Chemotherapy of Helminth Infections
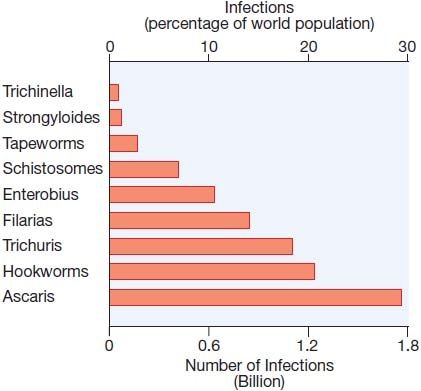
Infections with helminths, or parasitic worms, affect more than 2 billion people worldwide (Figure 51–1). In regions of rural poverty in the tropics, where prevalence is greatest, simultaneous infection with more than 1 type of helminth is common.
Figure 51–1 Relative incidence of helminth infections worldwide.
Worms pathogenic for humans are Metazoa and can be classified into roundworms (nematodes) and 2 types of flatworms, flukes (trematodes) and tapeworms (cestodes). These biologically diverse eukaryotes vary with respect to life cycle, bodily structure, development, physiology, localization within the host, and susceptibility to chemotherapy. Immature forms invade humans via the skin or GI tract and evolve into well-differentiated adult worms with characteristic tissue distributions. With few exceptions, such as Strongyloides and Echinococcus, these organisms cannot complete their life cycle and replicate within the human host to produce mature offspring. Therefore, the extent of exposure to these parasites dictates the number of parasites infecting the host. Second, any reduction in the number of adult organisms by chemotherapy is sustained unless reinfection occurs. The burden of parasitic helminths within an infected population is not uniformly distributed, and it typically displays a negative binomial distribution whereby relatively few persons carry the heaviest parasite burden, resulting in increased morbidity in these individuals who also contribute disproportionately to transmission.
Anthelmintics are drugs that act either locally within the gut lumen to cause expulsion of worms from the GI tract, or systemically against helminths residing outside the GI tract. Therapy for many tissue-dwelling helminths, such as filarial parasites, is not fully effective. There is increasing appreciation of the impact of helminth infections on the health and education of school-aged children. In a massive public health effort, international health organizations are promoting the periodic and frequent use of anthelmintic drugs in schools as a means to control morbidity caused by soil-transmitted helminths and schistosomes in developing countries. Control programs employing anthelmintics rank among the world’s largest health efforts, and hundreds of millions of people receive treatment annually.
This chapter is divided into 2 main parts:
• Clinical presentation and recommended chemotherapy for common helminth infections
• Pharmacological properties of specific anthelmintics
HELMINTH INFECTIONS AND THEIR TREATMENT
NEMATODES (ROUNDWORMS)
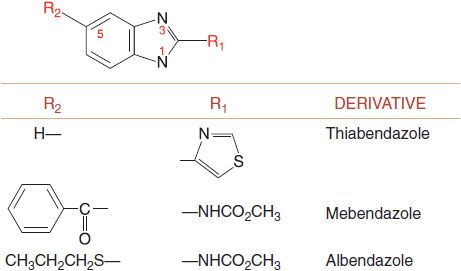
The major nematode parasites of humans include the soil-transmitted helminths (STHs; sometimes referred to as “geohelminths”) and the filarial nematodes. The major STH infections (ascariasis [roundworm], trichuriasis [whipworm], and hookworm infection) are among the most prevalent infections in developing countries. The agents most widely employed for reducing morbidity are the benzimidazole (BZ) anthelmintics, either albendazole (ALBENZA and ZENTEL) or mebendazole (VERMOX, others) (Figure 51–2).
Figure 51–2 Structure of the Benzimidazoles.
ROUNDWORM: ASCARIS LUMBRICOIDES. Ascaris lumbricoides, known as the “roundworm,” may affect from 70-90% of persons in some tropical regions; it is also seen in temperate climates. People become infected by ingesting food or soil contaminated with embryonated A. lumbricoides eggs.
The preferred anthelmintics are the BZs, mebendazole and albendazole, and the broad-spectrum drug pyrantel pamoate. Cure with any of these drugs can be achieved in nearly 100% of cases. Mebendazole and albendazole are preferred for therapy of asymptomatic to moderate ascariasis but should be used with caution to treat heavy Ascaris infections, alone or with hookworms. Some clinicians recommend the use of pyrantel for heavy Ascaris infections because this agent paralyzes the worms prior to their expulsion.
TOXOCARIASIS: TOXOCARA CANIS. This zoonotic infection, caused by the canine ascarid Toxocara canis, is a common helminthiasis in North America and Europe.
Three major syndromes are caused by T. canis infection: visceral larva migrans (VLM), ocular larva migrans (OLM), and covert toxocariasis (CTox). CTox may represent an under-appreciated cause of asthma and seizures. Specific treatment of VLM is reserved for patients with severe, persistent, or progressive symptoms. Albendazole is the drug of choice. In contrast, anthelmintic therapies for OLM and CTox are controversial.
HOOKWORM: NECATOR AMERICANUS, ANCYLOSTOMA DUODENALE. These closely related hookworm species infect ~1 billion people in developing countries (see Figure 51–1).
N. americanus is the predominant hookworm worldwide, whereas A. duodenale is focally endemic in Egypt and in parts of northern India and China. Hookworm larvae live in the soils and penetrate exposed skin. After reaching the lungs, the larvae migrate to the oral cavity and are swallowed. After attaching to the small intestinal mucosa, the derived adult worms feed on host blood. There is a general relationship between the number of hookworms (hookworm burden) as determined by quantitative fecal egg counts and fecal blood loss. Unlike heavy Ascaris and Trichuris infections, which occur predominantly in children, heavy hookworm infections also occur in adults, including women of reproductive age. Although iron supplementation (and transfusion in severe cases) often is helpful in individuals with severe iron-deficiency anemia, the major goal of treatment is to remove blood-feeding adult hookworms from the intestines. Albendazole is the agent of first choice and is considered far superior to mebendazole at removing adult hookworms from the GI tract. Oral albendazole is the drug of choice for treating cutaneous larva migrans, or “creeping eruption,” which is due most commonly to skin migration by larvae of the dog hookworm, A. braziliense. Oral ivermectin or topical thiabendazole also can be used.
WHIPWORM: TRICHURIS TRICHIURA. Trichuris (whipworm) infection is acquired by ingestion of embryonated eggs. In children, heavy Trichuris worm burdens can lead to colitis, Trichuris dysentery syndrome, and rectal prolapse. Mebendazole and albendazole are the most effective agents for treatment of whipworm. Both drugs provide significant reductions in host worm burdens even when used in a single dose. However, a “cure” (i.e., total worm burden removal) typically requires a 3-day course of therapy.
THREADWORM: STRONGYLOIDES STERCORALIS. S. stercoralis is distinctive among helminths in being able to complete its life cycle within the human host, infecting 30-100 million people worldwide, most frequently in the tropics and other hot, humid locales. In the U.S., strongyloidiasis is still endemic in the Appalachian region and in parts of the American South.
Infective larvae in fecally contaminated soil penetrate the skin or mucous membranes, travel to the lungs, and ultimately mature into adult worms in the small intestine, where they reside. Many infected individuals are asymptomatic, but some experience skin rashes, nonspecific GI symptoms, and cough. Life-threatening disseminated disease, known as the hyperinfection syndrome, can occur in immunosuppressed persons, even decades after the initial infection when parasite replication in the small intestine is unchecked by a competent immune response. Ivermectin is the drug of choice for treatment of strongyloidiasis.
PINWORM: ENTEROBIUS VERMICULARIS. Enterobius is one of the most common helminth infections in temperate climates, including the U.S.
Although this parasite rarely causes serious complications, pruritus in the perianal and perineal region can be severe, and scratching may cause secondary infection. In female patients, worms may wander into the genital tract and penetrate into the peritoneal cavity. Salpingitis or even peritonitis may ensue. Because the infection easily spreads throughout members of a family, a school, or an institution, the physician must decide whether to treat all individuals in close contact with an infected person. Pyrantel pamoate, mebendazole, and albendazole are highly effective. Single oral doses of each should be repeated after 2 weeks. When their use is combined with rigid standards of personal hygiene, a very high proportion of cures can be obtained.
TRICHINOSIS: TRICHINELLA SPIRALIS. T. spiralis is an ubiquitous zoonotic nematode parasite. Trichinosis in the U.S. and the developing world is usually caused by eating the under- or uncooked meat of deer and wild pigs.
When released by acid stomach contents, encysted larvae mature into adult worms in the intestine. Adults then produce infectious larvae that invade tissues, especially skeletal muscle and heart. Severe infection can be fatal, but more typically causes marked muscle pain and cardiac complications. Infection is readily preventable by cooking all pork products thoroughly before eating. The encysted larvae are killed by exposure to heat of 60°C for 5 min. Albendazole and mebendazole are effective against the intestinal forms of T. spiralis that are present early in infection. The efficacy of these agents or any anthelmintic agent on larvae that have migrated to muscle is questionable.
LYMPHATIC FILARIASIS: WUCHERERIA BANCROFTI, BRUGIA MALAYI, AND B. TIMORI. Adult worms that cause human lymphatic filariasis (LF) dwell in the lymphatic vessels. Transmission occurs through the bite of infected mosquitoes; ~90% of cases are due to W. bancrofti; most of the rest are due to B. malayi.
In LF, host reaction to the adult worms initially cause lymphatic inflymphangitis, and lymphadenitis. This can progress to lymphatic obstruction and is often exacerbated by secondary attacks of bacterial cellulitis, leading to lymphedema manifested by hydrocele and elephantiasis. All at-risk individuals should be treated once yearly with an oral 2-drug combination. For most countries, the WHO recommends diethylcarbamate (DEC) for its micro- and macrofilaricidal effect in combination with albendazole to enhance macrofilaricidal activity. The exceptions are in many parts of sub-Saharan Africa and Yemen, where either loiasis or onchocerciasis are co-endemic. In these regions, ivermectin is substituted for DEC. DEC and ivermectin clear circulating microfilariae from infected subjects, thereby reducing the likelihood that mosquitoes will transmit LF to other individuals. DEC is the drug of choice for specific therapy directed against adult worms. However, the anthelmintic effect on the adult worms is variable. In longstanding elephantiasis, surgical measures may be required to improve lymph drainage and remove redundant tissue.
LOIASIS: LOA LOA. L. loa is a tissue-migrating filarial parasite found in large river regions of Central and West Africa; the parasite is transmitted by deerflies. Adult worms reside in subcutaneous tissues, and infection may be recognized when these migrating worms cause episodic and transient subcutaneous “Calabar” swellings. Adult worms may also pass across the sclera, causing “eyeworm.”
Rarely, encephalopathy, cardiopathy, or nephropathy occurs in association with heavy infection, particularly following chemotherapy. DEC currently is the best single drug for the treatment of loiasis. Glucocorticoids may be administered to ameliorate post-treatment acute reactions. In rare instances, life-threatening encephalopathy follows the treatment of loiasis, probably due to the inflammatory reaction to dead or dying microfilariae lodged in the cerebral microvasculature. Guidelines have been developed aimed at screening out populations with heavy infection so that they are not administered ivermectin, which has also been associated with fatal encephalopathy.
RIVER BLINDNESS (ONCHOCERCIASIS). Onchocerca volvulus, transmitted by blackflies near fast-flowing streams and rivers, infects 17-37 million people in 22 countries in sub-Saharan Africa and fewer people (<100,000) in 4 Latin American countries.
Inflammatory reactions, primarily to microfilariae rather than adult worms, affect the subcutaneous tissues, lymph nodes, and eyes. Onchocerciasis is a leading cause of infectious blindness. Ivermectin is the drug of choice for control and treatment of onchocerciasis. DEC is no longer recommended because ivermectin produces far milder systemic reactions and few if any ocular complications. Although suramin (see Chapter 50) kills adult O. volvulus worms, treatment with this relatively toxic agent is generally not advised.
GUINEA WORM: DRACUNCULUS MEDINENSIS. Known as the guinea, dragon, or Medina worm, this parasite causes dracunculiasis, an infection in decline (<5000 cases as of 2009, mostly in rural Sudan, Ghana, and Mali).
People become infected by drinking water containing copepods that carry infective larvae. After ~1 year, the adult female worms migrate and emerge through the skin, usually of the lower legs or feet. Strategies such as filtering drinking water and reducing contact of infected individuals with water have markedly reduced the transmission and prevalence of dracunculiasis in most endemic regions. There is no effective anthelmintic for treatment of D. medinensis infection. Metronidazole, 250 mg given 3 times a day for 10 days, may provide symptomatic and functional relief.
CESTODES (FLATWORMS)
BEEF TAPEWORM: TAENIA SAGINATA. Humans are the definitive hosts for T. saginata.
Preventable by cooking beef to 60°C for >5 min, this infection rarely produces serious clinical disease, but it must be distinguished from that produced by Taenia solium. Praziquantel (BILTRICIDE) is the drug of choice for treatment of infection by T. saginata, although niclosamide can also be used.
PORK TAPEWORM: TAENIA SOLIUM. T. solium causes 2 types of infection. The intestinal form with adult tapeworms is caused by eating undercooked meat containing cysticerci, or more commonly by fecal-oral transmission of infective T. solium eggs from another infected human host. Cysticercosis, the far more dangerous systemic form that usually coexists with the intestinal form, is caused by invasive larval forms of the parasite.
Systemic infection results either from ingestion of fecally contaminated infectious material, or from eggs liberated from a gravid segment passing upward into the duodenum, where the outer layers are digested. In either case, larvae gain access to the circulation and tissues, exactly as in their cycle in the intermediate host, usually the pig. Invasion of the brain (neurocysticercosis) is common and dangerous. Niclosamide is preferred for treatment of intestinal infections with T. solium because it will have no effect on occult neurocysticercosis. Albendazole is the drug of choice for treating cysticercosis. The advisability of chemotherapy for neurocysticercosis is controversial, being appropriate only when it is directed at live cysticerci and not against dead or dying cysticerci. Pretreatment with glucocorticoids is strongly advised in this situation to minimize inflammatory reactions to dying parasites. Some experts advocate use of albendazole therapy for patients with multiple cysts or viable cysts.
FISH TAPEWORM: DIPHYLLOBOTHRIUM LATUM. D. latum is found most commonly in rivers and lakes of the Northern Hemisphere. In North America, the pike is the most common second intermediate host. The eating of inadequately cooked infested fish introduces the larvae into the human intestine; the larvae can develop into adult worms up to 25 m long. Most infected individuals are asymptomatic. The most frequent manifestations include abdominal symptoms and weight loss; megaloblastic anemia develops due to a deficiency of vitamin B12. Therapy with praziquantel readily eliminates the worm and ensures hematological remission.
DWARF TAPEWORM: HYMENOLEPIS NANA. H. nana is the smallest and most common tapeworm parasitizing humans. H. nana is the only cestode that can develop from ovum to mature adult in humans without an intermediate host. Cysticerci develop in the villi of the intestine and then regain access to the intestinal lumen where larvae mature into adults. Praziquantel is effective against H. nana infections, but higher doses than used for other tapeworm infections usually are required. Albendazole is partially efficacious against H. nana.
ECHINOCOCCUS SPECIES. Humans are one of several intermediate hosts for larval forms of Echinococcus species that cause “cystic” (E. granulosus) and “alveolar” (E. multilocularis and E. vogeli
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree