Burn Injuries
Nirav Patel
Key Questions
• What are the most common causes of burn injuries?
• How are burn degree and severity determined?
• What are the principles that guide the management of burn injuries?
• What are the potential complications associated with burn injuries?
![]()
http://evolve.elsevier.com/Copstead/
Burns are injuries to tissues caused by contact with dry heat (flame or hot surfaces), moist heat (steam or hot liquids), electricity (current or lightning), chemicals (corrosive substances), friction, or radiant and electromagnetic energy. Approximately 450,000 individuals seek medical attention for burn injuries annually in the United States, with 10% necessitating acute hospitalization.1 In recent decades, associated mortality rates have decreased significantly, with most patients achieving excellent functional and cosmetic outcomes. Improved outcomes have been attributed to the delineation of pathophysiologic mechanism of burns, advances in management, and the development of a comprehensive, treatment-oriented approach to care.2–4 The American Burn Association in conjunction with the American College of Surgeons Committee on Trauma has been instrumental in promoting the development of burn centers.5 Advanced burn life support prehospital and provider courses have also been developed to provide evidence-based guidelines for the assessment and treatment of burn victims.6 To facilitate appropriate treatment decisions and recognize potential complications, an understanding of the pathophysiologic processes associated with the burn injury is vital.
Thermal Injury
Etiology, Incidence, and Mortality
Thermal injuries are burns caused by contact with or exposure to extremes of temperature. Over the past 6 decades the incidence of burn injuries in the United States has steadily decreased, with approximately 450,000 currently occurring annually,1 resulting in approximately 40,000 hospitalizations and 3120 deaths.7–10 The fire loss record in the United States is the worst in the industrialized world, with the fire-related mortality double that of most countries on a per capita basis. From 2005 to 2009, residential fires resulted in nearly $7 billion per year in property damage.11
A half century ago, burns over 50% of the total body surface area (TBSA) resulted in a greater than 50% mortality in pediatric patients.12 Currently, most children survive burns of this size, and more than half survive burns of more than 90% of their TBSA.13 Early mortality generally occurred as a result of inadequate initial resuscitation. As vigorous resuscitation protocols were developed, a significant reduction in mortality occurred. Additionally, many advances have also contributed to decreasing thermal burn–related mortality, including: a better understanding of the pathophysiologic mechanisms of burns, implementation of a multidisciplinary team–oriented approach, improvement of resuscitation strategies and infection control measures, use of early surgical excision and skin-grafting techniques, application of advances in skin substitute development, and employment of improved rehabilitation strategies.14–18
Unfortunately, the reduction in mortality was replaced by an increased number of survivors with wound sepsis. The development of improved topical and systemic antimicrobial agents, recognition of the importance of maintaining proper nutrition, and adoption of early wound excision and grafting techniques have resulted in a significant reduction in mortality. As a result of these advances, acute mortality in patients with thermal injuries remains relatively low. The primary cause of death in this population now occurs in the subacute setting as a result of pulmonary sepsis, often developing secondary to inhalation injury. More than 80% of patients sustaining burns have involvement of less than 20% of their TBSA and are treated on an outpatient basis. Despite burn degree, the associated physical and emotional sequelae are often extensive and prolonged. As a result, this unique population requires vigilant follow-up care.
Risk Factors
The U.S. Centers for Disease Control and Prevention (CDC) has identified the following groups as being at high risk for fire-related injuries and deaths: children younger than 4 years; adults 65 years and older; Native Americans and African Americans; economically challenged individuals; people living in rural areas; and those residing in manufactured homes or substandard housing. Children younger than 15 years old account for one third of all admissions to burn units and one third of all deaths from burns and burn-related injuries.8 Scald injuries, primarily secondary to accidental spills, or in up to 20% from an element of abuse or neglect, account for up to 65% of all burn injuries.4,12,19 See Figure 54-1 illustrating an abuse burn.
The population older than 65 years of age accounts for approximately 29% of all burn/fire-related deaths in the United States.20 Burns in the elderly carry a high mortality rate as a result of preinjury disability, age-related immunosuppression, and impaired healing responses (Table 54-1).8 Environmental and lifestyle factors influence the frequency and magnitude of thermal burn injuries. Alcohol and drug abuse contributes to approximately 40% of all residential fire-related deaths. Neurologic and psychiatric disorders have also been found to increase the risk of accidental burn injury, with one study finding 3% of patients admitted to the burn unit had thermal injuries associated with neurologic disorders.
