The number and proportion of older individuals in the total population is increasing rapidly in the United States and other developed nations. There are a number of physiological and metabolic changes unique to aging that may affect clinical laboratory values. In addition, aging is often accompanied by multiple medical conditions requiring diverse medications, which can also affect clinical laboratory values. This chapter will summarize the issues that should be given special consideration with regard to clinical chemistry in the geriatric patient.
THE AGING OF AMERICA
The age structure of the United States population is currently undergoing a change, and based on this change, there is increased focus and emphasis on the older subset of individuals. The population older than 65 is projected to nearly double by the year 2050 to over 83.7 million.1 While in 2010, there were over 40 million individuals in the United States aged 65 years and older, which made up 13% of the population, the baby boomers began to turn 65 in 2011, which increased the percentage over the age of 65 to nearly 50 million in 2015. Not only is this the largest number of aged individuals and the largest percentage of the population ever reported in a US Census, this segment of the population is growing much more rapidly than the US population as a whole.
Aging of the “baby boomers,” individuals born during the post–World War II surge from 1946 to 1964, coupled with increased life expectancy, has had a significant impact on the population breakdown in the United States. In 2010, the average female was expected to live to 80.8 years, while the average male was expected to live to 75.7 years.2 Now it is estimated that one out of every three nursing home residents is an “Oldest Old Woman,” that is, over the age of 85 years.1 Further, approximately 10,000 boomers will turn 65 each day for the next two decades, more than doubling the number of Americans 65 years of age or older to 88.5 million by 2050.2 Figure 34.1, taken from the U.S. Census Bureau 2010: “65+ In the United States,” categorizes the age structure of the American population and the projected changes over the next 40 years. These changes are largely due to the aging of the baby boomers along with immigration trends.3 Complementary data from the 2010 census document illustrate and characterize the increase in the population numbers over the past 110 years.1 Depending on immigration, fertility, and longevity rates, these seniors are expected to constitute over 20% of the total US population by 2050 (Fig. 34.2).3,4 The total population over the age of 65 (Fig. 34.3) is expected to reach 19 million in the United States by 2050, almost 4.5% of the total population.3 With the burden of medical illness and medication use falling disproportionately on the elderly, a dramatic increase in the utilization of health care services, including clinical chemistry, is inevitable.
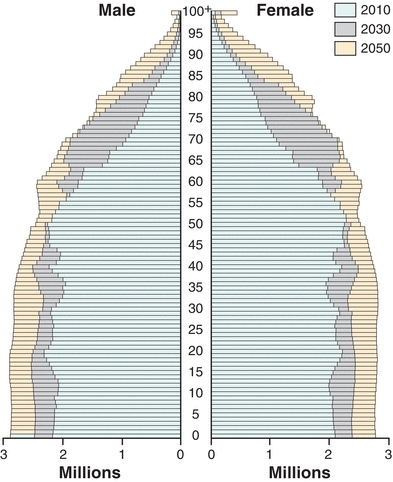
FIGURE 34.1 Data taken from the US Census Bureau 2008 display the age/gender structure of the population in this country and the projected changes that are expected to occur over the next 40 years. There is an anticipated shift in the age structure for the 13% of the population falling into the subclass of 65 or older. The distribution is expected to increase to nearly 20% by the year 2030.3 (Source: Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Washington, DC: US Census Bureau; 2008. http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed August 26, 2012.)
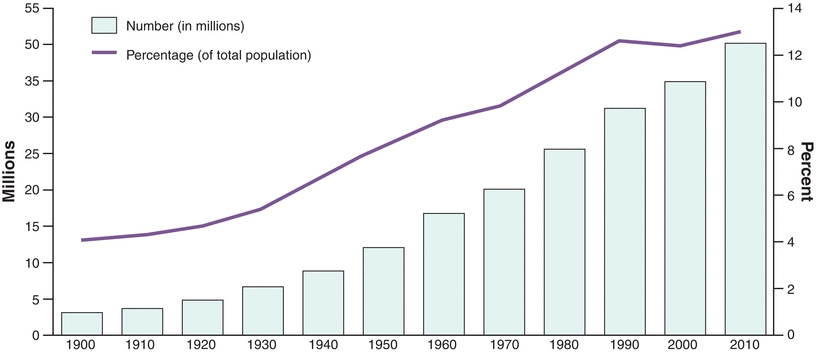
FIGURE 34.2 Population 65 years and older by size and percent of total population: 1900 to 2010. This figure shows the age growth over the past 110 years in the United States. Currently, over 40.3 million people are over age 65. This was an additional increase of 5.3 million over the numbers in the 2000 census. Additionally, the percentage of the population over age 65 has increased from 12.4% in 2000 to 13% in 2010. Further, the percentage of the US population greater than 85 years is expected to continue to increase, and in 2050, this age range is expected to make up over 20% of the US population. (Source: U.S. Census Bureau. Decennial census of population, 1900 to 2000. 2010 Census Summary File 1.)
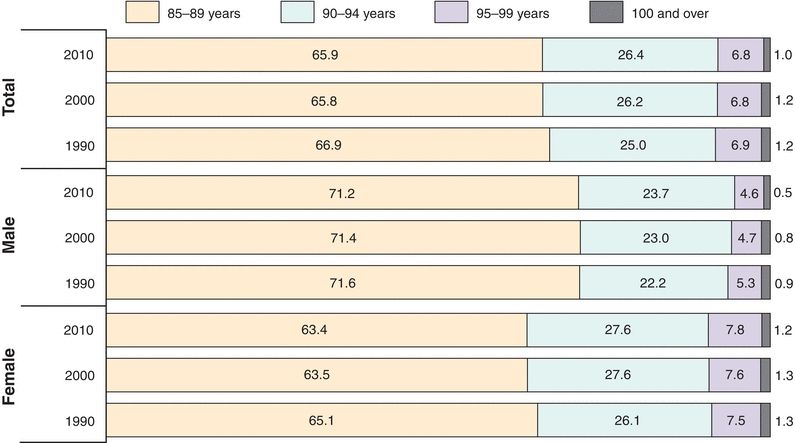
FIGURE 34.3 Projected population of Americans over the age of 65 by age and sex. The percent distribution of the population over the age of 85 is further broken down according to gender.3 The largest percentage increase during the previous 20 years was in the 90 to 94 year age group, which saw an increase of 1.4% between the years 1990 and 2010. Females contribute a larger percentage to the oldest-old calculation compared with the male data. (Source: U.S. Census Bureau. 1990 Census Summary File 2C, Census 2000 Summary File 1, and 2010 Summary File 1.)
