Renal cell carcinoma (RCC)
Benign
Clear cell RCC
Oncocytoma
Multilocular cystic RCC
Papillary adenoma
Papillary RCC
Metanephric adenoma
Chromophobe RCC
Angiomyolipoma
Collecting duct RCC
Epithelioid AML
Medullary carcinoma
Cystic nephroma
RCC, unclassified type
Mixed epithelial andstromal tumor
Clear cell papillary RCCa
Xp11 translocation associated RCCa
Mucinous tubular and spindle cell carcinomaa
Tubulocystic carcinomaa
Thyroid-like follicular carcinomaa
Grading of Renal Cell Carcinoma
The first major study on RCC grading was published in 1932 by Drs. Hand and Broder from the Mayo Clinic . Their grading system was based on nuclear features and correlated with patient outcome. Since that time, three notable studies addressing RCC grading have been published, and with the exception of the 2012 ISUP consensus conference grading system, all were reported prior to the Heidelberg and Rochester classifications. The work by Skinner et al. is of particular note as these authors analyzed their experience with a large cohort of surgically treated patients and found that a four-tier nuclear grading system based on the worst grade of a tumor stratified patients into four prognostic groups [4]. The 309 patients in their series treated by nephrectomy and with at least 5 years follow-up had 5-year survival for grades 1, 2, 3, and 4 of 75, 65, 56, and 26 %, respectively. Skinner et al. also reported for the first time that grade remained prognostic within the various RCC stages (Robson) including advanced stages. The authors also realized at that time that little was known of the various types of RCC, and divided tumors into clear cell, clear cell or granular, and spindle cell types. Subsequently, the most cited paper on RCC grading was published by Fuhrman et al. in 1982 [5]. Their study consisted of 103 patients, 84 treated by nephrectomy and with at least 5 years of follow-up. The grading system had four tiers and was based on nuclear features (size, shape, nucleoli) and the highest grade within a tumor was designated as the overall grade identical to Skinner et al . Fuhrman et al. made the additional observation of nucleolar size evident at various microscopic magnifications as an additional objective measure of nuclear grade. In their survival analysis, only three groups that differed in outcome were identified. Fuhrman grade 1 tumors had a survival of 65 % compared to grades 2 and 3 at 30 % and grade 4 at less than 10 %. Prior to 2012, the Fuhrman grading system was recommended for clinical use .
Shortcomings in the Fuhrman grading system have been well documented, and in 2012, a consensus conference of the ISUP developed grading system recommendations that were specific to the classification of RCC. Studies examining the prognostic impact of grade on outcome have been limited to clear cell, papillary, and chromophobe RCC as the other RCC types are too infrequent to analyze or have a relatively defined clinical behavior. In clear cell and papillary RCC , the ISUP recommended that the grade is determined exclusively by nucleolar prominence in grades 1–3, that grade 4 includes pleomorphic cells or sarcomatoid and rhabdoid differentiation (Table 23.2 and Fig. 23.1), and that chromophobe RCC should not be graded [6]. In clear cell RCC , the ISUP system shows a strong association with cancer-specific outcome among surgically treated patients at the Mayo Clinic (Fig. 23.2) [7]. A study subsequent to the ISUP consensus conference found that the addition of coagulative tumor necrosis in the clear cell RCC grading system improved the prognostic ability of the ISUP grading system particularly for grade 3 tumors where grade 3 clear cell RCC without necrosis has a 5-year cancer specific survival of 62 % compared to 30 % for tumors that have necrosis [7].
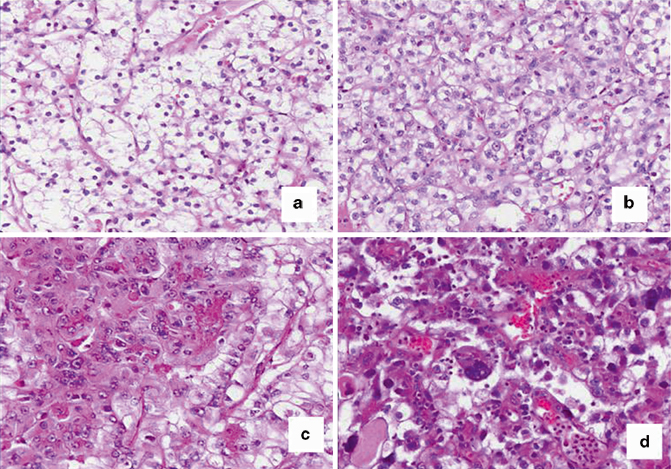
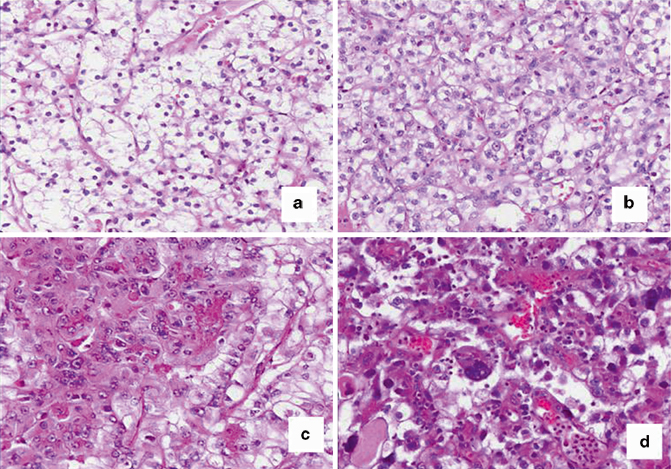
Fig. 23.1
ISUP grading for clear cell RCC. Grade 1 ( a), 2 ( b), and 3 ( c) are defined by nucleolar prominence while grade 4 ( d) contains pleomorphic cells
Fig. 23.2
Kaplan-Meier curve of patients treated by nephrectomy at the Mayo Clinic between 1970 and 2008 for clear cell renal cell carcinoma ( RCC). International Society of Urologic Pathology ( ISUP) grade is significantly associated with the outcome
Table 23.2
2012 ISUP grading system for clear cell and papillary RCC
ISUP grade | Feature |
|---|---|
Grade 1 | Absent or inconspicuous nucleoli |
Grade 2 | Nucleoli evident at 400x but inconspicuous or invisible at 100x |
Grade 3 | Nucleoli visible at 100x |
Grade 4 | Nuclear pleomorphism or rhabdoid or sarcomatoid differentiation |
Classification of Adult Renal Tumors
Clear Cell Renal Cell Carcinoma
Clear cell RCC accounts for approximately 70 % of all RCC [8]. The highest incidence occurs in the sixth and seventh decades but there is a wide age distribution, and males are affected twice as frequently as women. Presenting signs and symptoms include hematuria, abdominal pain or discomfort, scrotal varicocele, or generalized symptoms such as weight loss, fever, anorexia, or fatigue. Tumors are frequently identified incidentally by imaging for unrelated issues. Clear cell RCC is cortically based and are generally solitary, and multiple lesions should raise the consideration of von Hippel–Lindau disease caused by a germ-line mutation of the Von Hippel–Lindau (VHL) tumor suppressor gene at chromosome 3p25.
Clear cell RCC generally exhibits a round to lobulated growth pattern with pushing borders and formation of a fibrous pseudocapsule. High-grade clear cell RCC may have infiltrative margins. Low-grade tumors have a distinctive golden yellow appearance due to high lipid content that may be lost in higher grade tumors. Areas of hemorrhage, fibrosis and cystic degeneration are frequent. Clear cell RCC exhibits a sheet-like or nested growth pattern interspersed by a rich network of delicate thin-walled vessels. The cells within clear cell RCC typically have an abundant clear cytoplasm and prominent cell membranes. Higher grade tumors may lose this lipid production and show populations of cells having a more eosinophilic or granular appearance. Most clear cell RCCs show reactivity using antibodies against low-molecular-weight keratins, vimentin, RCC antigen, epithelial membrane antigen (EMA) carbonic anhydrase IX (CA IX), and CD10. Clear cell RCC is usually not positive for cytokeratin 7 (CK7) or alpha-methylacyl CoA racemase (AMACR), features that can be helpful separating clear cell from papillary RCC . CD117 and e-cadherin are negative in clear cell RCC in contrast to chromophobe RCC . Immunohistochemical stains may be useful in separating clear cell RCC from other subtypes on needle core biopsy specimens using a panel that includes CA IX, CD117, AMACR, CK7 and CD10 [9]. Genetic testing of clear cell RCC is characterized by structural alterations of the short arm of chromosome 3 (3p) resulting in the loss of genomic material at 3p21 and 3p12–14 or 3p25.
The outcome of patients with clear cell RCC is dependent on grade, stage, tumor size , coagulative tumor necrosis , and the presence of sarcomatoid and rhabdoid differentiation [10]. A number of clinical nomograms are available based on these features to predict outcome [11]. In regard to the three most common RCC subtypes, stage for stage and grade for grade, clear cell RCC has a worse outcome than papillary and chromophobe RCC (Fig. 23.3) [12].
Fig. 23.3
Patients with clear cell renal cell carcinoma ( RCC) have a significantly worse outcome than patients with papillary and chromophobe RCC . The Kaplan-Meier curve shows the outcome difference between all patients with these tumor types treated surgically at the Mayo Clinic. This outcome difference is also seen within the various tumor nodes metastasis (TNM) stages
Multilocular Cystic Renal Cell Carcinoma
Multilocular cystic RCC is an uncommon variant of clear cell RCC accounting for less than 2 % of RCC . This tumor is multicystic, and cysts are lined by cells with low grade nuclear features and clear cytoplasm in addition to small nests of clear cells in the cyst walls. Expansile nests of clear cells, however, disqualify a tumor from this diagnosis. The distinction of multilocular cystic RCC from a benign renal cortical cyst is made by the presence of multiple cell layers lining the cysts or more frequently and more dependably, by the presence of nests of clear cells in the cyst wall. Patients have an excellent outcome following tumor excision, and in our experience, none of these tumors has exhibited aggressive behavior.
Papillary Renal Cell Carcinoma
Papillary type RCC is the second most common type of RCC, and accounts for 10 % of adult RCC [8]. The age distribution, male to female ratio, and presenting signs and symptoms are similar to patients with clear cell RCC. Papillary RCC (PRCC) is typically solitary, but multifocal or bilateral lesions are not uncommon, and rarely indicative of an inherited RCC syndrome. Grossly, PRCC is lobulated and circumscribed and frequently show degenerative changes with hemorrhage and friability. PRCC demonstrates a wide variety of morphologic features but are characterized by a papillary or tubulo-papillary growth pattern. Papillary structures are composed of fibrovascular cores that contain lipid-laden histiocytes. Some tumors have a more solid and tubular growth pattern mimicking metanephric adenoma. Psammomatous calcifications, areas of hemosiderin deposition (that can be present within the cytoplasm of tumor cells) and necrosis are also frequent findings.
The cells comprising PRCC can be quite variable showing a range of minimal to abundant eosinophilic, basophilic, or clear cytoplasm. This variability in cytoplasmic appearance has resulted in the categorization of PRCC into two types based in part on these cytoplasmic differences (Fig. 23.4) [13]. Tumors classified as type 1 are comprised of cells with a minimal amount of pale to basophilic cytoplasm and small oval nuclei with inconspicuous nucleoli. Cells of type 1 tumors tend to be distributed in a single layer along the papillary structures and commonly show lipid-laden macrophages and psammomatous calcifications. Type 2 tumors are comprised of cells with more abundant eosinophilic cytoplasm and larger, round nuclei with visible nucleoli, showing a pseudostratified organization along the papillary structures. Classifying a particular PRCC as type 1 or 2 can be problematic at times as there can be areas demonstrating features of both types within a single tumor. Cells with clear cytoplasm can be seen in PRCC , though generally they do not show the clarity of clear cell RCC but have a suggestion of granularity within the cytoplasm. The presence in a tumor with a papillary growth pattern of a significant proportion of cells with clear cytoplasm should raise the possibility of a translocation-associated RCC. Immunohistochemically, tumors are positive for low molecular weight keratin, RCC, CD10 and P504S, and CK7 is present in a significant proportion of PRCC with type 1 morphology. In cases of low-grade papillary RCC with basophilic features that resembles metanephric adenoma, WT-1 and CK7 are particularly helpful, as PRCC is WT1 negative and CK7 positive in contrast to metanephric adenoma. Immunohistochemistry (transcription factor E3/transcription factor EB, TFE3/TFEB) and molecular genetic analysis can be used to differentiate from translocation-associated tumors. The most reproducible genetic abnormality in PRCC is trisomy of chromosomes 7 and 17. Patients with PRCC have a better outcome grade for grade and stage for stage when compared to patients with clear cell RCC. Features predictive of outcome include tumor grade and stage. Although it is recommended to report the type of PRCC, the grade is a stronger prognostic feature than the type [14].
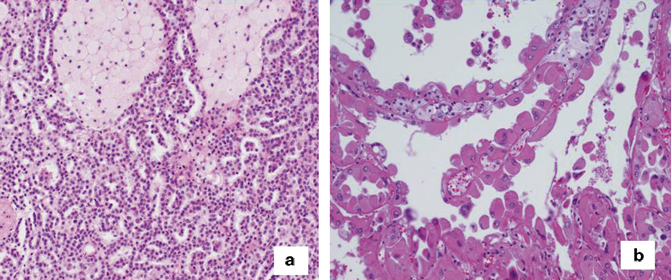
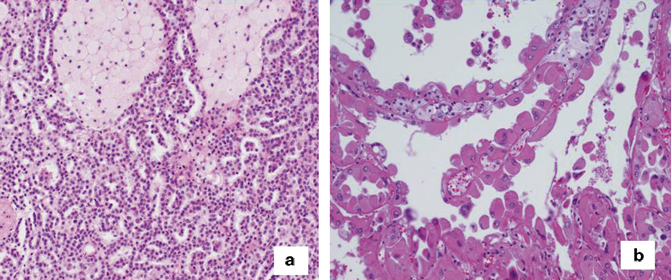
Fig. 23.4
Two examples of papillary RCC showing the wide spectrum in histologic appearance. The tumor ( a) is type 1, grade 1, while the tumor ( b) is type 2, grade 3
Clear Cell Papillary Renal Cell Carcinoma
Clear cell PRCC (also known as clear cell tubulopapillary RCC) is a relatively recently described subtype of RCC that displays features of both clear cell and PRCC. This entity, along with other recently described entities addressed in this chapter, is covered in greater detail in Chap. 26 of this book. These tumors are typically circumscribed, encapsulated, and solitary although multiple tumors have been described in patients. They show areas of papillary, acinar, or tubular growth with a cystic component common. The cells have a small to moderate amount of clear cytoplasm and small, compact nuclei. A helpful diagnostic feature is the orientation of the nuclei towards the apical aspect of cells lining tubules or papillary structures. Unlike PRCC, clear cell papillary RCC does not contain clusters of lipid-laden histiocytes or exhibit necrosis.
Clear cell papillary RCC demonstrates a distinct immunophenotype. Tumor cells are strongly positive for CK7 and CA IX, and are typically negative for CD10 and AMACR [15]. Molecular studies have shown that clear cell papillary RCC represents an entity distinct from either papillary or clear cell RCC as it does not exhibit trisomy 7 or 17 or alteration of chromosome 3p. Based on reports thus far, clear cell papillary RCC is an indolent tumor. Nearly all tumors are low grade (ISUP grade 1 and 2) and low stage, and no reports of death have been reported although in our experience, rare tumors have acted aggressively.
Chromophobe Renal Cell Carcinoma
Chromophobe RCC constitutes approximately 5–10 % of RCC [8, 10]. Signs and symptoms, age distribution and male to female ratio are similar to other RCC subtypes. Chromophobe RCC can be quite large and most are circumscribed, homogenous, and lack necrosis (Fig. 23.5). Higher stage tumors and tumors with necrosis should raise concern for sarcomatoid differentiation. Chromophobe RCC has a characteristic histologic appearance with solid growth and cells that have distinct cell membranes, abundant clear to eosinophilic cytoplasm with perinuclear clearing and irregular nuclei imparting a “plant cell” appearance to the tumor. Some tumors are composed of cells with eosinophilic cytoplasm, the so-called eosinophilic variant of chromophobe RCC. The nuclei in chromophobe RCC have a characteristic appearance and are particularly helpful in separating from other tumors, particularly oncocytoma. The nuclei have irregular wrinkled contours, often described as “raisinoid” or “koilocytotic” with condensed chromatin and inconspicuous nucleoli. Chromophobe RCC usually demonstrate reactivity with antibodies against pan keratins, CK7, CD117 and e-cadherin and are usually negative for CD10 and vimentin. The most common recurrent genetic abnormalities described in chromophobe RCC are losses of whole chromosomes 1, 2, 6, 10, 13, 17, and 21. Outcome for chromophobe RCC is similar to patients with papillary RCC. Features associated with outcome include stage, tumor necrosis , and presence of sarcomatoid component [10]. The ISUP recommends that tumors that share features of chromophobe and oncocytoma be designated as “hybrid” oncocytic chromophobe tumor and be classified as chromophobe RCC [3] .
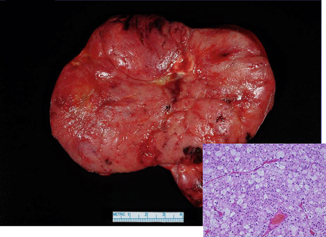
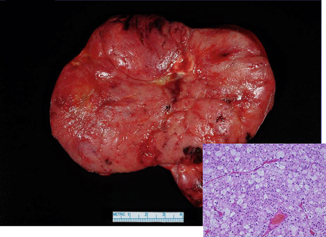
Fig. 23.5




Chromophobe RCC can be quite large, and the histologic appearance shows a classic “plant cell” appearance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


