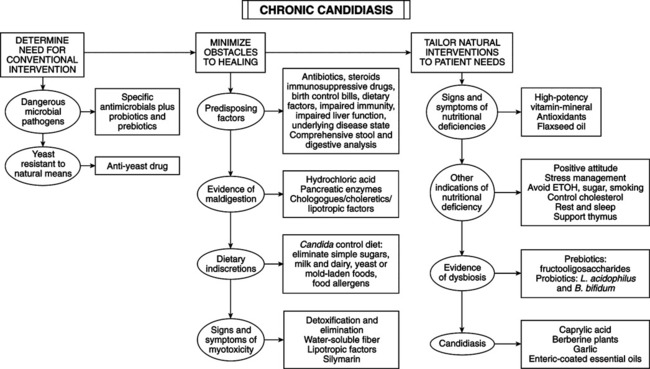
• Causal factors: multifactorial; correct factors predisposing overgrowth; requires more than killing yeast with antifungals, synthetic or natural; prolonged antibiotic use is the key factor in most cases—suppresses normal intestinal bacteria that control yeast, suppresses immunity, generates antibiotic-resistant mi-crobes, may contribute to Crohn’s disease. • Related syndromes: small intestinal bacterial overgrowth and leaky gut associated with Candida overgrowth; may produce identical symptoms to the yeast syndrome. • Screening method: comprehensive questionnaire (see Textbook, “Candida Questionnaire”). • Best method: clinical evaluation—knowledge of yeast-related illness, detailed medical history, patient questionnaire. • Comprehensive stool and digestive analysis (CSDA): more clinically useful; evaluates digestion, intestinal environment, and absorption; indicates underlying digestive disturbance; may pinpoint other causes (e.g., small intestinal bacterial overgrowth, leaky gut syndrome). • Laboratory techniques (used only to confirm): stool cultures for Candida, antibody to Candida, Candida antigens in the blood; rarely needed; confirm what history, physical examination, CDSA reveal; confirm Candida is factor, monitor therapy. • Sugar: chief nutrient of Candida; restrict sugar, honey, maple syrup, and fruit juice. • Milk and dairy products: high lactose content promotes Candida; contain food allergens; may contain trace levels of antibiotics disrupting GI bacteria, promoting Candida. • Mold and yeast-containing foods: avoid foods with high yeast or mold levels: alcohol, cheese, dried fruits, peanuts. • Food allergies: common in patients with yeast syndrome; enzyme-linked immunosorbent assay (ELISA) tests for immunoglobulin (Ig) E- and IgG-mediated food allergies.
Chronic Candidiasis
GENERAL CONSIDERATIONS
DIAGNOSIS
THERAPEUTIC CONSIDERATIONS
Diet
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Chronic Candidiasis
