Patient Story
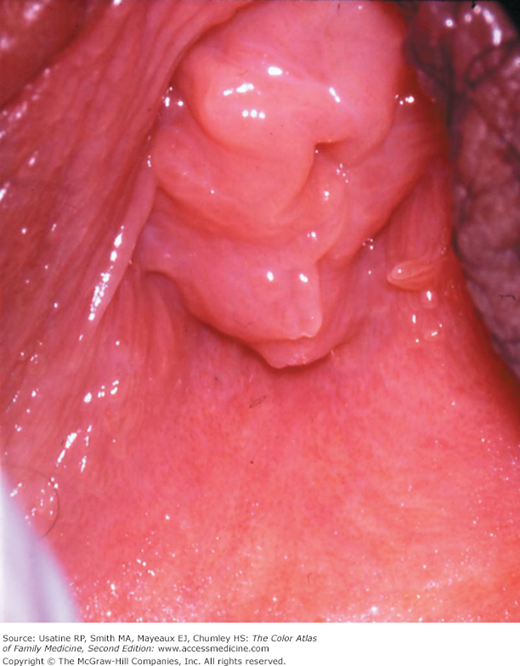
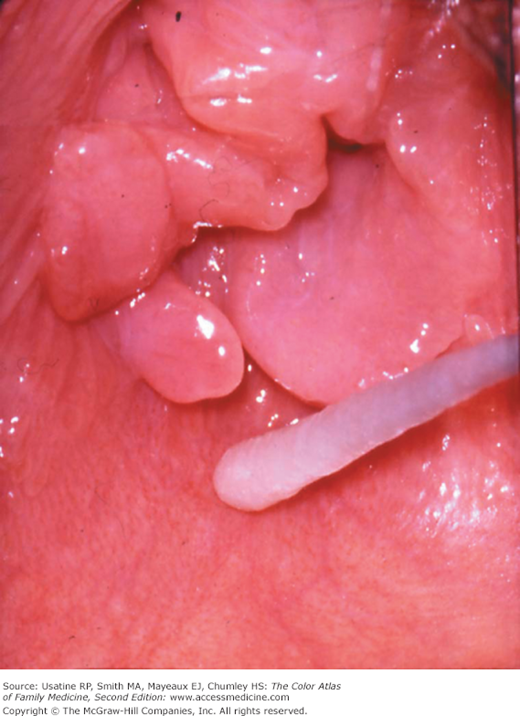
A 12-year-old girl is being seen for chronic abdominal pain by her family physician. The physician asks the mother to step out of the room and does a complete history including the HEADSS (home life, education level, activities, drug use, sexual activity, suicide ideation/attempts) questions. The girl tearfully reports that her stepfather has been touching her in her private areas when her mother is not home. On examination with a female nurse chaperone in the room, the physician finds that the girl’s hymen initially appears normal (Figure 9-1). However, when the girl is more carefully examined with a cotton-tip applicator, a healed posterior hymenal transection is seen (Figure 9-2). When the girl is asked whether any other types of sexual abuse occurred with her stepfather, she admits to repeated penile penetration. Although rare, sometimes the examination reveals more than what the child is willing to disclose about the abuse. Partial disclosures of abuse are common in children. In addition, the findings of sexual abuse tend to be subtle and are easily missed if a careful examination and special techniques are not used. Attempts are made to reassure the girl that this should never happen and that this is not her fault. Her mother is brought back into the room and after a sensitive discussion, the police are called and Child Protective Services notified.
Figure 9-2
Hymenal cleft visible when the girl in Figure 9-1 is more carefully examined using a saline moistened cotton-tip applicator to gently separate and demonstrate the edges of the hymen. This injury was caused by sexual abuse and may have been missed without the more careful examination. (Courtesy of Nancy D. Kellogg, MD.)
HEADSS is an acronym that provides a framework for interviewing adolescents and children about health risks. The questions start from easiest and least sensitive to more sensitive questions that need to be asked:
Epidemiology
- The U.S. Department of Health and Human Services compilation of Child Protective Services (CPS) data from 48 states in 2008 indicates there were 772,000 children confirmed as victims of abuse.1 Of these, 9% were victims of sexual abuse. Not included in these numbers are several thousand additional victims who are sexually assaulted by nonfamily members; these cases are reported to law enforcement but not CPS.
- Sexual abuse of girls occurs at much higher rate than boys: 2.3 per 1000 females versus 0.6 per 1000 males.2
- Up to 50% of abusive sexual acts involve penetration of the vagina, anus, or oral cavity, or oral-genital contact.3 In general, penetrative types of abuse are associated with poorer medical and mental health outcomes.
Etiology and Pathophysiology
Child sexual abuse occurs when a child is involved in sexual activities that he or she cannot comprehend, for which the child is developmentally unprepared and cannot or does not give consent, and/or that violate laws. All states have laws that require physicians to report a suspicion of abuse to child protection or law enforcement agencies.
Most sexual abuse involves an adult perpetrator the child knows and is expected to trust who uses deception and position of authority to gain the child’s acquiescence and accommodation to the abuse;4 it is not unusual for the abuse to progress from less to more severe and intrusive sexual acts, and for the child to wait months or years to disclose the abuse.
Diagnosis
- Child victims of sexual abuse may have behavior changes, depression, increased sexual behaviors, somatic complaints (e.g., headaches or abdominal pain, constipation, enuresis/encopresis, genital/anal pain), or may be asymptomatic.
- Child may present to a medical provider for the following reasons:
- Child has disclosed abuse (most common); it is rare for the abuse to be witnessed. Referrals to specialized programs with clinicians trained in the assessment of child sexual abuse is recommended, and are generally accessible in most areas of the United States.
- Caregiver suspects abuse and presents to the clinician because of behavioral or physical symptoms.
- Child is brought for routine care and sexual abuse is suspected based on clinical findings (e.g., acute or healed genital injuries, vaginal discharge in a prepubertal child, lesions suggestive of human papillomavirus [HPV] or herpes simplex virus [HSV]).
- Child has disclosed abuse (most common); it is rare for the abuse to be witnessed. Referrals to specialized programs with clinicians trained in the assessment of child sexual abuse is recommended, and are generally accessible in most areas of the United States.
- Recent studies show that less than 5% of child sexual abuse victims have physical examination findings indicative of penetrative trauma because the type of sexual act either does not result in tissue damage or because when tissue damage occurs, most injuries heal quickly and completely.5–7 In a study of 36 pregnant adolescents, only two had evidence of penetrative trauma.8 The medical diagnosis relies predominantly on the child’s history and clinicians should remember that “normal” does not mean “nothing happened.”
- Tips for doing the physical examination:
- The anogenital inspection should utilize optimal direct light source, magnification, and appropriate examination positions and techniques.
- Recommended examination positions include supine frogleg or lithotomy and prone knee-chest; the latter position is particularly important to confirm any posterior (between the 4 and 8 o’clock positions of the hymen in supine) defects of the hymen that are seen in supine position.
- Various examination techniques include labial separation and traction (gently pulling the labia outward and inferiorly), gluteal lifting in prone knee-chest and using cotton-tipped applicator for separating tissues.
- In some cases, it may help to have an assistant gently squirt a small amount of nonbacteriostatic saline onto the hymen as the examiner uses gentle labial traction; this procedure is used to free folded hymenal edges.
- A speculum examination and use of a cotton-tipped applicator to separate hymenal edges are traumatic procedures for prepubertal females and should not be used.
- Most findings of anal trauma can be visualized by gently spreading the anal folds.
- The anogenital inspection should utilize optimal direct light source, magnification, and appropriate examination positions and techniques.
- Physical findings concerning for abuse include:9

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree