinal lymph nodes (Fig. 15-7). The more cephalad group of nodes parallels the inguinal ligament. These nodes lie in the path of an anterior groin incision onto the femoral artery, and the rich plexus of lymphatic channels surrounding these nodes increases the
risk of lymphocele after incisions in this area. Both groups of nodes drain to the deep subinguinal nodes found in the fatty areolar tissue within the femoral triangle, and from there lymph drains through the femoral canal to the external iliac chain.
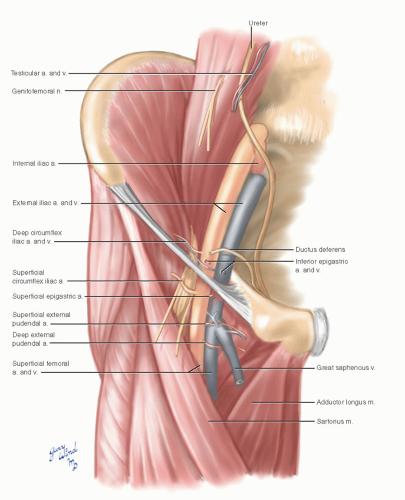
Three superficial branches of the femoral artery arise just distal to the inguinal ligament and penetrate both the femoral sheath and fascia lata to reach the subcutaneous tissue of the lower abdomen and upper thigh. These are the superficial external pudendal, superficial circumflex iliac, and superficial epigastric arteries. Their accompanying veins converge on the great saphenous vein near its junction with the femoral vein. These vessels should be
protected if possible when incising directly down to the femoral artery. The superficial epigastric pedicle has long been used to support an axial lower abdominal skin flap. The superficial external pudendal artery crosses the femoral vein immediately adjacent to the saphenofemoral junction.
protected if possible when incising directly down to the femoral artery. The superficial epigastric pedicle has long been used to support an axial lower abdominal skin flap. The superficial external pudendal artery crosses the femoral vein immediately adjacent to the saphenofemoral junction.
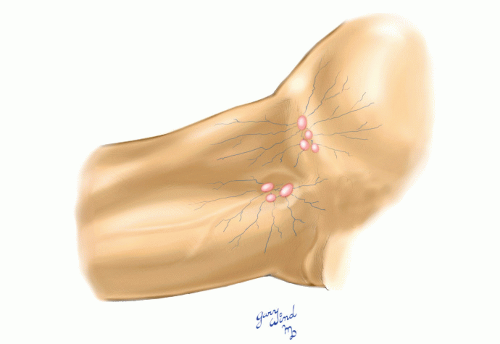 Fig. 15-7 The superficial inguinal lymph nodes are clustered beneath the inguinal ligament and around the fossa ovalis. |
Before peeling back the fascia lata to examine the deeper structures of the femoral triangle, we should briefly look at the relationships of the external iliac artery just inside the abdominal wall to anticipate the major route through which bypass grafts to the femoral artery must pass.
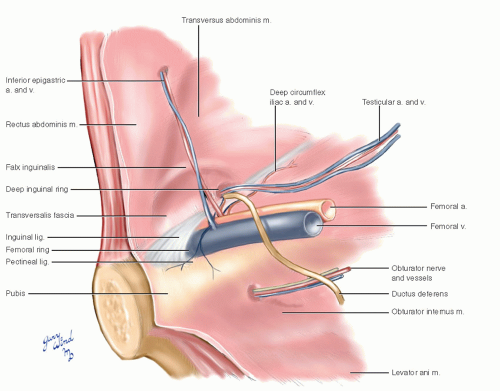 Fig. 15-8 A medial view of the right superior pubic ramus stripped of peritoneum shows the relationships of the femoral and obturator vessels. |
Just inside the abdominal wall, the external iliac artery gives off two small branches that run in the plane between the peritoneum and the transversalis fascia (Fig. 15-8). The inferior epigastric artery runs
toward the umbilicus, penetrating the transversalis fascia below the arcuate line of the posterior rectus sheath to reach the lower third of the rectus abdominis muscle. Immediately after its origin, the inferior epigastric sends a small branch with the internal oblique fibers that form the cremasteric covering of the spermatic cord in the male. The second small branch of the terminal external iliac artery is the deep circumflex iliac artery, which runs behind the lateral portion of the inguinal ligament. Any of these small arteries and especially their accompanying veins may be injured in creating the tunnel for the bypass graft. The resultant bleeding is annoying and increases the risk of infection. In addition, approximately 20% of patients have an obturator artery that arises from the inferior epigastric rather than from the internal iliac artery (Fig. 15-9 and see Fig. 19-21). This aberrant vessel descends across the pelvic end of the femoral canal and across the pectinate line of the pubis to reach the obturator canal. There is a potential for injury of this vessel during graft tunneling, a lesson learned from repair of femoral and inguinal hernias.
toward the umbilicus, penetrating the transversalis fascia below the arcuate line of the posterior rectus sheath to reach the lower third of the rectus abdominis muscle. Immediately after its origin, the inferior epigastric sends a small branch with the internal oblique fibers that form the cremasteric covering of the spermatic cord in the male. The second small branch of the terminal external iliac artery is the deep circumflex iliac artery, which runs behind the lateral portion of the inguinal ligament. Any of these small arteries and especially their accompanying veins may be injured in creating the tunnel for the bypass graft. The resultant bleeding is annoying and increases the risk of infection. In addition, approximately 20% of patients have an obturator artery that arises from the inferior epigastric rather than from the internal iliac artery (Fig. 15-9 and see Fig. 19-21). This aberrant vessel descends across the pelvic end of the femoral canal and across the pectinate line of the pubis to reach the obturator canal. There is a potential for injury of this vessel during graft tunneling, a lesson learned from repair of femoral and inguinal hernias.
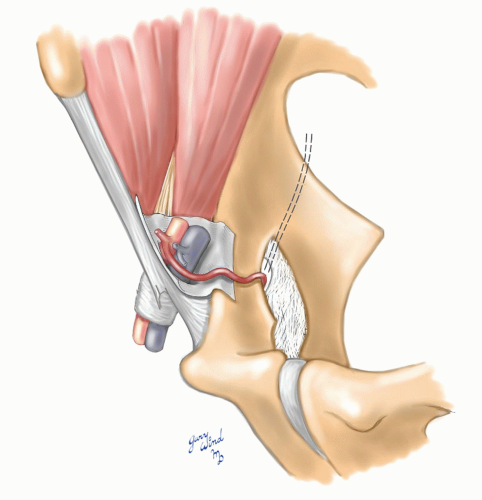 Fig. 15-9 A surgically treacherous origin of the obturator artery from the inferior epigastric artery is found in nearly one-fifth of individuals. |
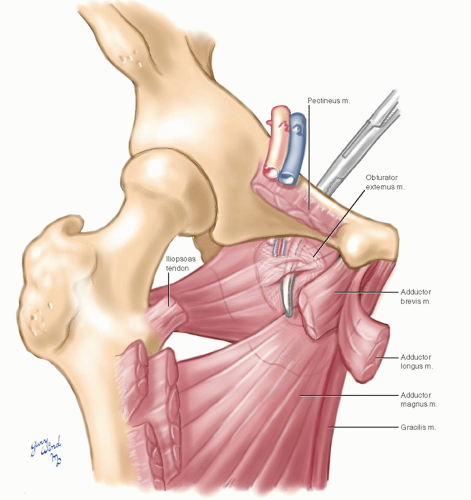
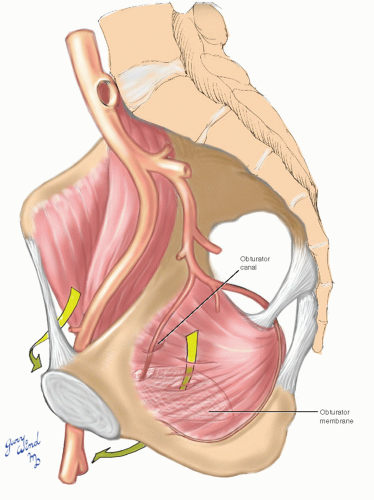
The floor of the femoral triangle beneath the femoral vessels consists of the pectineus muscle medially and the iliopsoas muscle arching over the anterior aspect of the hip joint laterally (see Fig. 15-1). The proximity of the underlying hip joint is demonstrated by the occasional joint infection after femoral arteriography when sterile technique is broken. Deep to the pectineus muscle lies the obturator foramen, covered by a dense membrane in all but its cephalad portion (Fig. 15-10).
The attachments of the adductor muscles around the bony margins of the obturator foramen form the rim of a cone, with the obturator membrane as its base. Within this cone, the obturator externus muscle has its broad origin from the lower part of the membrane, and the obturator nerve and vessels pass from the pelvis to the thigh through the more cephalad obturator canal. The obturator membrane provides an alternate route for bypass grafts to the femoral artery (Fig. 15-11).
The attachments of the adductor muscles around the bony margins of the obturator foramen form the rim of a cone, with the obturator membrane as its base. Within this cone, the obturator externus muscle has its broad origin from the lower part of the membrane, and the obturator nerve and vessels pass from the pelvis to the thigh through the more cephalad obturator canal. The obturator membrane provides an alternate route for bypass grafts to the femoral artery (Fig. 15-11).
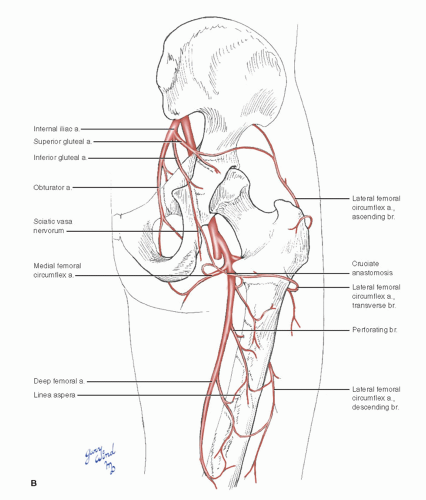
The common femoral artery crosses the pectineus muscle diagonally and divides into the superficial and deep femoral arteries. The deep femoral (profunda femoris) artery provides the majority of blood flow to the thigh muscles, supplemented by the obturator artery and descending branches of the superior and inferior gluteal arteries (Fig. 15-12). The superficial femoral artery reaches the inverted apex of the femoral triangle and then traverses the thigh in the adductor canal (Hunter’s canal) between the quadriceps and adductor muscles, giving off only minor muscular branches (see Fig. 15-4).
Near the adductor hiatus, the superficial femoral artery gives off the highest genicular artery that may assume importance as a collateral channel in femoral occlusive disease (see Chapter 17).
Near the adductor hiatus, the superficial femoral artery gives off the highest genicular artery that may assume importance as a collateral channel in femoral occlusive disease (see Chapter 17).
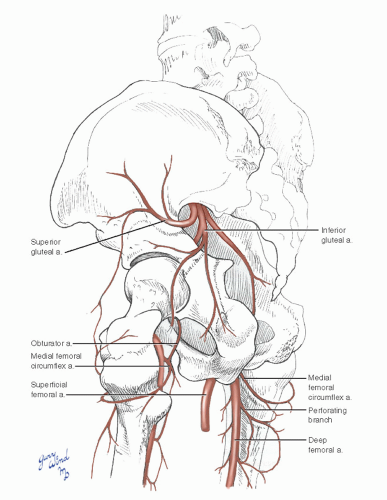 Fig. 15-12 Branches of the gluteal arteries and the obturator artery supplement the deep femoral in providing blood supply to the thigh. |
The common femoral artery gives off the small deep external pudendal artery before giving rise to the large deep femoral branch approximately 4 cm distal to the inguinal ligament. The deep femoral artery usually arises on the lateral side of the parent vessel. Shortly after its origin, the deep femoral artery gives rise to the lateral and medial femoral circumflex vessels (Fig. 15-13). Either of these vessels may less commonly arise from the common femoral artery and be confused with the deep femoral trunk.
Such variant branches must be identified to obtain control of this segment for anastomosis.
Such variant branches must be identified to obtain control of this segment for anastomosis.
The origin of the deep femoral artery is crossed by the lateral femoral circumflex vein (Fig. 15-14). Branches of the lateral femoral circumflex artery supply the proximal quadriceps muscle. The descending branch of the lateral femoral circumflex artery enters the substance of the vastus lateralis where it anastomoses with genicular collaterals. Branches of the medial femoral circumflex artery supply the proximal adductor compartment. These vessels anastomose with each other, with the inferior gluteal artery, and with the first perforating branch of the deep femoral artery.
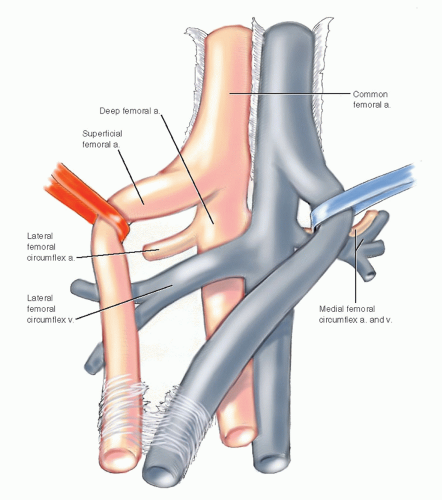 Fig. 15-14 The origin of the deep femoral artery is crossed by the lateral femoral circumflex vein that may be divided for exposure. |
The continuation of the deep femoral artery turns posteromedially toward the femur and enters the plane posterior to the adductor longus where it closely parallels the femoral shaft (Fig. 15-15A, B). It supplies the bodies of the adductor muscles and sends four perforating vessels through openings in the adductor brevis and magnus muscles. The first two branches usually perforate both muscles, whereas the lower branches penetrate only the tendinous attachment
of the adductor magnus muscle along the medial lip of the linea aspera of the femur. The last perforator is the termination of the deep femoral artery. The perforators anastomose with each other along the posterior side of the adductor magnus muscle and provide blood to the hamstring muscles of the flexor compartment. The second perforator usually provides a major nutrient vessel to the femur, and the distal perforators anastomose with branches of the popliteal artery.
of the adductor magnus muscle along the medial lip of the linea aspera of the femur. The last perforator is the termination of the deep femoral artery. The perforators anastomose with each other along the posterior side of the adductor magnus muscle and provide blood to the hamstring muscles of the flexor compartment. The second perforator usually provides a major nutrient vessel to the femur, and the distal perforators anastomose with branches of the popliteal artery.
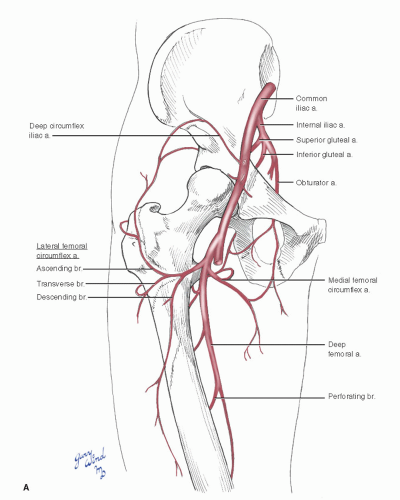 Fig. 15-15 A: Anterior view of the rich collateral circulation around the hip joint and proximal femur. |