AGING AND MEDICAL SCIENCE
Gerontology, the study of aging, and geriatrics, the subspecialty of clinical medicine that focuses on care of the aged, have much to tell us about normal aging, as well as the unique features of common illnesses in the elderly. The differentiation of “normal” or “healthy” aging versus the accumulation of multiple medical problems with age is an area of active research and debate. There are several analytical measurements that change when comparing a diseased individual to a healthy one, but because there are also a number of biochemical changes that occur as a consequence of normal aging, it can be difficult to differentiate between abnormal physiological changes and normal signs of aging in geriatric patients.
One important principle is that aging is extremely heterogeneous. The extent of differences between individuals of the same age is often quite significant. Indeed, an individual’s overall health status and expected longevity are more closely related to their functional status than their chronologic age. Thus, an 86-year-old jet-setting international attorney may look very unlike a 60-year-old nursing home patient bedbound with dementia. Older adults may also mistake a health symptom for a normal part of aging, and may not seek medical attention as early as they should.5
An important consideration is the concept of diminished physiological reserve. While an aged person usually has the same adaptive mechanisms to stress as a younger person, those adaptations may not be as rapid or as robust. Therefore, with diminished reserve, an aged individual may encounter adverse health effects much more quickly than a younger person. For example, an elderly person undergoing diuretic therapy for hypertension would not be able to withstand a long period of vomiting and diarrhea compared with a younger person. Age-associated decrease in total body water would favor dehydration and development of hypernatremia and delirium.6
While age-dependent changes in concentrations of analytes are shown to be important in a number of areas of chemistry, there are also several examples of chemistry values that are unchanged as a consequence of age.7 Table 34.1 outlines some of the age-specific changes that occur in regard to certain chemistry analytes, and some of these changes will be specifically addressed in the coming section outlining physiologic changes with age. Ideally, the changes that impact laboratory results would be classified in age-specific reference ranges, but since these are not readily available; changes in analyte level over time can help to manage patient treatment.7
TABLE 34.1 Changes in Selected Clinical Chemistry Analytes with Age8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
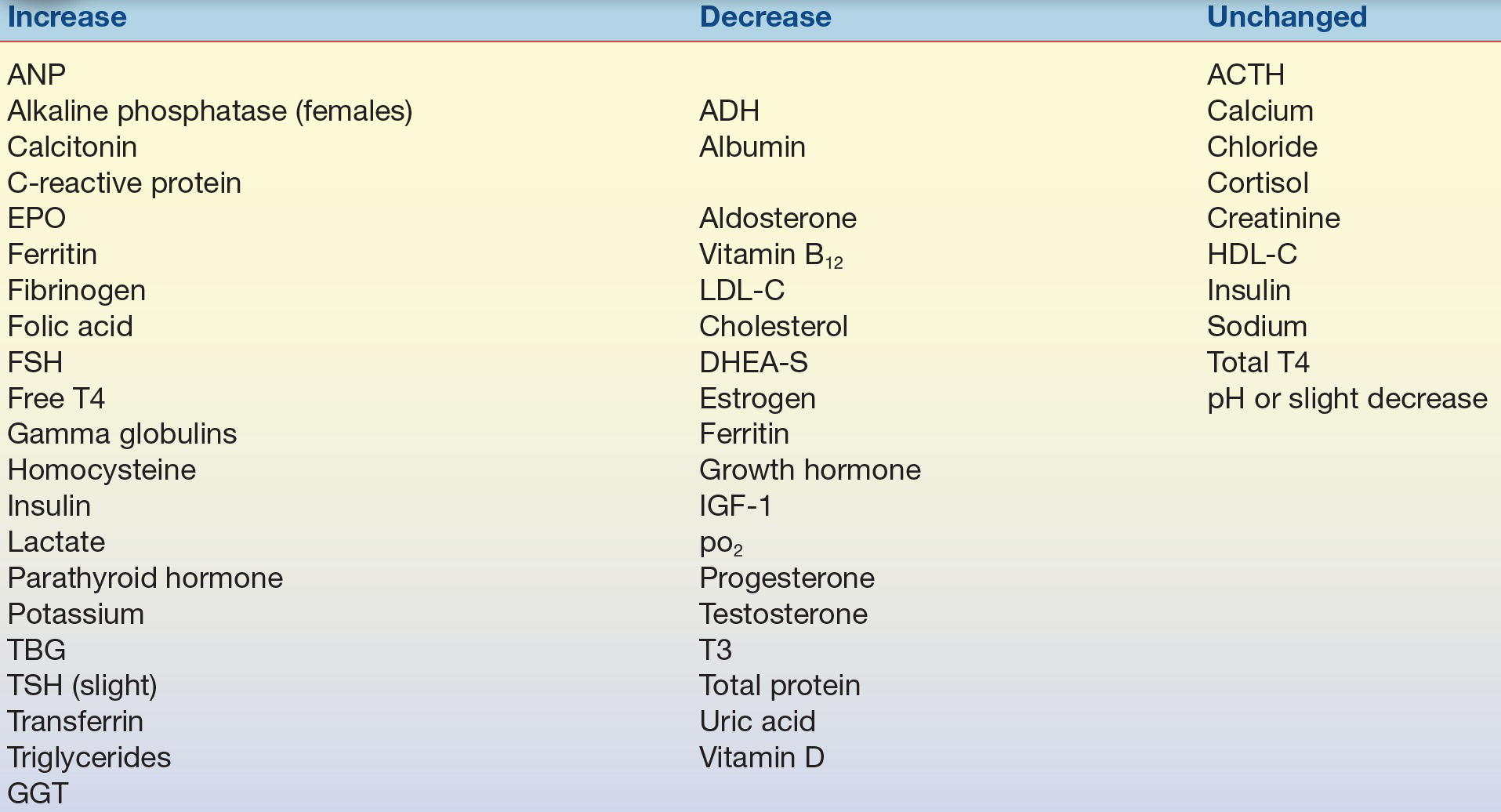
ANP, atrial natriuretic peptide; ACTH, adrenocorticotropic hormone; ADH, antidiuretic hormone; EPO, erythropoietin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FSH, follicle-stimulating hormone; DHEA-S, sulfated dehydroepiandrosterone; IGF-1, insulin-like growth factor-1; TBG, thyroid binding globulin; TSH, thyroid-stimulating hormone; GGT, Gamma-glutamyl transferase; T3, triiodothyronine.
GENERAL PHYSIOLOGIC CHANGES WITH AGING
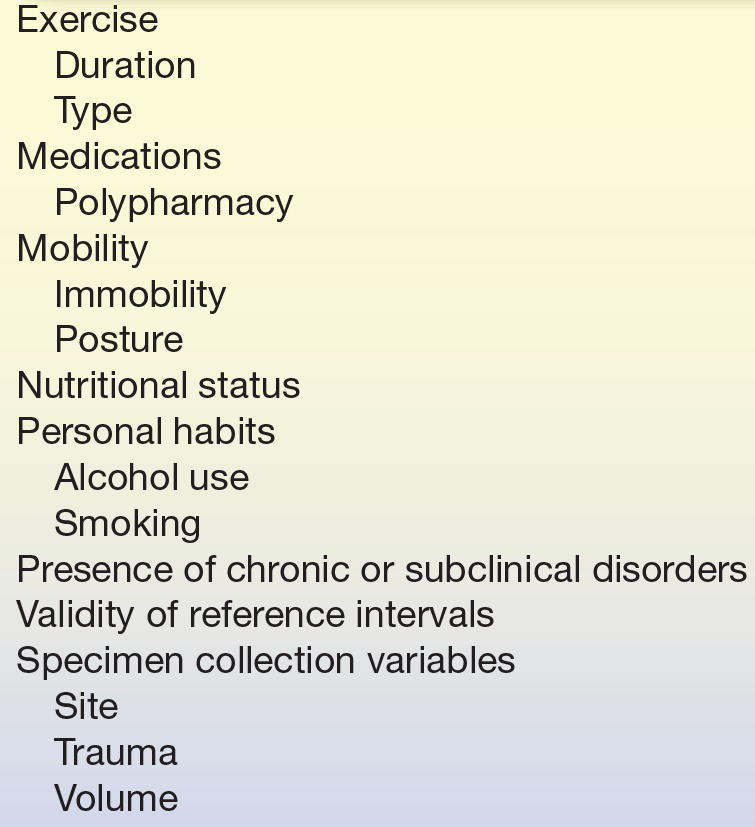
The aging process involves both biochemical and physiological changes and can be subdivided into various organ systems. The systems continue to function appropriately unless they are subjected to excess stress. With increasing age, an individuals’ ability to respond to stress decreases. This leads to an age-associated increase in the prevalence of pathological conditions. Table 34.2 outlines some of the more common factors impacting the interpretation of clinical laboratory results.
TABLE 34.2 Factors Impacting Interpretation of Clinical Laboratory Results for the Elderly5,19,20,29, 30, 31, 32, 33, 34
Muscle
Total body muscle mass typically decreases with age, but the rate and extent of loss have a strong genetic component. This age-related decline (sarcopenia) results in a decrease in lean body mass and a decrease in total creatinine production, such that serum creatinine is no longer reliable for assessment of renal function in the aged.8
Bone
Total bone density and mass decreases with age in both men and women, though the changes are much more dramatic in women after menopause.9 Serum calcitonin levels typically rise with age, but ionized calcium levels remain stable.10 Parathyroid hormone (PTH) levels increase in postmenopausal women, and this increase is associated with changes in bone metabolism.11
Gastrointestinal System
The incidence of atrophic gastritis increases with age, with a consequent increase in vitamin B12 deficiency from poor absorption.12 The incidence of achlorhydria (low or absent gastric acid production) also increases with age, which can result in decreased calcium and iron absorption, as well as an increased incidence of bacterial overgrowth in the small intestine.13 Albumin levels decrease, and the incidence of malnutrition, leading to higher mortality rates, also increases.35
Kidney/Urinary System
The number of functional glomeruli decreases with age, resulting in a decrease in kidney size and weight. Glomerular filtration rate (GFR) declines, and renal blood flow is even more reduced, such that filtration fraction (GFR/renal plasma flow) actually increases.15 Additionally, the kidney’s concentrating ability declines. The result of all these changes is that acid/base, water, and electrolyte levels remain normal under optimal conditions, but physiologic reserve is diminished. The secretion of erythropoietin (EPO), the glycoprotein hormone that controls red blood cell production, increases with age, and the level of serum renin, an enzyme that regulates blood pressure, decreases. Renal responsiveness to atrial natriuretic peptide (ANP) decreases, and serum levels of ANP and brain natriuretic peptide increase with age.16,36 Structural, neurological, and immune changes result in an increased incidence of urinary tract infection in the elderly, especially in women.17
CASE STUDY 34.1
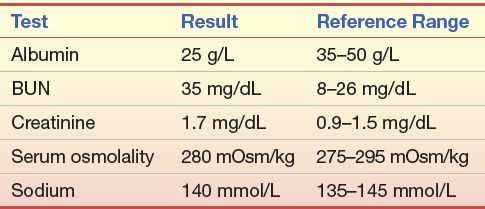
A healthy 65-year-old man entered the hospital to have his appendix removed. Preoperative laboratory results are shown in Case Study Table 34.1.1.
CASE STUDY TABLE 34.1.1 Laboratory Results
Question
1. What is the BUN/Creatinine ratio for this patient?
2. What do these data suggest?
3. Which test results support this conclusion?
Immune System
The thymus shrinks with age, causing a decrease in thymosin levels and T-cell function. B-cell function slowly declines, as well, such that cellular and humoral immune responses are less vigorous and slower in the aged than in younger individuals.18 Autoimmune antibody (antinuclear antibody [ANA]) levels increase,37 and hematopoietic stem cell numbers decrease.38 Examples of the consequences of declining cellular immunity in the elderly include reactivation of latent tuberculosis and herpes varicella zoster (HVZ) virus. HVZ is the virus responsible for the chicken pox, but in an adult, reactivation is termed shingles and presents as a painful, blistering skin rash. The prevalence of shingles in the United States is about a million cases per year, and susceptibility to shingles increases at the age of 50 years. This increase has led to the development of a live vaccine for elderly adults.39
Endocrine System
Serum adrenocorticotropic hormone and cortisol levels typically do not change with age, though response to stress may be delayed. Pulsatile secretion of growth hormone (GH) typically diminishes with age, resulting in a decrease in lean body mass/fat ratio, as well as loss of overall body mass. The peak but not the basal levels of melatonin secretion decrease with age, which may contribute to sleep cycle disorders as well as diminished protection from free radicals.40 Norepinephrine secretion generally increases, which contributes to systemic vasoconstriction and decrease in myocardial relaxation; epinephrine levels remain stable. Aldosterone levels may decline, which can contribute to orthostatic hypotension, or a drop in blood pressure upon standing.41 Thyroid hormone levels are typically well preserved or slightly increased into very old age.42,43
Sex Hormones
Although menopause in women typically occurs prior to the earliest ages considered “geriatric,” the reduction in gonadal production of estrogen and progesterone and secondary increase in hypothalamic gonadotropin-releasing hormone persist through the remainder of a woman’s life.44 Testosterone levels in men typically exhibit a gradual decrease with increasing age—the term “andropause” has been used to describe this observation in analogy to menopause, but the decline in serum levels of sex hormone is not abrupt and not as significant in degree for men as it is for women. The distinction between a normal serum testosterone level for age and hypogonadism in an aged man is a point of some contention and includes consideration of sexual function, general perception of well-being by the individual, and other clinical factors in addition to the value of the serum testosterone level.45 Dehydroepiandrosterone (DHEA), sulfated DHEA, and pregnenolone all decrease with age.
Glucose Metabolism
Insulin secretion is unchanged, though there are age-related changes at the cellular level in insulin signalling, receptors, and glucose transporters. An individual with the genetic predisposition to type II diabetes mellitus is more likely to manifest clinical illness with increasing age, body mass index, and lack of exercise. The combination of an aging population, increasing obesity, and an increasing number of individuals from racial/ethnic groups at increased risk of diabetes (African American, Hispanic American, American Indian) has resulted in a dramatic increase in the number of older adults with diabetes.46 Many of these individuals will also suffer some of the consequences of diabetes, including damage to the eyes, kidneys, nerves, and blood vessels.
EFFECTS OF AGE ON LABORATORY TESTING
Basic biochemical and physiological changes accompany the aging process, and these changes can impact an individual’s clinical laboratory test results. It is important that laboratorians understand how these changes can impact specific tests. It has been suggested that the presence of age-specific changes may warrant separate reference intervals for the elderly,43,47 but these are not readily available. In addition, consideration of preanalytical variables must be factored into the interpretation of laboratory results. How does the aging process affect interpretations of drug levels in the elderly? What are the effects of exercise and nutrition on chemistry results? Table 34.3 describes some of the factors that laboratorians should consider when interpreting test results for the elderly and defines some of the laboratory values that are impacted by these changes.
TABLE 34.3 Effects of Age on Laboratory Testing9,16,18,36,37,42, 43, 44, 45,48, 49, 50, 51, 52, 53, 54, 55
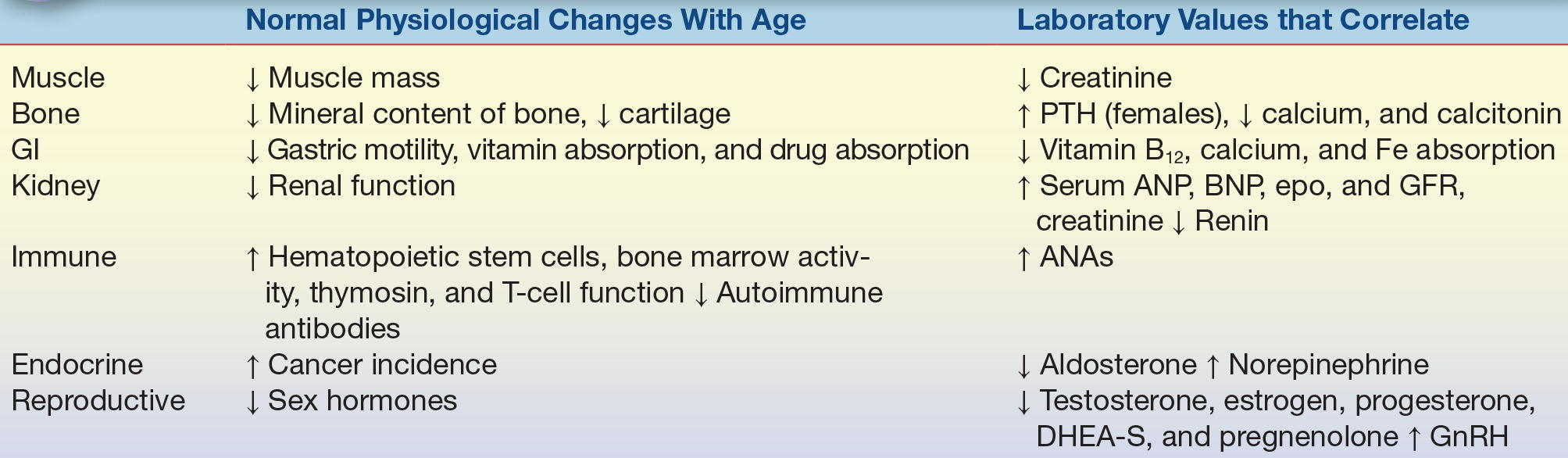
PTH, parathyroid hormone; GI, gastrointestinal; ANP, atrial natriuretic peptide; BNP, brain natriuretic peptide; EPO, erythropoietin; GFR, glomerular filtration rate; ANA, antinuclear antibody; DHEA-S, sulfated dehydroepiandrosterone; GnRH, gonadotropin-releasing hormone.
Muscle
As muscles age, they begin to decrease in number and size. Creatinine levels correlate with both muscle mass and renal function. In the geriatric population, a decrease in muscle mass coupled with the decrease in renal function keeps the creatinine level nearly the same or slightly increased.
Bone
Adequate calcium intake and sufficient vitamin D are important in maintaining bone mass and density. Osteoporosis incidence is high in the elderly population, and this leads to increased risk of fracture. In addition, osteoporosis incidence coincides with increased risk of vitamin D deficiency. Vitamin D helps with absorption of dietary calcium from the intestine, thus decreased vitamin D levels can decrease the amount of dietary calcium that is absorbed. Inadequate calcium absorption may eventually lead to low serum calcium levels and increased PTH levels. This increased PTH then causes increased calcium loss from the bone, which increases alkaline phosphatase levels.19
Gastrointestinal System
The gastrointestinal system includes the digestive tract and accessory organs including the pancreas and the liver. There are a number of age-related changes with respect to the liver analytes. C-reactive protein, an acute phase reactant, has been shown to be elevated in the elderly.56 This elevation is thought to be a nonspecific indicator of inflammation and typically is a poor prognostic indicator.29 Gamma-glutamyl transferase (GGT) levels tend to increase with age in a gender-specific manner. Men do not show this age-related increase, but men tend to have higher levels of GGT than women. Fibrinogen, an acute phase reactant, is frequently elevated in geriatric patients, and this increase coincides with inflammatory disease, stroke, coronary dysfunction, and cancer.20,30
CASE STUDY 34.2
A healthy 70-year-old woman is seen by her primary care physician for an annual checkup. She complains of muscle weakness, drowsiness and confusion. Her laboratory results are shown in Case Study Table 34.2.1.
CASE STUDY TABLE 34.2.1Laboratory Results
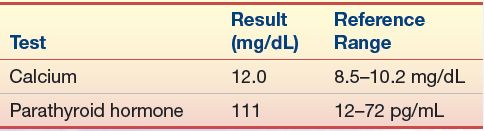
Questions
1. Based on the laboratory data, how might the PTH test be interpreted?
2. Should any additional testing be done?
Ferritin levels can be low in the elderly population, and when this is seen, it is usually due to iron deficiency anemia, similar to younger people. Transferrin levels can be reduced due to iron-deficient anemia or as a result of acute or chronic stress. Albumin levels are frequently decreased in the elderly population as a result of inflammation, malnutrition, and liver disease. Levels can be high in dehydration, but elevations above the upper limits of normal rarely occur in the elderly due to the prevalence of other health conditions that mask alterations.21 Total protein levels are also frequently decreased in the elderly for the same reasons that albumin levels are low.
Urinary System
Serum creatinine levels are thought to be lower in the elderly due to decreased muscle mass. At the same time, a reduction in glomeruli filtration rate can offset this decrease.
Immune System
As age increases, infection-induced morbidity and mortality rise. This is in part due to a weakened immune system. The innate immune system, commonly referred to as the “first line of defense,” is the nonspecific antigen activation that confers short-term protection from a pathogen. Adaptive immune system, on the other hand, is activated by the innate system and refers to the protection from antigen that an individual develops throughout the life. Both the innate and adaptive immune systems become damaged and dysfunctional as individuals age, leading to increased prevalence of infection, and potentially also autoimmune disease and cancer.57 Gastroenteritis is more frequently observed as individuals’ age, but the increased frequency is thought to be a result of a weakened immune system.22 Pathogenic bacteria can enter and infect the digestive tract and contribute to presentation. Additionally, there is an increase in ANA production, which correlates with incidence of arthritis and many other autoimmune disorders.31
Endocrine System
There are a variety of age-related changes to endocrine hormone regulation. These can be subclassified according to whether the hormone level increases or decreases.
Increased Hormone Level
Elevated levels of cortisol, though rarely present, have been reported to be associated with decreased cognitive function and memory loss.48 A slight increase in thyroid-stimulating hormone (TSH) has been observed but is not profound.42,43 Follicle-stimulating hormone (FSH) levels increase with aging, but with this increase, there is a down-regulation of FSH receptors, such that in menopause, there are no longer circulating cells with FSH receptors and thus no responsiveness to the high level of hormone. ANP levels increase with age, and the levels have been shown to be nearly fourfold higher in healthy elderly individuals than in younger people.49 Anemia is common in the elderly population, and EPO, a marker for anemia, rises in elderly patients.23 PTH levels are slightly higher in older individuals than gender-matched pairs.50
Decreased Hormone Level
In contrast to the finding with cortisol, DHEA levels have been shown to decrease by 40% to 60%.24 Estrogen and progesterone levels decrease with age, and the reduction in estrogen further up-regulates FSH levels. Insulin-like growth factor (IGF-1) and GH levels decrease with age. Secretion rates and serum concentrations of aldosterone decrease with age as a consequence of a decreased level of renin.51,58 Pituitary function declines with age, and hypothalamic antidiuretic hormone (ADH) levels are increased.
Sex Hormones
Levels of expression of all sex hormones diminish with age. Testosterone levels decrease with age, as do estrogen and progesterone levels.45
Glucose Metabolism
Insulin sensitivity decreases with age. As a result of this decreased sensitivity, there is an increase in the prevalence of type 2 diabetes, with the incidence reaching a peak between the ages of 60 and 74.59
ESTABLISHING REFERENCE INTERVALS FOR THE ELDERLY
Most laboratory tests have “gender-specific” reference ranges and/or “age-specific” reference ranges. The broad categories for the age ranges are very wide, and the adult reference range includes individuals between 18 and about 50 years. As people live longer, age-related criteria for the analysis and interpretation of test results become increasingly important. Because of the need to establish reference ranges in a healthy population, and the increased prevalence of at least one health condition in the aged, there are little data on more appropriate age-specific reference ranges for older adults. Based on this lack of data, there has been an increased interest in determining age-related reference ranges in order to more effectively identify individuals with early stage disease.52,60,61 While the idea has a lot of merit, there are only a few publications establishing age-appropriate reference ranges for the elderly.62 Laboratories should consult the current literature for latest age-related reference ranges.
Certain analyte fluctuations that are seen as individual’s age are clearly the result of aging organs, but other analytes do not lend themselves to such apparent delineation.63 In addition, coincident medical conditions can further complicate the issue. The requirement that reference values be obtained from healthy, normal individuals unfortunately limits a large number of geriatric patients from contributing to establishing these references. Recently, a strategy for reference interval data mining has been introduced to expand on age-appropriate reference intervals for all age groups.64 Prior to this approach, the use of exclusion criteria caused the geriatric population to be vastly underrepresented in most randomized clinical trials, which further limited the validity of age-specific reference range generation.65 In addition, there is a wide intraindividual variability among the various analytes, which has been seen as a major obstacle for determining age-appropriate reference ranges among the elderly. Instead, the current clinical approach that has been increasingly implemented is careful documentation of laboratory values and paying closer attention to changes over time instead of where the values fit in with the remainder of the population. This is not feasible among all elderly, as there is a small subset that resists treatment and thus does not see a medical professional on a regular basis.66 A lack of baseline measurements coupled with the lack of age-specific reference ranges continues to make diagnosis challenging. Currently, most physicians who care for the geriatric patient population rely on established patient care, frequent routine examinations, and following changes in laboratory values over time as an early indicator of a problem.
PREANALYTICAL VARIABLES UNIQUE TO GERIATRIC PATIENTS
There are a number of factors that contribute to the accuracy and validity of test results in any population, but several of these factors have a greater impact in the geriatric patient. These include sample collection, sample handing, and physiological variables. Geriatric patients can present a challenge to phlebotomists due to disease, malnutrition, or dehydration.67 With increased age, there is a reduction in healing rate and an increased risk of acquiring infection due in part to a gradual loss in the capacity of the immune system to fight off infections.68 Further, the skin and veins are less elastic and can be injured more easily during venipuncture. The decrease in muscle mass and collagen leads to a decrease in vascular stability of veins and a subsequent decrease in blood flow. Physiological changes in the patient may impact laboratory results due to unavoidable issues that arise at the time of collection. Increased hemolysis or insufficient volume can ultimately impact the validity of the result. Other factors that may influence normal laboratory values in geriatric patients include diet, medications, exercise, smoking, alcohol consumption, physical activity, and body composition. While these factors influence results independent of age, geriatric patients are more likely to have one or several of these causing variations in test results. Caution should always be exercised when reporting results in a geriatric patient, but clearly an absurd result (one not compatible with life) should be investigated to identify potential causes of the discrepancy.
DISEASES PREVALENT IN THE ELDERLY
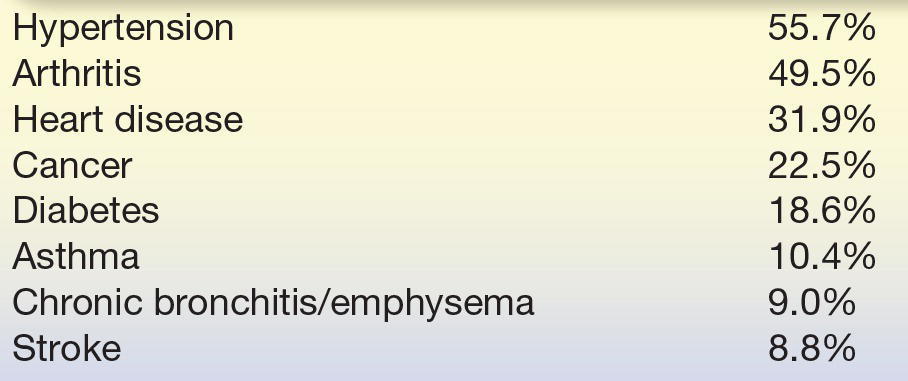
There are many diseases that are especially common in the elderly. Table 34.4 outlines the prevalence of some of these conditions in Americans 65 years and older as reported in the 2007 to 2008 National Health Interview Survey, a self-reported statistically valid sample of the US population.69 The overall prevalence of these diseases is inadequately understood due to poor documentation and the presence of multiple conditions warranting many medications. There have been attempts to classify disease prevalence in the elderly population based upon pharmacy databases.70 Classification in this population has been difficult due to inaccuracies related to misidentification of conditions or diseases, or incomplete medical records. Approaches to classify individuals at an earlier stage of disease have led clinicians and laboratorians to analyze drug combination therapies as markers of disease. A list of drugs that patients are prescribed is available in a pharmacy database, from which statistics can be generated calculating nationwide averages for disease prevalence.
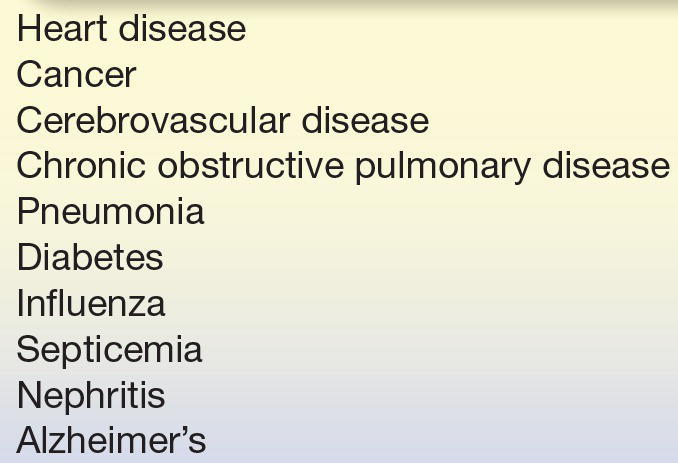
The majority of the diseases noted in Table 34.5 are degenerative conditions, leading to concerns that increased life expectancy will increase the number of years with declining health. Health is defined as the state of being free from illness or injury, and deteriorating health is the number one reason that elderly leave their homes and enter retirement facilities.72 Unfortunately, without baseline measurement, it can be difficult to identify noteworthy changes in analyte levels.
Menopause is defined as the time when the primary function of the human ovaries is permanently terminated. This time is variable for each individual, but typically, it begins between the ages of 35 and 58 years. This wide age range is based in part on the fact that functional disorders affecting the reproductive system can speed the transition to menopause. For instance, women with cancer of the reproductive tract, polycystic ovary syndrome, or endometriosis typically transition to menopause earlier than women without these conditions.73, 74, 75 The precise definition of menopause is lack of menses for greater than 1 year. This transitional phase from reproductive to nonreproductive typically lasts about a year to a year and a half, and during this period of time, there is a gradual decline in ovarian function, thus a decrease in ovarian hormone production.75 The changes that occur are caused by reduced estrogen levels that result from loss of the granulosa and interstitial cells lining the follicles.76 The placenta normally produces hCG during pregnancy, but in addition to placental production, hCG can also arise from the pituitary. In perimenopausal women, hCG levels are often detected in the absence of pregnancy as a result of ovarian failure.53 Pituitary hCG is more commonly detected in women ≥55 years, and marked elevations in this age group are most commonly associated with cancer.77
Osteoporosis, a bone disease that is prevalent in the elderly, leads to increased risk of bone fracture. Two types of tissue form bone, compact and spongy (trabecular). Compact bone accounts for 80% of the total bone mass of an adult, while trabecular bone accounts for the remaining 20%. Trabecular bone is highly porous (30% to 90%), while compact bone has a porosity of 5% to 30%. The risk of fracture is highest in bones with more compact tissue, which functions in whole body support. Bone mineral density (BMD) is reduced with age, and the World Health Organization has defined osteoporosis as BMD 2.5 standard deviations below peak bone mass.78 This decreased density and an observed reduction in a number of bone-associated proteins both contribute to the weakened condition. Classifications of osteoporosis include primary type 1, primary type 2, and secondary (also known as type 3).79 While primary type 1 is more frequently seen in elderly females, there is a growing precedence of osteoporosis in men. Secondary osteoporosis occurs in women or men who are older than 70 years of age and is typically associated with decreased bone formation and decreased renal production of dihydroxy vitamin D. Vitamin D deficiency causes decreased calcium absorption, which increases the PTH levels and promotes calcium mobilization from the bones, sacrificing skeletal calcium in order to maintain normal serum calcium levels. Type 3 osteoporosis is the only form of osteoporosis that affects individuals of any age. Most cases of type 3 osteoporosis are due to drug treatment or medication use, such as steroids,80 and type 3 is not common in the elderly. Laboratory testing surrounding osteoporosis includes monitoring serum calcium, phosphate, creatinine, alkaline phosphatase, and 25-hydroxy vitamin D, and in men, testing also includes testosterone.81
Dementia is a syndrome defined as impairment of memory and at least one other cognitive domain (language, perceptual skills, attention, constructive abilities, orientation, and problem solving) that is severe enough to significantly impair day-to-day function.82 Dementia is common in the elderly—approximately 10% of individuals over 65 years suffer from the syndrome; this rises to as high as 50% of those over 85 years.83 Mild cognitive impairment (MCI) is a term used to describe similar cognitive problems that are not severe enough to significantly impair day-to-day function, but between 6% and 25% of individuals with MCI will go on to develop dementia in 1 year.
Dementia can be described in a number of ways, including the area of the brain that is most affected (cortical vs. subcortical), whether the etiology is known or unknown (secondary vs. primary), age of onset (presenile vs. senile), or by clinical syndrome. Many types of dementia can only be definitively diagnosed by pathological examination of brain tissue, which is obviously not helpful to the individual suffering from the illness, and correlation between the clinical syndromes and pathologic findings has historically been fairly poor. Recent advances in imaging and neurochemistry have improved this somewhat.84 Conditions of cognitive impairment are largely clinical assessments and do not involve chemistry measurement in most cases. This is an opportunity for additional research as there are few proteins associated with these medical conditions (indicated below), and the data are not as terribly strong.
Alzheimer’s disease (AD) is the most common form of dementia, responsible for approximately 70% of cases.83 The pathologic findings of AD include amyloid plaques (made of beta amyloid) and neurofibrillary tangles (made of tau protein). Individuals with AD typically have a fairly slow but steady progression of impairment.
Vascular dementia is the second most common form of dementia and may be caused either by multiple clinically evident strokes (multi-infarct dementia) or by ischemic changes in the deep white matter of the brain. Individuals with vascular dementia typically have a “stuttering” or “stair-step” progression of impairment, but the speed of progression and specific manifestations may vary widely, depending on which areas of the brain are damaged.71,84,85
Dementia with Lewy bodies (DLB) is the third most common form of dementia and is characterized by prominent visual hallucinations, significant fluctuations in mental status, and parkinsonism (motor symptoms similar to those of Parkinson’s disease). Lewy bodies are collections of alpha-synuclein protein inside neurons, but whether they are a cause or an effect of the illness is unclear, and Lewy bodies are also seen in Parkinson’s disease, as well as in some cases of Alzheimer’s. DLB typically progresses more quickly than AD.
There are also less common types of dementia including Pick’s disease, frontotemporal dementia, Creutzfeldt-Jakob disease, normal pressure hydrocephalus, Huntington’s disease, and Wernicke-Korsakoff syndrome. Typically, diagnosis of dementia is based on the patient’s history and physical examination. Brain imaging and clinical laboratory testing may be performed to confirm or eliminate suspicion of specific clinical abnormalities.86
AGE-ASSOCIATED CHANGES IN DRUG METABOLISM
As adults age, changes occur that impact how the body metabolizes and utilizes drug compounds. Absorption, distribution, metabolism, and excretion of the drugs are impacted by the normal aging process. The prevalence of multiple health conditions in this subset of the population has highlighted the issue of polypharmacy32 and the importance of therapeutic drug monitoring. Such testing in the laboratory helps prevent overdose and adverse drug reactions. Calculation of the actual in situ drug level is a key factor when looking at the result and metabolic rate, and elimination of these compounds needs to be considered for optimal dosing.87
Absorption
The rate of drug absorption from the small intestine slows with aging, leading to a lower peak serum concentration and a decrease in the time to reach peak. Typically, the total amount of drug absorbed (bioavailability) is the same in younger and older patients.88 An exception arises due to an age-related decrease in hepatic function. Drugs that undergo extensive first-pass metabolism (such as nitrates) tend to have greater serum concentrations or greater bioavailability than drugs involved in conjugation or acetylation reactions.
Varying disease states or other drugs administered concurrently to the elderly may also cause changes in absorption. For example, calcium carbonate is frequently recommended for bone health in the elderly. This calcium salt requires gastric acid for absorption and should therefore be taken with food to stimulate gastric acid secretion. Patients with achlorhydria from natural causes or from acid-suppressing medications such as proton pump inhibitors or H2 blockers should instead take calcium citrate, the absorption of which does not require gastric acid.89
Distribution
Volume of distribution (Vd) is the volume of plasma into which a fixed concentration of drug is dissolved. The larger the Vd, the greater the distribution of the compound. Older adults typically have less body water and lean body mass as a percent of total body mass—or in other words have more fat as a percent of total body mass. Drugs such as ethanol and lithium that are water soluble (hydrophilic) have a lower Vd in the elderly. Highly water-soluble drugs tend to be more concentrated in elderly individuals due to decreased body water. Additionally, drugs such as benzodiazepines and barbiturates that are fat soluble (lipophilic) have higher Vd in the elderly due to increased body fat and decreased lean body mass.90 The extent to which a drug binds to plasma proteins also impacts its Vd. Many drugs bind to albumin, which is often decreased in the elderly. The unbound (free) portion of the drug is the pharmacologically active portion, and many drug assays measure total (bound and unbound) drug concentrations. Elderly patients with “normal” total drug levels may have excessive levels of free drug and exhibit signs of toxicity due in part to decreased albumin levels. Digoxin and phenytoin are examples of drugs that are significantly protein bound91—geriatricians will typically aim for the low end of the therapeutic range because of this issue.92
Metabolism
The liver is responsible for the majority of drug metabolism, and both hepatic blood flow and hepatic mass decrease with age. Phase I pathways of drug metabolism (hydroxylation, oxidation, dealkylation, and reduction) result in metabolites that may be of lesser, equal, or greater pharmacologic effect than the parent drug. In contrast, phase II pathways (glucuronidation, conjugation, or acetylation) result in inactive metabolites. Therefore, drugs metabolized by phase II pathways are generally preferred for the elderly because of decreased incidence of toxicity—for example, lorazepam is preferred over diazepam when benzodiazepine therapy is required in the elderly. The half-life of diazepam is extremely long, and as a result of this prolonged half-life, its metabolites accumulate to unexpectedly high levels in the elderly with repeated dosing. Because of this, lorazepam is preferred in this patient population.93
Elimination
Kidney mass and blood flow decrease with age, which results in gradual decline in GFR. Figure 34.4 graphically represents this gradual, age-related decline over time. Further, the current estimates of the prevalence of chronic kidney disease in individuals over age 60 years are nearly 40%.92,93 This decrease in GFR impairs elimination of therapeutic drugs and increases toxicity and adverse outcomes.94,95 Therapeutic drug monitoring is an important consideration to ensure that compounds ingested are being metabolized and excreted appropriately. The gold standard for determining GFR is a measurement of iothalamate or iohexol measurement following intake. Another means of determining GFR is the measurement of creatinine in a 24-hour urine sample, though measurement of creatinine in a random serum sample is more commonly tested due to ease of collection. A number of formulas exist to calculate GFR, and no formula is ideal for all patient populations. The three equations used to estimate renal function are the Modification of Diet in Renal Disease (MDRD) equation, the Cockcroft-Gault equation (CG), and the Chronic Kidney Disease Epidemiology Collaboration equation (CKD EPI).94, 95, 96 All three formulas use serum creatinine levels in combination with other factors to estimate GFR. The Food and Drug Administration traditionally uses the CG equation in its recommendations on appropriate dosing of therapies.97 Most clinical laboratories estimate renal function using the MDRD equation because this equation requires serum creatinine, age, race, and gender, but not weight. There is growing movement based upon current recommendations to use the CKD-EPI equation, which uses serum creatinine, age, race, and gender. There is also interest in incorporating cystatin C as well as creatinine in an estimating equation. There have been studies to assess the best equation for different demographics and patient populations. The findings of these studies have been contradictory, and based on the mixed results, there is no consensus equation used in the elderly patient population.98,99 Different GFR results can change the dose of drug administered, and thus, there has been effort to find alternate methods to achieve the best estimation of GFR. There have been various methods proposed and tested, but eGFR measurement has been widely incorporated into clinical laboratory testing. Creatinine measurement alone should not be used to assess renal function.
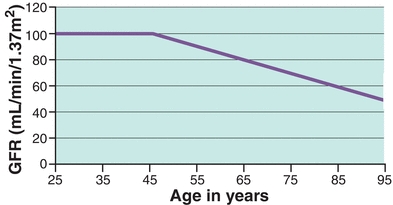
FIGURE 34.4 Rate of GFR decline in normal individuals with age. The course of GFR decline with normal aging was based on a cross-sectional study of iothalamate clearance in patients aged 17 to 70 years.116 (Modified from Hebert L, Cody R, Slivka A, Sedmak D. Hypertension-induced kidney, heart, and central nervous system disease. In: Mandal AK, Jennette JC, eds. Diagnosis and Management of Renal Disease and Hypertension. 2nd ed. Durham NC: Carolina Medical Press; 1994.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree