Chronic Granulomatous Lymphadenitis
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Granulomatous inflammation is specific type of inflammatory response
Characterized by accumulation of modified macrophages (epithelioid cells)
Initiated by infectious or noninfectious agents
Requires poorly digestible irritants and T-cell mediated immunity directed at irritant
Chronic granulomatous lymphadenitis (CGL) is characterized by
Accumulation of activated macrophages and inflammatory cells forming granulomas within lymph node
Often associated with necrosis or acute inflammation
Etiology/Pathogenesis
Infections are most common cause of CGL
Autoimmune diseases (e.g., sarcoidosis)
Foreign bodies (e.g., talc, suture, lipid)
Clinical Issues
Cervical lymph nodes most commonly involved
Microscopic Pathology
CGL may be classified as caseating or noncaseating
M. tuberculosis is most common cause of caseating granulomas
Ancillary Tests
PCR allows identification of infectious agents in cases that were previously regarded as unknown etiology
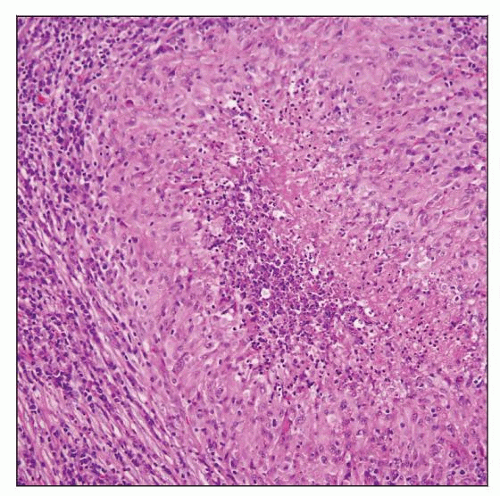 Paraffin section shows necrotizing chronic granulomatous lymphadenitis. The granulomas are composed of central necrosis surrounded by epithelioid histiocytes and inflammatory cells. |
TERMINOLOGY
Abbreviations
Chronic granulomatous lymphadenitis (CGL)
Synonyms
Chronic granulomatous inflammation of lymph node
Definitions
Granulomatous inflammation is a specific type of inflammatory response
Characterized by accumulation of modified macrophages (epithelioid cells)
Initiated by infectious or noninfectious agents
Requires poorly digestible irritants and T-cell mediated immunity directed at irritant
Chronic granulomatous lymphadenitis is characterized by
Accumulation of activated macrophages and inflammatory cells forming granulomas within lymph node
Results from deposition of indigestible antigenic material within tissue
Often associated with necrosis or acute inflammation
ETIOLOGY/PATHOGENESIS
Infectious Agents
CGL is usually caused by wide variety of infectious agents including
Mycobacteria, bacteria, viruses, fungi, and parasites
Chlamydia, spirochetes
Infectious CGL can be classified into 3 subgroups based on its etiology
Infections caused by well-recognized organisms
Mycobacterium tuberculosis is most common
Infections caused by organisms identified by molecular methods but not readily isolated by conventional microbiological methods
Infectious etiology is strongly suspected, but causal organisms have not yet been identified
Advances in molecular diagnostic technology have allowed identification of more organisms
Previously, cause of these infections was unknown
Other Causes
There are a large number of other causes of CGL
Foreign bodies or other irritants/antigens
Autoimmune diseases/mechanisms
e.g., sarcoidosis
Granulomas can occur in patients with lymphoma
Granulomas also can occur in lymph nodes draining nonhematopoietic neoplasms
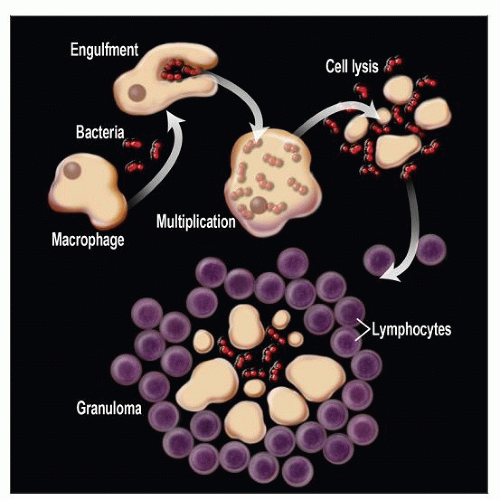
Pathogenesis
CGL is result of complex interplay of events
Presence of invading agent (e.g., bacteria) in tissue results in recruitment of monocytes-macrophages from circulation
Monocytes-macrophages engulf bacteria
Bacteria multiply within macrophages
Macrophages process bacteria and present them to activated T-helper cells
Release of cytokines and chemokines by activated macrophages and T-helper cells; causes cell lysis
Macrophages mature into epithelioid cells or fuse to form multinucleated giant cells
Granulomas form when bacteria and debris are surrounded by macrophages and inflammatory cells
CLINICAL ISSUES
Site
Lymph node group involved depends in part on
Initiating agent
1st route of entry into body
Cervical lymph nodes are most common
Any lymph node or lymph node group can be affected
Presentation
Lymphadenopathy, localized or general
May be accompanied by systemic symptoms
Laboratory Tests
Microbiologic culture and identification by biochemical methods
Serologic tests are helpful in
Identifying infectious agents
Determining timing of exposure to organism
Polymerase chain reaction (PCR) methods detect infectious agents with high sensitivity
Infectious agents have been identified in diseases that were previously of unknown etiology
Treatment
Empiric antibiotics
Antituberculous therapy
Surgical manipulation
Prognosis
Depends on specific etiology and therapy administered
Benign clinical course with good prognosis
IMAGE FINDINGS
General Features
Well-defined lymph nodes
Increased in number &/or size
CT scans are 1st-line imaging tool to evaluate lymphadenopathy
Standard x-rays and CT scans show consolidation
With or without central necrosis
MACROSCOPIC FEATURES
General Features
Cut surface can appear nodular (if macrogranulomas)
Yellow areas can be seen corresponding to necrotic foci
MICROSCOPIC PATHOLOGY
Histologic Features
CGL may be classified as immune or foreign body type
Immune type
Caused by insoluble particles (e.g., bacteria) that elicit cell-mediated immune response
Can further divide these into caseating and noncaseating granulomas
Caseating granulomas
Composed of central areas of coagulative necrosis
Peripheral concentric layers of epithelioid cells, Langhans giant cells, lymphocytes, and fibroblasts
Organisms may be identified by using special stains
M. tuberculosis is most common cause of caseating granulomas
Noncaseating granulomas
Composed of collection of epithelioid cells, Langhans giant cells, lymphocytes, and histiocytes
Eosinophils can occur in granulomas caused by parasites
Acute inflammatory cells common in granulomas caused by fungi
Foreign body type
Cytologic Features
Epithelioid histiocytes and inflammatory cells can be identified in fine needle aspiration smears
In some cases, granulomas can be recognized
Special stains can be performed on smears
ANCILLARY TESTS
Immunohistochemistry
Mycobacterial antigens can be detected and typed with monoclonal antibodies conjugated to peroxidase
PCR
Highly sensitive and has identified infectious agents in diseases that previously had no known etiology
Special Stains
Acid-fast bacilli can be demonstrated by Ziehl-Neelsen, Kinyoun, or Fite-Faraco stain
Fungal-like organisms can be highlighted with periodic acid-Schiff (PAS) or Grocott methenamine silver stain
Gram-positive and Gram-negative organisms can be seen with Gram stain
Parasites can be highlighted by Giemsa stain
DIFFERENTIAL DIAGNOSIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree