Coronary artery anatomy. (A) Anterior view. (B) Posterior view. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Left main coronary artery disease
•Three-vessel disease
•Two-vessel disease with proximal left anterior descending artery disease and EF <50%
A 22-year-old man presents to the emergency department (ED) with a stab wound to the chest. He is hypotensive. A focused assessment with sonography for trauma (FAST) ultrasound examination of the heart demonstrates collapse of the right atrium. What is the differential diagnosis?
The finding of right atrial collapse suggests a tension pneumothorax or cardiac tamponade. Both conditions may also present with jugular venous distention. The absence of breath sounds over one lung mandates the emergent placement of a large-bore needle (or a chest tube, if available) to decompress the tension pneumothorax. The diagnosis of cardiac tamponade can be confirmed with the sonographic finding of pericardial blood.
•The right ventricle is the most commonly injured chamber in both blunt and penetrating cardiac trauma
•The right atrium is a low-pressure chamber and collapses with tension pneumothorax or cardiac tamponade
•A tension pneumothorax decreases venous return by compressing the superior and inferior vena cava
•A chest X-ray (CXR) should not be performed because it wastes time
•Emergent chest decompression is indicated
•Penetrating cardiac injury
•Often presents with tamponade
•Emergent pericardiocentesis is needed for cardiac tamponade unless an ED thoracotomy is indicated
•ED thoracotomy
•Blunt trauma—use only if pulse lost in the emergency room (ER)
•Penetrating trauma—use only if pulse lost en route to ER or in ER
•Left anterolateral thoracotomy at fourth interspace
•Open pericardium anterior to phrenic nerve to relieve tamponade
•Start cardiac massage and attempt to control bleeding from injury
•Blunt cardiac injury
•If there is a new murmur, ectopy, or increased cardiac enzymes → emergent echo
•Otherwise, admit for serial enzymes and cardiac monitoring
•Aortic injury
•15% of deaths from motor vehicle accidents
•Due to rapid deceleration → disruption at points of aortic fixation, such as the ligamentum arteriosum
•Diagnosis
•Unequal radial pulses if subclavian takeoff is involved
•CXR: Widened mediastinum, loss of aortic knob
•Treat with antihypertensives until definitive surgical repair
Following a lower extremity vascular bypass procedure, a patient is noted to be slightly hypothermic. A pulmonary artery catheter reveals a pulmonary capillary wedge pressure of 20, a cardiac index of 1.2, and a systemic vascular resistance of 1,400. What treatment is indicated?
These findings are most consistent with postoperative heart failure or a postoperative MI. Dobutamine is the treatment of choice for postoperative heart failure presenting with low cardiac output.
Cardiogenic Shock/Heart Failure
•Postoperative cardiac failure is suggested by:
•Increased central venous pressure
•Increased pulmonary artery wedge pressure
•Decreased cardiac output (which may manifest as decreased urine output)
•A dobutamine or dopamine infusion is indicated to treat cardiogenic shock
•Receptors
•α1—vascular smooth muscle constriction; gluconeogenesis, glycolysis
•β1—myocardial contraction and SA rate
•β2—relaxes vascular and bronchial smooth muscle; ↑ insulin, glucagon, and renin
•Dopamine—relaxes renal and splanchnic smooth muscle
•Inotropes
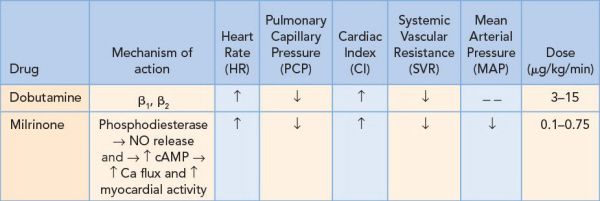
•Mixed inotropes/vasoconstrictors
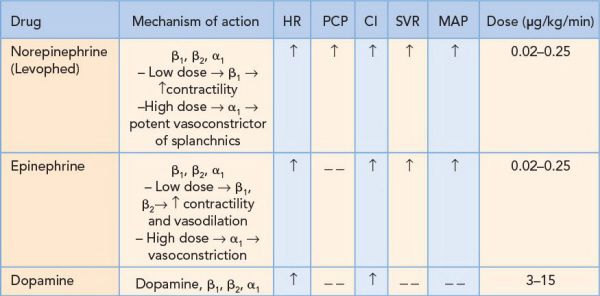
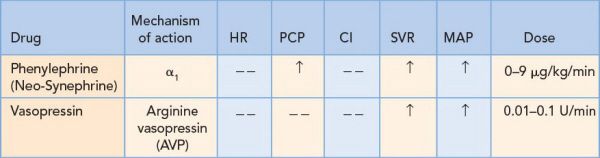
•Vasoconstrictors
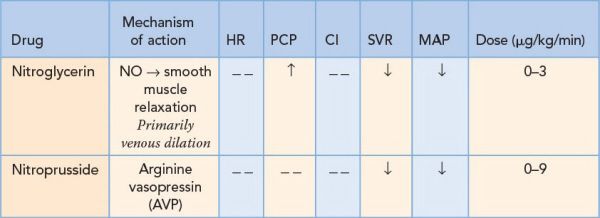
•Vasodilators
•Nitroprusside can → cyanide toxicity
What is the mechanism of an intra-aortic balloon pump?
A balloon pump augments diastolic blood flow and reduces afterload.
Intra-aortic Balloon Pump
•Can be placed at the bedside
•The tip of the catheter should be just distal to the left subclavian 1 to 2 cm below the top of the arch
•Reduces afterload by inflating during diastole (40 milliseconds before the T-wave) and deflating during the P-wave (systole) → increased perfusion to the coronary arteries
•The indications for an intra-aortic balloon pump include
•Acute MI with shock
•Acute mitral insufficiency
A 56-year-old man is found to have a new holosystolic murmur 5 days after an acute MI. What is the next step in management?
A transesophageal echocardiogram should be performed for any suspicious findings following an acute MI. Given a new systolic murmur, it is important to rule out mitral regurgitation (MR) and a ventricular septal defect (VSD).
Acute Myocardial Infarction
•Complications after an acute MI usually present 3 to 7 days later and include
•MR from a ruptured papillary muscle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