TABLE 54-1
PHYSIOLOGIC CHANGES ASSOCIATED WITH AGE
| BODY SYSTEM | PEDIATRIC | ELDERLY |
| Cardiovascular | Symptoms of shock: Increased heart rate Decreased blood pressure Decreased urine output Cardiac output dependent on heart rate Decreased myocardial compliance Stroke volume plateaus at lower filling pressures Peripheral cyanosis: Neonates: a normal finding Children: decreased cardiac output | Increased chronic disease processes Decreased vascular elasticity results in increased systolic blood pressure Decreased cardiac output Decreased β-adrenergic responsiveness Decreased cardiac stress response Decreased intrinsic heart rate Decreased blood flow Decreased vascular permeability Increased myocardial irritability Decreased myocardial perfusion Increased dysrhythmias Conduction system changes |
| Pulmonary | Small trachea is easily obstructed Neck hyperextension leads to epiglottal or tracheal obstruction At <8 yr, cricoid cartilage is narrowest airway point At <8 yr, no cuff is needed on endotracheal tube Hypoxemia leads to decreased heart rate in neonates Hypoxemia leads to decreased heart rate in children Diaphragmatic breathing Lower airways are easily obstructed Decreased O2 reserve | Increased need for ventilatory support Increased incidence of inhalation injury Increased pneumonia Decreased lung elasticity Decreased chest wall muscle Decreased oxygen saturation Decreased tidal volume Decreased vital capacity Decreased pulmonary capillary circulation |
| Thermoregulation and metabolism | Increased resting metabolic rate Increased resting O2 consumption Increased BSA in relation to body weight Increased hypothermia Increased heat loss from evaporation and convection At <6 mo, inability to shiver to increase body heat Stress leads to hypoglycemia Glycosuria is a sign of infection At <2 yr, buffering capacity is decreased Increased metabolic demands of growth | Increased burn wound infection Increased sepsis Poor or delayed wound healing Increased preexisting malnutrition Decreased febrile response Increased hypothermia |
| Gastrointestinal and renal | Decreased endogenous calorie stores Increased diarrhea with fluid and calorie deficits At <2 yr, gastric emptying is delayed At <2 yr, increased gastric distention At <30% TBSA burn, can take sufficient caloric supplementation At >30% TBSA burn, requires caloric supplementation At <12 mo, poor renal filtration and absorption | Increased volume sensitivity Decreased nutritional status Increased likelihood of hypotensive or hypertensive renal damage Increased incidence of type 2 diabetes mellitus Decreased creatinine clearance |
| Neurocognitive | Increased incidence of cerebral edema with fluid resuscitation Increased irritability Increased regressive behavior Increased risk-taking behavior Immature judgment | Decreased brain mass Decreased cerebral nerve cells Decreased brain cortex layer Decreased cerebellar cortical cells Decreased nerve conduction velocity Decreased memory Decreased electroencephalographic activity Slower reaction time Decreased taste Decreased smell Decreased vision Decreased hearing Increased pain threshold Decreased judgment and cognitive abilities |
| Immune | Immature immune system Decreased immunocompetence | Decreased number of leukocytes Decreased immunocompetence Decreased T-cell response |
BSA, Body surface area; mo, month(s); TBSA, total body surface area; yr, year(s).
From Carrougher GJ, editor: Burn care and therapy, St Louis, 1998, Mosby, p 100.
Integument Effects
The skin is the largest organ of the body and constitutes approximately 20% of the total body weight. It consists of two layers, the epidermis and dermis, which rest on the hypodermis (or subcutaneous layer). The epidermis contains two main cell types, melanocytes and keratinocytes, as well as multiple appendages such as hair, nails, and glands (sweat and sebaceous). The appendages, although originating from the epidermal layer, are anatomically located in both the epidermis and the dermis. Keratinocytes synthesize keratin, and melanocytes scattered throughout the basal layer (stratum germinativum) produce melanin, a pigment that shields deeper structures of the skin from sunlight. Apocrine glands, the large sweat glands, are rudimentary structures with no known useful purpose. They respond to autonomic nerve stimulation rather than thermal stimulation to produce an odorless, viscous, milklike droplet from the hair shaft. Apocrine glands are more numerous in women and are located in the axilla, areola of nipples, groin, perineum, and perianal and periumbilical regions. Eccrine glands are small sweat glands distributed over the body that act as true secretory glands and produce the sweat responsible for heat regulation. At environmental temperatures greater than 31° or 32° C (90° F), sweating occurs over the entire body; at lower temperatures, microscopically visible droplets are secreted periodically as part of the total insensible water loss from the body. Sweat normally provides skin with an acid mantle (average pH, 5.7 to 6.4) that retards growth of the many bacteria that reside in the keratin layer, glands, and hair follicles.
Sebaceous glands secrete sebum, a complex mixture of lipids that is emptied into the hair shaft. The rate of production of sebum and its location depend on androgens, which initiate and continue production. During the hypermetabolic state that follows major thermal injury, production of sebum is decreased, leading to the dry skin conditions commonly found after recovery.
Thermal injury to the integument occurs in two phases: (1) immediate, which is a result of direct cellular injury and (2) delayed, which occurs as a result of progressive dermal ischemia.
The duration of exposure and the temperature, or the amount of energy, to which the skin is exposed primarily determines the degree of tissue/cellular injury, which is characterized by three zones (from inner to outer): (1) zone of necrosis; (2) zone of stasis, which is a region with decreased blood flow that either can be returned to its normal state with appropriate resuscitation or can be converted to a necrotic state in the case of dehydration, infection, or decreased perfusion; and (3) zone of hyperemia, which is minimally injured tissue that usually recovers normal function within 1 week.21
In response to thermal injury, keratinocytes develop from cells in the basal layer of the epidermis and progress upward from the stratum germinativum to the stratum corneum over a 14-day period. During this time the wound develops a light pink or reddish coloration, with normal skin color restored in a delayed fashion by the melanocytes. Regeneration of hair and nails is dependent on viability of the hair follicle and nail matrix. With intact follicles, hair generally regrows at approximately 1 cm per month. New nail formation is often irregular and of abnormal thickness as regrowth occurs.
Depth Classification
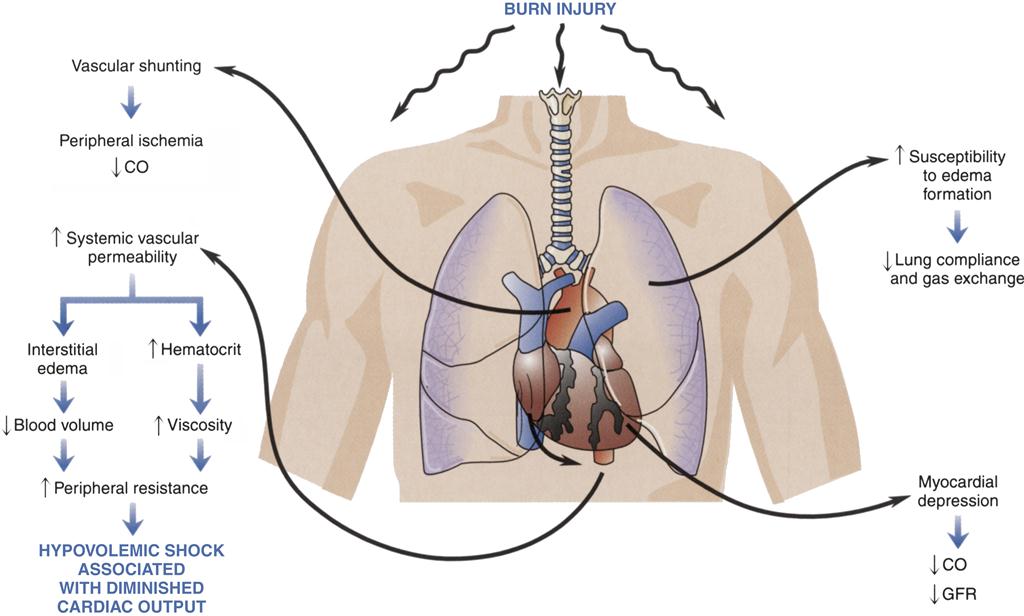
Depth of burn injury is divided into four classifications: first-degree burns, also known as superficial burns, second-degree burns, also known as superficial and deep partial-thickness, third-degree burns (full-thickness), and fourth-degree burns (full-thickness with bone or muscle involvement), based on criteria established by the American Burn Association (Table 54-2).22
TABLE 54-2
| DEGREE OF BURN | CAUSE OF INJURY | DEPTH OF INJURY | WOUND CHARACTERISTICS | TREATMENT COURSE |
| First-degree burn | Prolonged ultraviolet light exposure, brief exposure to hot liquids | Limited damage to epithelium, skin intact | Erythematous, hypersensitive, no blister formation | Complete healing within 3-5 days without scarring |
| Superficial partial-thickness burn: second degree | Brief exposure to flash, flame, or hot liquids | Epidermis destroyed, minimal damage to superficial layers of dermis, epidermal appendages remain intact | Moist and weepy, pink or red, blisters, blanching, hypersensitive | Complete healing within 21 days with minimal or no scarring |
| Deep partial-thickness burn: second degree | Intense radiant energy, scalding liquids or hot semiliquids (e.g., tar) or solids, flame | Epidermis destroyed, underlying dermis damaged, some epidermal appendages remain intact | Pale, decreased moistness, blanching absent or prolonged; intact sensation to deep pressure but not to pinprick | Prolonged healing (often longer than 21 days), may require skin grafting to achieve complete healing with better functional outcome |
| Full-thickness burn: third degree | Prolonged contact with flame, scalding liquids, steam; hot objects; chemicals; electrical current | Epidermis, dermis, and epidermal appendages destroyed; injury through dermis | Dry, leatherlike; pale, mottled brown, or red; thrombosed vessels visible; insensate | Requires skin grafting |
| Full-thickness burn: fourth degree | Electrical current, prolonged contact with flame (e.g., unconscious victim) | Epidermis, dermis, and epidermal appendages destroyed; injury involves connective tissue, muscle, and possibly bone | Dry; charred, mottled brown, white, or red; no sensation; limited or no movement of involved extremities or digits | Requires skin grafting, amputation of involved extremities or digits likely |
From Carrougher GJ, editor: Burn care therapy, St Louis, 1998, Mosby, p 138.
First-degree burns (also known as superficial burns) involve only superficial tissue destruction in the outermost layers of the epidermis, with no associated compromise of the function of the skin (see Table 54-2). These burns are often associated with local discomfort, erythema, and mild systemic responses such as headache, chills, nausea, and vomiting. Erythema, a thermovascular response that occurs in first-degree burns in the absence of direct trauma to the dermis, is probably related to the release of tissue contents into the superficial circulation. First-degree burns are generally self-limiting, require no fluid resuscitation, and are therefore not included in estimates of the percentage of TBSA burned. However, in infants and elderly adults, first-degree burns may lead to systemic dehydration, necessitating intravenous resuscitation. Therapy generally includes simple analgesia. These injuries typically heal in 3 to 6 days without scarring or pigmentation changes.
Second-degree (superficial partial-thickness) burns involve the epidermis to the level of the dermis and appear red to pale ivory. Moist, thin-walled blisters often form within minutes of the injury (Figure 54-2). Pain is a major clinical feature of this depth of injury because tactile and pain sensors remain intact (see Table 54-2). Injuries typically heal in 7 to 21 days in the absence of wound infection. The amount of scarring that follows is a genetically determined trait, with some groups of people tending to scar excessively (African Americans and Caucasians with red hair) or minimally (Native American and Asian groups). Hair follicles remain intact and will regrow hair in the area of injury. Hair usually reappears 7 to 10 days after injury.
Second-degree (deep partial-thickness) burns may involve the entire dermis and leave only the epidermal skin appendages located in the hair follicles. The area of injury has a mottled appearance, with large areas of waxy-white tissue surrounded by light pink or red tissue. The surface is generally dry, and blisters tend to resemble flat, dry tissue paper rather than the fluid-filled raised areas seen with superficial partial-thickness injury. Tactile and pain sensors are either absent or greatly diminished in the area of deepest tissue destruction, but this area is usually surrounded by margins of lesser depth of injury in which pain and tactile sensors remain intact. Deep partial-thickness injury is visually and clinically indistinguishable from full-thickness injury at the time of injury. These wounds heal spontaneously in previously healthy individuals in about 4 weeks in the absence of secondary infection. As the length of healing time increases, so does the degree of scarring and depigmentation. As a result, these burns are often excised early and subsequently treated with a skin graft in an effort to diminish scarring and achieve early wound closure.
Third-degree (full-thickness) burns may also involve the entire epidermis, the dermis, and the underlying subcutaneous tissue. Immediately following injury, these areas appear white, cherry red, or black. Deep blisters may be present under a dry layer of dehydrated skin. Superficial blood vessels coagulated by the heat of injury may be visible through the skin as thrombosed veins. One of the physiologic characteristics of the skin that is lost (Box 54-1) is the elasticity of the dermis, resulting in a wound with a dry, hard, leathery texture. The massive edema that accompanies major burn injury combined with the loss of elasticity may result in a tourniquet-like effect when the injury occurs circumferentially around a limb or torso. This often necessitates escharotomies or, rarely, fasciotomies to restore distal circulation.
These burns are painless to touch, because all superficial nerve endings in the skin have been destroyed. However, as with partial-thickness injuries, rarely are burn injuries totally uniform, and an area of lesser injury in which pain and tactile sensors are intact is usually located on the periphery. Areas of full-thickness injury require skin grafting with the patient’s own skin because all dermal elements have been destroyed, leaving no residual tissue for regeneration. However, small injuries often heal by secondary intention as a result of ingrowth of dermal elements from the margins of the wound.
Fourth-degree (full-thickness) injuries that extend beyond the dermis to involve muscle, bone, or both are often classified as fourth-degree. These injuries often occur in victims of high-voltage electrical injury or in persons who have had prolonged exposure to intense heat, such as unconscious fire victims.
Extent of Injury
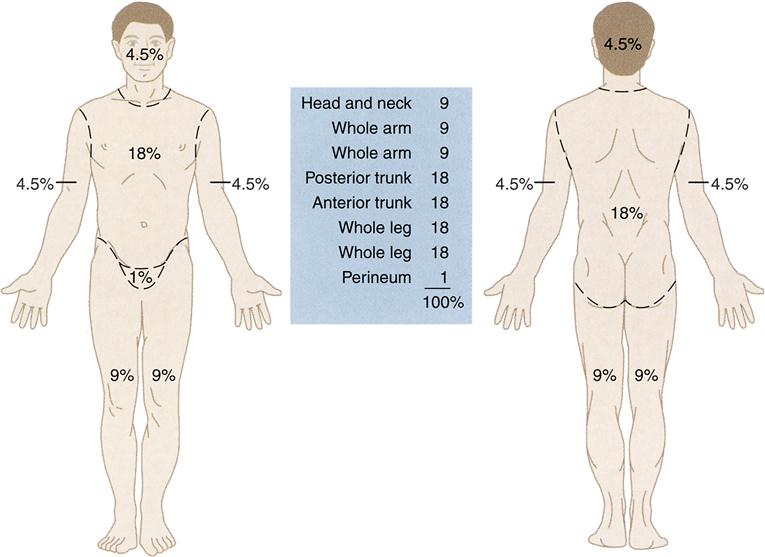
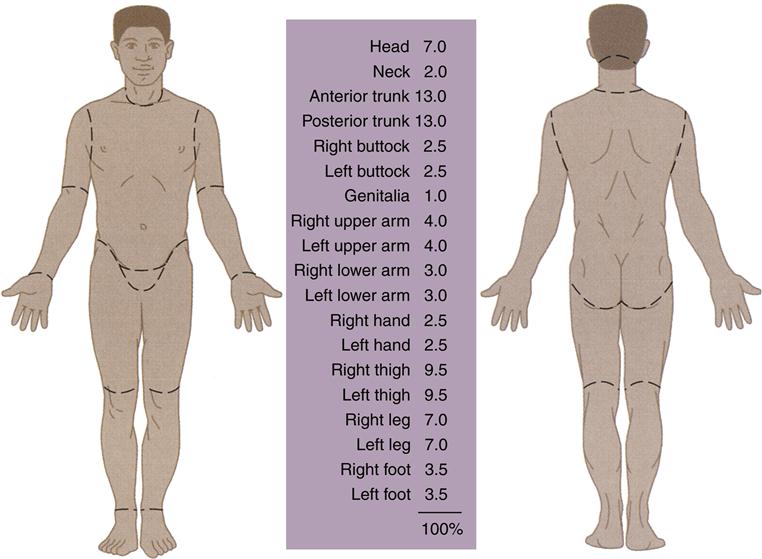
Extent of injury refers to the percentage of TBSA burned. Estimates can be calculated with the rule of nines (Figure 54-3) or the Lund and Browder chart (Figure 54-4). The rule of nines is commonly used in prehospital settings and emergency departments, and provides a rough estimate of TBSA involved. The Lund and Browder chart, or a variation of it, is generally used in burn centers and is more precise, particularly in assessing TBSA in children under the age of 10 years (see Figure 54-4).
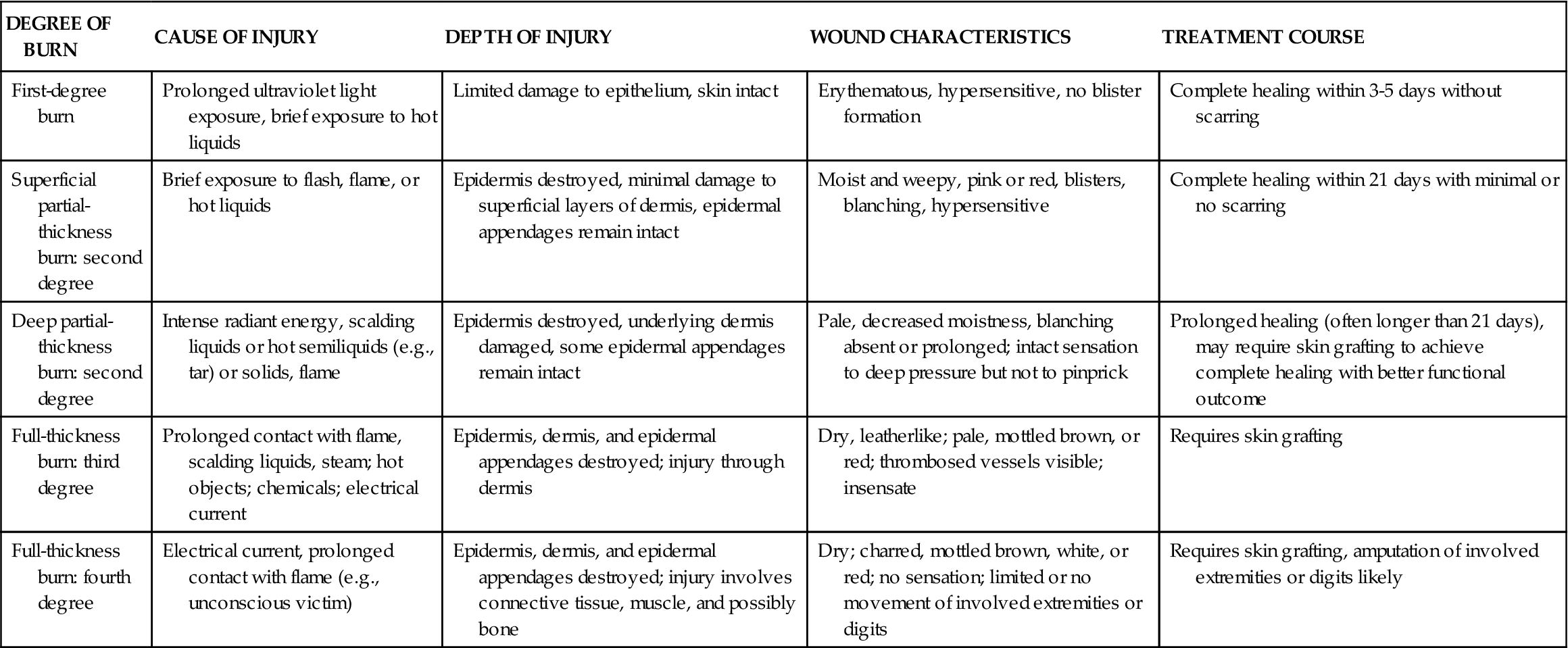
Severity Classification
The severity of a burn injury is determined by the extent to which the physiologic functions of the skin are disrupted beyond the body’s normal ability to respond with compensatory mechanisms. The American Burn Association22 classifies burn injury as minor, moderate, and major (Table 54-3). The severity of the burn injury and the eventual morbidity and mortality associated with it are related to a combination of factors: the patient’s medical history, the extent and depth of the burn, the body area involved, the presence of concomitant trauma sustained at the time of the burn, and the patient’s age.
TABLE 54-3
AMERICAN BURN ASSOCIATION BURN SEVERITY CLASSIFICATION SCHEDULE
| CLASSIFICATION | ASSESSMENT CRITERIA |
| Minor burn injury | <15% TBSA burn in adults <40 yr old |
| <10% TBSA burn in adults >40 yr old | |
| <10% TBSA burn in children <10 yr old | |
| and | |
| <2% TBSA full-thickness burn without risk of cosmetic or functional impairment or disability | |
| Moderate burn injury | 12-25% TBSA burn in adults <40 yr old |
| 10-20% TBSA burn in adults >40 yr old | |
| 10-20% TBSA burn in children <10 yr old | |
| and | |
| 10% TBSA full-thickness burn without cosmetic or functional risk to burned area involving face, eyes, ears, hands, feet, or perineum | |
| Major burn injury | >25% TBSA burn in adults <40 yr old |
| >20% TBSA burn in adults >40 yr old | |
| >20% TBSA burn in children <10 yr old | |
| or | |
| >10% TBSA full-thickness burn (any age) | |
| or | |
| Injuries involving face, eyes, ears, hands, feet, or perineum likely to result in functional or cosmetic disability | |
| or | |
| High-voltage electrical burn injury | |
| or | |
| All burn injuries with concomitant inhalation injury or major trauma |
TBSA, Total body surface area.
Modified from American Burn Association guidelines. In Carrougher GJ, editor: Burn care and therapy, St Louis, 1998, Mosby, p 94.
Acute Management
The first priority in burn management is the elimination of the source; however, extreme caution must be exercised to ensure that the rescuer does not become a victim. The fire should preferably be extinguished with water, because it not only eliminates the source of the heat but also enables cooling of the underlying skin. In the absence of water, flames may be smothered with a blanket, coat, or any other nonflammable covering that will aid in deprivation of the oxygen required for combustion. Once the flames are eliminated, the cover should be promptly removed to enable dissipation of the underlying heat, thereby minimizing injury depth. Scald injuries are best treated initially with cool water, which allows cooling of the scalding liquid as well as the underlying skin.
Assessment
Initial management of patients with thermal burn injuries should focus on stabilizing the ABCs (airway-breathing-circulation).4 Common signs of inhalation injury include cough, stridor, hoarseness, singed nasal hair, carbonaceous sputum, oropharyngeal edema, and blisters. These injuries generally evolve over time, often progressing to complete airway obstruction secondary to edema. Unfortunately, no clinical variables accurately predict which patients will progress to airway compromise; therefore consideration should be given early to bronchoscopy and endotracheal intubation.23 Compromise of breathing in burn patients is often attributed to underlying inhalation injury or circumferential full-thickness burns resulting in impaired chest excursion; however, breathing difficulties may also arise from associated pneumothorax, hemothorax, or chest wall instability from multiple segmental fractures (flail chest). Vascular access is preferentially obtained peripherally through unburned tissue if possible. If no such sites are available, access may be established through burned skin. The patient is then evaluated by a complete head-to-toe examination for any other associated traumatic injuries, which are identified and managed as required. TBSA is then determined using a standardized chart such as the Lund and Browder chart (see Figure 54-4). Fluid resuscitation requirements are subsequently determined and initiated while the patient is placed on clean sheets and the burned areas covered with dry clean sheets or dressings. Coverage with cool wet sheets should be avoided, because these quickly become cold wet sheets, and with the loss of the burned skin’s ability to regulate body temperature, hypothermia can quickly ensue. Application of topical agents in the acute setting outside of a burn center is not recommended. A Foley catheter is also placed to monitor urine output during resuscitation, and in patients with burns greater than 20% of the TBSA, if possible, a nasogastric tube should be placed to allow for gastric decompression and to minimize the risk of abdominal bloating and aspiration. Transfer of patients to burn units or other facilities with appropriate resources is initiated during the course of the initial assessment. The American College of Surgeons Committee on Trauma has developed a set of burn unit referral criteria to assist initial evaluators in triage (Box 54-2).
Burn Shock and Acute Resuscitation
Two different, but simultaneous mechanisms occur in cases of major burns: local wound pathophysiologic processes related to the loss of skin integrity and systemic pathophysiologic processes related to sequelae of the burn injury.
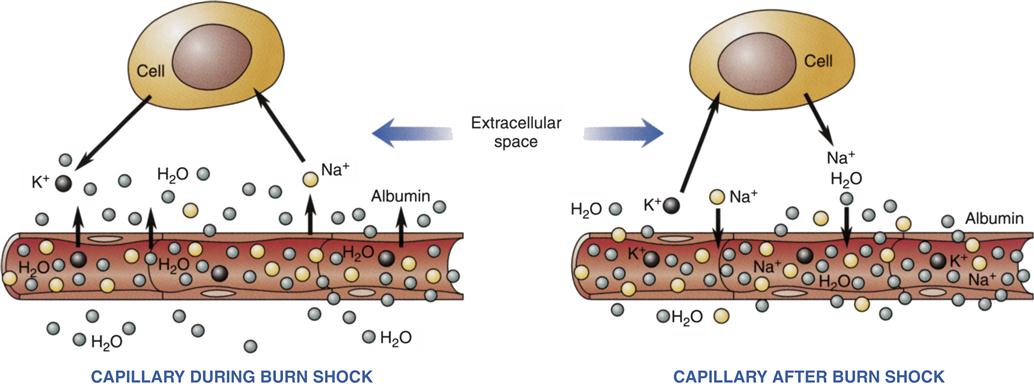
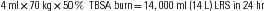
Within minutes of a burn injury, the cardiovascular system, which is normally a closed, semipermeable system, becomes an open system through which the patient’s circulating volume leaves the circulatory system. This phenomenon, known as “capillary leak,” occurs within a few minutes of injury and persists for 24 hours. Burn shock is not confined to the burn area but, rather, is a systemic process. While the capillary system throughout the body becomes leaky, fluid lost in the area of the burn leaks through the burn into the environment in an evaporative fashion, whereas fluid loss internally collects in the nearby soft tissues, producing extensive interstitial edema (Figure 54-5).
Restoration of the patient’s circulating volume is an essential part of acute burn management. The rate and volume of fluids lost are related directly to the severity of burn. Therefore, the extent and depth of the burn injury must be ascertained during the initial clinical assessment.
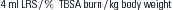
The most widely used formula to guide fluid resuscitation within the first 24 hours of burn injury is the Parkland formula (Box 54-3). The formula utilizes lactated Ringer solution as the resuscitation fluid, because it most closely approximates the fluid it is replacing and thereby minimizes the profound electrolyte imbalances often seen with large-volume resuscitation (Box 54-4). The standardized formulas provide an excellent guideline for initiating fluid resuscitation but do not ensure adequacy of resuscitation. In Cartotto’s series, 30 patients with mean TBSA burns of 27% received 6.7 ± 2.8 ml/kg/% TBSA burn in the first 24 hours to ensure adequate resuscitation.24 Adequacy of resuscitation is determined by the global response of the patient to the fluid administration and not by one single variable.25 Markers commonly used to reflect adequacy of resuscitation include normalization of mental status, blood pressure, pulse rate, capillary refill time, arterial pH, and base deficit and maintenance of urine output at 0.5 to1 ml/kg per hour for adults and 1 to 1.5 ml/kg per hour for children. In addition to the fluid volumes calculated by the standardized formulas, the patient should also receive appropriate maintenance fluid over the first 24-hour period.
Approximately 24 hours following the acute burn injury, the capillary leak syndrome begins to resolve as cardiovascular integrity is restored. At this time, a colloid solution such as albumin may be administered according to an appropriate formula, which differs by gender and age (see Box 54-4), in an effort to replace the protein lost during the acute burn shock phase. Resuscitation in the acute setting with colloid has been shown to decrease net volume of fluid administered and complications associated with large-volume resuscitation such as abdominal compartment syndrome.26
One of the major functions of intact skin is to serve as a barrier to water evaporation. With major burn injury, this ability of the skin to regulate evaporative loss is disrupted. In a classic study conducted in 1962, Moncrief and Mason27 attempted to determine the magnitude of such a loss and found that daily evaporative loss was in the range of 20 times normal during the early phase of burn injury, with gradual decreases as wound closure was achieved. Further studies revealed that the insensible water loss through burned skin is not caused by evaporation of water from sweat glands but rather by water vapor formed within the body and lost through the skin.28,29 As the patient progresses to the subacute phase of resuscitation, it is imperative that attention be paid to these unaccountable losses.
Patients at the extremes of age groups require special considerations with respect to resuscitation. Table 54-1 summarizes the physiologic changes associated with age that increase the vulnerability of children and elderly persons.30–32
Organ Dysfunction
Cardiovascular Dysfunction
Burn shock is often accompanied by a precipitous drop in cardiac output that does not parallel the gradual reduction in blood volume and is refractory to restoration of the circulating volume. This finding of low cardiac output in the presence of vigorous intravenous fluid resuscitation and massive catecholamine release has led to the suggestion of a specific myocardial depressant factor.33–38 The pathophysiologic mechanism behind this myocardial dysfunction is poorly understood. There appears to be no simple, specific myocardial depressant factor but rather a cascade of events involving metabolic and immunologic factors (Figure 54-6).19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree