Figure 74-1. The adult female breast. The upper and medial portions of the breast rest on the pectoralis major muscle, and the inferolateral portion rests on the serratus anterior.
Lymphatic Drainage
The lymphatic flow from the breast is unidirectional through thin-walled, valveless vessels that are interconnected through three groups. The primary group of lymphatic vessels comes from within the gland in the interlobular spaces and along the lactiferous ducts. The lymphatic vessels that drain the skin, nipple/areola, and the central portion of the gland constitute the subareolar plexus. The third plexus is on the deep surface of the breast and communicates with small vessels in the deep fascia underlying the breast. More than 75% of the lymph from the breast passes to the axillary lymph nodes, whereas the remainder passes to parasternal nodes. The flow of lymph to either the axillary or the parasternal nodes is independent of the quadrant from where the lymph originated.5 Occasionally, lymph flow can be found outside of these three interconnected plexuses, occurring along the lateral cutaneous branches of the posterior intercostal arteries, within the rectus sheath or subperitoneal plexus by following branches of the intercostal and musculophrenic vessels, or directly to subclavicular or apical nodes.6

Figure 74-2. The breast consists of 15 to 20 lobes of glandular tissue. Within each lobe, the lobules are composed of branched tubuloalveolar glands. Each lobule ends in a lactiferous duct. These ducts dilate into lactiferous sinuses beneath the nipple.

Figure 74-3. The axillary lymph nodes are divided into three levels by the pectoralis minor muscle. The level I nodes are inferior and lateral to the pectoralis minor, the level II nodes are below the axillary vein and behind the pectoralis minor, and the level III nodes are medial to the muscle against the chest wall.
The axilla is a pyramidal compartment between the upper extremity and the thoracic walls, which can be thought of as consisting of four walls, an apex, and a base. The anterior wall consists of the pectoralis major/minor and its associated fasciae. The subscapularis muscle, teres major muscle, latissimus dorsi muscle, and associated tendons form the posterior wall. The medial wall consists of the serratus anterior muscle and associated intercostal muscles of the upper four or five ribs. A thin strip of the humerus and the bicipital groove, which is between the insertion of the muscles of the anterior and posterior walls, forms the lateral wall. The apex is an aperture that extends into the posterior triangle of the neck through the cervicoaxillary canal, which is bounded by the clavicle anteriorly, the scapula posteriorly, and the first rib medially. The base of the axilla is the axillary fascia and the skin.6
The axillary lymph nodes have traditionally been divided into three levels, corresponding to their location relative to the pectoralis minor (Fig. 74-3). Level 1 nodes (external mammary, axillary vein, and scapular lymph node groups) are inferior and lateral to the pectoralis minor; level 2 nodes (central lymph node and some subclavicular lymph node groups) are behind the pectoralis minor; and level 3 nodes (subclavicular lymph node group) are medial to the pectoralis minor. The interpectoral nodes (Rotter nodes) are located between the pectoralis major and minor muscles along the lateral pectoral nerve. The supraclavicular nodes are contiguous with the apex of the axilla. The internal mammary nodes are located in the first six intercostal spaces within 3 cm of the edge of the sternum, with the highest concentration of nodes found in the first three intercostal spaces.7,8

Figure 74-4. Tanner stages of breast development.
BREAST PHYSIOLOGY
Breast Development
As epidermal appendages, mammary glands likely evolved from ancient apocrine glands that were associated with hair follicles.9 The mammary gland is a complex secretory organ consisting of multiple different cell types. Epithelial cells form the ductal network of the gland, which is embedded within a fat pad composed of adipocytes. In addition, there are vascular endothelial cells that make up the blood vessels, stromal cells including fibroblasts, and immune cells. During the three stages of mammary development (embryonic, pubertal, and pregnancy/lactation), these cells undergo an intricate series of changes under the regulation of hormones and regulatory factors, resulting in permanent changes to the mammary gland that both modify its architecture and biologic characteristics.10 Understanding breast development and morphology is extremely important to the study of both premalignant and malignant conditions.
In humans, mammary gland development starts in the sixth week of fetal life with the formation of bilateral milk lines or ectodermal thickenings that extend from the axilla to the groin. These ridges rapidly regress except for those of the thorax, where invagination of ectoderm cells into the mesenchyme results in mammary bud formation. In the human embryo, at about 5 months, the deep layer of the mammary bud epithelium starts to proliferate and produces about 10 to 25 secondary buds, which will later correspond to lactiferous ducts. Canalization, or the formation of lumens within the solid core of these epithelial structures, occurs later in development. By birth, six to eight of these ducts are patent and empty into the nipple.11–15 A parallel bundle of an additional 25 smaller ducts also appear and are the precursors to the milk-producing units of the breast.16 The subareolar lymphatic plexus also develops from the ectoderm in a similar fashion,17 while the nipple forms from the proliferation of the mesenchyme under the areola.14
In infants, only small ductal structures are seen within the stroma and during childhood, these structures continue to grow isometrically at a rate similar to the rest of the body until puberty.18 These initial stages of breast development are not dependent on sex steroids but are likely governed by numerous growth factors that regulate the epithelial-mesenchymal interaction, including Lef-1,19 parathyroid hormone-related protein, and the type 1 parathyroid hormone/parathyroid hormone-related protein receptor.20
During puberty, the female glands enlarge rapidly secondary to maturation of the ductal system into a lobuloalveolar system. This is characterized by thickening of the ductal epithelium, elongating ducts, and an increasing amount of periductal connective tissue. In addition, stem cells at the tips of the ductal tree form terminal end buds, which are highly proliferative and give rise to alveolar buds. In early puberty, these alveolar buds empty into a terminal ductal lobular unit and are referred to as lobules type 1. Under the influence of ovarian hormones (estrogen and progesterone), lobules type 1 will differentiate into lobules type 2, which are characterized by smaller but more numerous buds that are noted as ductules or alveoli. It has been postulated that each menstrual cycle fosters new budding that never fully returns to the baseline of the prior cycle.21,22 In addition to estrogen and progesterone, pubertal breast development is also dependent on other hormones and regulatory factors including prolactin, growth hormone, glucocorticoids, growth factors (hepatocyte growth factor, IGF-1, IGF-2, FGF, neuregulins especially heregulin), vitamin D receptor, metalloproteinases, and PTEN.23–28
As these developmental events are occurring, physical changes in the breast contour and the appearance of the nipple become evident and are illustrated as the five Tanner stages of breast development (Fig. 74-4).29
Menstrual Cycle
During a 28-day menstrual cycle, the mammary gland undergoes five histologic phases described by Vogel: proliferative (days 3 to 7), follicular phase of differentiation (days 8 to 14), luteal phase of differentiation (days 15 to 20), secretory (days 21 to 27), and then menstrual (days 28 to 2). The first phase starts with the proliferation of the mammary epithelium and is characterized by mitotic figures, a predominant eosinophilic cell type, dense stroma, and tight lumen. During the follicular phase, the epithelial cells start to differentiate with the appearance of multiple cellular types (luminal columnar basophilic, intermediate pale cells, and basal clear cells with hyperchromatic nucleus or myoepithelial cells). In the luteal phase, the prior dense stroma starts to loosen and the lumen starts to open with secretions. Also, the basal clear cells have prominent vacuolization, consistent with the known effects of progesterone on the glycogen content of cultured endometrial epithelium.30 The secretory phase is notable for active apocrine secretion from luminal cells and an edematous stroma. During the menstrual phase, the stroma returns to a dense and cellular form, the lumen distends with secretions, and the basal cells have extensive vacuolization.31 These five phases depict the morphologic changes that occur in the breast from normal ovarian hormone cycling during menses, further supporting the notion that the mammary gland is not a resting gland but one that is dynamic.
Pregnancy and Lactation
Although the pubertal phase is marked by significant lobular development, the mammary gland does not achieve full differentiation until after pregnancy and lactation. In early pregnancy, the distal ducts continue to proliferate, resulting in more lobules and more alveoli within each lobule. However, by midpregnancy, proliferation of the lobules ceases and instead alveolar cells begin to differentiate into acini by hypertrophy and the ability to secrete colostrum into the lumina of the ductules. By the third trimester, the acini become distended with colostrum and the breast’s connective tissue and fat become largely replaced by glandular proliferation. In addition, the connective tissue becomes infiltrated with plasma cells, lymphocytes, and eosinophils. There is also a marked increase in vascularity. The stage of lactogenesis or the ability to synthesize and secrete milk marks the final stage of maturation of the mammary gland (lobule type 4).32,33 Following lactation or during weaning, the mammary gland involutes with lobules type 4 returning to the prepregnancy state as lobules type 2 and 3.34,35
The hormones and regulatory factors that govern mammary development during pregnancy and lactation overlap with those previously discussed for pubertal breast development, with estrogen, progesterone, and prolactin playing chief roles. Other hormones and regulatory factors include intracellular signaling molecules (c-erbB, hox genes, cell–cell adhesion molecules such as E-cadherin, cell cycle protein cyclin D1, RANK-L, slug transcription factor), activins and inhibins including STAT5, hypothalamic peptides, thyrotropic-releasing hormone, and lactogenic hormones.36–43
Menopause
By menopause, the mammary gland is mainly replaced by fat as the glandular epithelium undergoes apoptosis. As such, the postmenopausal phase is characterized by a decrease in lobules and ducts.44,45
In summary, human breast development is a progressive process that is initiated during embryonic life, with glandular maturation starting at puberty, and attainment of full breast differentiation only with subsequent pregnancy and lactation.
CLINICAL EVALUATION OF THE PATIENT WITH BREAST DISEASE
Breast disease is an extremely common clinical problem. Most women who present to a breast health specialist will have benign breast disease. One of the primary goals of the evaluation is to determine whether the breast problem represents benign or malignant breast disease. With benign conditions, the goals are to reassure the patient and if indicated, provide symptomatic treatment. With a malignant condition, prompt evaluation and treatment should be undertaken, typically involving a multidisciplinary team including a breast surgeon, medical oncologist, and radiation oncologist. In this section, the tools that a clinician uses to evaluate patients with breast disease are discussed including the history, clinical breast examination (CBE), diagnostic imaging studies, and biopsy procedures.
DIAGNOSIS
Table 74-1 Medical History of a Breast Problem

As the first step in the evaluation of a breast problem, it is important to elicit a relevant history. This includes the specific history related to the presenting breast problem, as well as a more general history focused on assessing breast cancer risk. This includes age at menarche, number of pregnancies, number of live births, and age at first live birth. Family history and history of breast biopsy should also be elicited. Menopausal status (for premenopausal patients, the time in their menstrual cycle) and the use of any hormonal therapies should be assessed (Table 74-1).
Clinical Breast Examination
CBE is performed in both the sitting and supine positions (Fig. 74-5). The patient is disrobed from the waist up and then provided a front-opening gown. Visual inspection is first accomplished with the patient sitting upright with the arms relaxed to her side. The bilateral breasts are compared for size and shape. It is normal to find slight differences in breast size, with the left breast often slightly bigger than the right. Breast shape is also contrasted. Recent changes to breast size or alterations in breast shape can be concerning signs and need to be evaluated by the provider, as tumors located superficially can cause changes to the breast contour. The skin of the breasts is inspected for dimpling, edema (peau d’orange), and/or erythema. In cases of significant erythema and peau d’orange, the provider needs to consider the diagnosis of an inflammatory breast cancer (IBC) versus an infectious etiology. This is followed by close inspection of the nipples for symmetry. Although some women have a lifelong history of nipple inversion, any new history of nipple inversion needs to be regarded with a high index of suspicion. Next, the nipple–areola complex is evaluated for any eczematous changes or ulcerations (to suggest conditions such as Paget disease of the breast [PDB]). The patient is then asked to raise her arms to allow for a more complete visual inspection of the lower aspect of the breasts bilaterally. The visual examination is completed when the patient is asked to place her hands on the hips and then to contract the pectoral muscles. This allows for a final visual assessment of breast symmetry. Furthermore, tumors deep within the substance of the breast involving Cooper’s ligaments can result in skin retraction and can sometimes be seen best with contraction of the pectoral muscles.

Figure 74-5. Breast examination. A: The patient’s ipsilateral arm is supported by the examiner to relax the pectoral muscle while the axillary nodes are examined. B: Bimanual examination of the breast in the upright position. C: Bimanual examination in the supine position with the arm raised over the head.
With the patient remaining in the sitting position but now with the pectoral muscles relaxed, palpation of the regional lymph nodes of the neck, clavicles (infraclavicular and supraclavicular), and axilla is then performed. To best delineate the axillary lymph nodes, the patient should be examined with the ipsilateral arm supported. Attention is paid to evaluate the size, consistency (soft or firm), and characteristics (mobile or matted, tender or nontender) of the lymph nodes. Bimanual palpation of the breasts for masses and asymmetry completes the sitting examination.
The patient is then placed in the supine position with the ipsilateral arm raised above the head and the contralateral breast covered with the gown. The breast tissue is carefully palpated to evaluate for masses and asymmetry. It must be noted that generalized lumpiness is not a pathologic finding, with most normal breasts having more nodularity in the upper outer quadrants, at the inframammary ridge, and in the subareolar region. Comparing the breasts for symmetry by palpation may help discriminate benign findings from those that require additional evaluation. The area examined extends from the clavicle to the lower rib cage and medially from the sternal border to the midaxillary line. In addition, the axillary tail of the breast should be carefully palpated. The three search patterns that have been described are concentric circles, radial spoke method, and the vertical strip pattern (Fig. 74-6). As the first two methods can result in a less than thorough examination of the nipple–areola complex, we prefer the vertical strip pattern as it incorporates this area. Otherwise, with the other two search patterns, a separate examination of the nipple–areola complex needs to be performed.
Diagnostic Mammography and Breast Ultrasound
1A woman who has an indeterminate or abnormal CBE will typically benefit from a diagnostic imaging evaluation, which can include targeted ultrasound, mammography, and/or MRI. It is important to note that any clinically suspicious mass, even in the absence of an imaging abnormality, needs to be biopsied as up to 15% of breast cancers are mammographically occult.46
Soft tissue densities and clustered microcalcifications are two common mammographic findings suggestive of breast cancer. Soft tissue densities can appear as well-defined round/oval/lobulated masses, spiculated masses, irregular masses, or as areas of architectural distortion without an obvious mass (Fig. 74-7). Nearly 90% of spiculated soft tissue masses are associated with invasive cancer whereas well-defined solid masses are rarely predictive of malignancy. Microcalcifications can have benign or malignant features, with benign calcifications often appearing rim-like, large, coarse, smooth, round, and/or oval in appearance. Calcifications that are associated with malignancy tend to be smaller in size, ranging between 0.1 and 1 mm in diameter. They are typically clustered, numbering 4 to 5/ cm3. Histologically, these represent intraductal calcifications in areas of necrotic tumor or calcifications within mucin-secreting tumors. In addition, malignant microcalcifications can often appear in a granular or linear branching pattern, with the linear branching pattern being highly associated with malignancy (Fig. 74-8).

Figure 74-6. Clinical breast examination search patterns: vertical strip, radial spoke, and concentric circles.

Figure 74-7. Mammographic masses. A: Spiculated mass with calcifications. B: Lobulated mass with indistinct posterior margin. C: Well-circumscribed mass.
Breast ultrasound is another important diagnostic imaging modality for the evaluation of breast masses and/or mammographic abnormalities. Breast ultrasound is complementary to mammography and is particularly valuable for the evaluation of breast masses. Breast ultrasound can increase the sensitivity and specificity of mammography for detection of breast cancer.47 Ultrasound can differentiate a cystic mass from a solid one, characterize a palpable lesion that is not seen on mammography, and can assist with determining the actual size of a lesion. Ultrasonographic features that are used to characterize a lesion include shape (oval, round, lobular, irregular); margin (circumscribed, obscured, microlobulated, ill-defined, speculated); orientation (parallel or not parallel to skin); matrix echogenicity (anechoic, hypoechoic, hyperechoic); homogeneity (homogeneous, heterogeneous); and attenuation (indifferent, shadowing, enhancement).

Figure 74-8. Microcalcifications. The branching, irregular appearance is classic for ductal carcinoma in situ.

Figure 74-9. Comparison of core needle biopsy specimen (A) and fineneedle aspiration specimen (B). Only the core specimen can demonstrate the architectural detail.
Diagnostic MRI
Gadolinium contrast-enhanced MRI is complementary to mammography and breast ultrasound. It is not typically used for the evaluation of benign breast masses but does have a high sensitivity for detection of breast cancer. As such, MRI is most commonly used to evaluate extent of disease and exclude occult breast cancers in patients with newly diagnosed breast cancer. In a meta-analysis of 44 studies, the sensitivity and specificity of diagnostic breast MRI was determined to be 90% and 72%, respectively.48 The role of MRI in the evaluation of patients with newly diagnosed breast cancer is discussed in the section on Evaluation of the Patient with Breast Cancer.
Biopsy Procedures
Breast biopsy is one of the most common general surgery procedures performed in the United States. There are multiple different types of breast biopsy ranging from fine needle aspiration (FNA) biopsy to excisional biopsy. The different types of breast biopsy are discussed later.
Fine Needle Aspiration
FNA of the breast is the least invasive breast biopsy procedure. FNA can be used for both diagnosis and treatment and can be performed using palpation or image guidance. During FNA cells or fluids are removed from the breast using a small gauge needle (20 to 25 gauge). FNA is commonly used to sample suspicious breast and axillary lesions especially those that are palpable. Other indications include drainage of simple cysts and small abscesses. The patient is placed in the supine position on the examination table at a 30-degree angle with the arm of the involved side above the head. When lesions are lateral or in the axilla, the patient is positioned in the lateral decubitus position. Inframammary lesions may require an assistant to help retract the breast. For ultrasound guidance, the probe is positioned directly over the area of interest. As an example, for a breast cyst, the probe would be placed directly over the cyst with the cyst located at the side of the probe; this way the shortest distance to the cyst is shown. Prior to aspiration, the cyst is thoroughly scanned in all planes for septa or loculations to facilitate complete aspiration. The skin is then prepped with an antiseptic solution and further scanning is performed in a sterile fashion. With the nondominant hand steadying the cyst, 1 to 2 mL of 1% lidocaine is injected into the skin. A 20-gauge needle with a 5 or 10 mL syringe is inserted in a plane parallel to the chest wall directly toward the center of the cyst. The plunger is then slowly retracted to create a vacuum to aspirate the cyst contents. For palpable lesions not requiring ultrasound guidance, aspiration can be performed in a similar fashion. The aspiration site can be dressed with an adhesive bandage. If there is bleeding, pressure is applied for 15 minutes. Other potential complications include infection and failure to adequately sample the area of concern. In institutions with experienced cytopathologists, diagnostic FNA has a reported sensitivity of 98% and a specificity of 97%.49 However, as the tissue architecture cannot be evaluated by FNA, the diagnosis of invasive cancer cannot be made. In the past, FNA was commonly used to sample palpable breast masses as part of the Triple Test for evaluation of palpable masses. Currently, ultrasound can more accurately assess these lesions and low suspicion lesions are followed with serial imaging. High suspicion lesions are best sampled by core needle biopsy to allow assessment of tissue architecture (Fig. 74-9).
Core Needle Biopsy
2 Core needle biopsy is also a minimally invasive strategy for breast biopsy. Given the limitations of FNA, core needle biopsy allows for more tissue to be sampled, permitting a histologic diagnosis, and offering the ability to discriminate between invasive and noninvasive breast cancer. Core needle biopsy can be performed by palpation, but ultrasound-guided core needle biopsy typically offers superior results. Ultrasound imaging and patient preparation are similar to that described for patients undergoing FNA. The skin and planned needle tract are anesthetized with lidocaine, and a small stab incision is made with a No. 11 blade prior to needle entry. A common core biopsy device consists of a hollow 14-gauge needle (range: 18-gauge to 11-gauge) with a spring firing mechanism. More advanced devices have vacuum assistance and an automated firing mechanism. Under ultrasound guidance, the tip of the needle is guided toward the lesion, often to its edge as the needle excursion is typically approximately 2 cm. Advancing the needle beyond the abnormality can result in sampling error and/or injury to the chest wall. The device is then fired and the needle is withdrawn, with the resultant “tissue core” placed into formalin. Three tissue cores are obtained to ensure adequate sampling of the abnormality. A clip is then deployed under ultrasound guidance to mark the biopsy site for future reference. For palpable masses, the procedure can be performed without ultrasound guidance. The nondominant hand is used to steady the mass and is positioned perpendicular to the entry point of the needle device to avoid inadvertent needle stick injury.
For nonpalpable lesions that cannot be imaged by ultrasound but are present on mammography (most commonly microcalcifications), stereotactic core biopsy can be performed. Stereotactic techniques use the principle of triangulation, which allows the precise location of a breast lesion to be determined in three dimensions.50 The patient can be upright or prone depending on the machine. More commonly, the patient is placed in the prone position on the stereotactic table, which has an opening for the breast. A mammography unit is attached beneath the table and compresses the dependent breast. An initial scout image is obtained perpendicular to the compressed breast and evaluated. The skin overlying the area of interest is then prepped and anesthetized with lidocaine injected in the skin and along the planned needle path. Using a No. 11 blade, a small stab incision is made. The needle is then advanced through the skin puncture site and toward the center of the lesion on the basis of the computed calculations. The needle is advanced to the leading edge of the lesion and its position is verified by imaging. Following biopsy, repeat images are obtained to ensure that the area of concern has been adequately biopsied. The procedure may be repeated to obtain additional cores. Most stereotactic core biopsies are performed with vacuum assistance allowing for greater accuracy. If suspicious microcalcifications are biopsied, the samples can be examined with specimen imaging to ensure the presence of microcalcifications within the biopsy samples. At the completion of the procedure, manual compression is used to obtain hemostasis, and the skin nick is closed with adhesive strips with a transparent medical dressing. An ice pack and compression dressing can also be used.
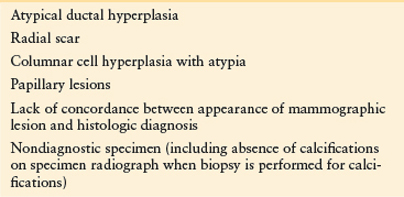
Failure to obtain an adequate sample can result in a false-negative test result, although the false-negative rate is very low. In some instances, the results of the core biopsy may not be definitive and a surgical excision is required. If the core biopsy demonstrates a concerning lesion, surgical biopsy is required to exclude a diagnosis of malignancy. In the clinical context of persistent suspicious physical examination or imaging abnormalities (discordance between clinical and/or imaging findings and pathology results), surgical excision is required. Please see Table 74-2 for indications for surgical excision after core biopsy.
Incisional Biopsy
Incisional biopsy typically involves surgical removal of part of a large mass for diagnosis. With the advent of core needle biopsy techniques, incisional biopsy is rarely required. However, if a core needle biopsy is nondiagnostic and the mass is too large to remove without significant cosmetic compromise, an incisional biopsy can be performed for definitive diagnosis.
INDICATIONS/CONTRAINDICATIONS
Table 74-2 Indications for Surgical Biopsy After Core Biopsy
Excisional Biopsy
Excisional biopsy of the breast is the surgical removal of a breast lesion. Although core needle biopsy has largely obviated the need for excisional biopsy for diagnostic considerations, indications for this procedure still remain. Indications include breast lesions that are presumed to be benign but require excision, discordance between clinical evaluation/diagnostic imaging and pathology requiring further tissue sampling, high-risk lesions (including atypical ductal hyperplasia, radial scar, and papilloma) identified on core biopsy, abnormalities that are close to the nipple or chest wall, small breasts that are not amenable to core biopsy (given the needle excursion is often 2 cm), and for patients who cannot tolerate stereotactic core needle biopsy. In addition, excisional biopsy may be considered for complex cysts, aspirated cysts that do not completely resolve, and when follow-up imaging for a lesion with previous benign pathology from a core biopsy shows an increase in size or has suspicious changes. Excisional biopsies may also be performed for likely benign lesions that are greater than 2 cm, painful, or recurring, or where the mass represents growing cysts or fibroadenomas. Patient preference for complete removal of a benign lesion may also be an indication for excisional biopsy.
For nonpalpable lesions, the abnormality can be localized preoperatively using a needle localization wire that is placed with the patient in a sitting position with the breast compressed by a labeled grid plate. Various needles used include the Kopans needle (check mark wire), the Hawkins needle (multiple barbs and the only retractable wire for repositioning), and the Homer needle (J wire and nontransectable needle). For lesions that are superficial and can be readily imaged by ultrasound, needle localization can be performed under ultrasound guidance. The patient is then taken to the operative setting, where excision of the lesion can be performed under local anesthesia with sedation or general anesthesia. In the operating room, the patient is placed in the supine position with the arm ipsilateral to the index lesion positioned at 90 degrees. Appropriate padding of the arm and wrists should be undertaken. The operative site is then prepped and draped in a sterile fashion. Intraoperative localization is performed by evaluating the imaging studies and palpating the needle (for nonpalpable lesions) or by direct palpation. For lesions located in the upper half of the breast, transverse or curvilinear incisions are made along Langer’s lines. If an incision is needed in the lower half of the breast, radial incisions are used. When possible, periareolar or inframammary incisions are made as they result in the best cosmesis. Prior to incision, a local anesthetic is injected into the skin and along the path of the needle localization wire. The incision is then typically made directly above the palpable mass or the tip of the needle (Fig. 74-10). Alternatively, an incision can be made next to the needle and then followed down to its tip to find the target lesion. Once the skin incision is made, the thickest possible flaps, which would still result in fully removing the lesion anteriorly, are developed. The specimen is then excised with electrocautery. The specimen is oriented with sutures, with the short stitch designating the superior margin and the long stitch designating the lateral margin. Palpation of the cavity is performed to ensure complete removal of the lesion. Specimen imaging is performed to confirm excision of the lesion of interest. The skin is closed in two layers. Cyanoacrylate tissue adhesive is then applied, allowing the patient to take a shower within 24 hours. For allergies to skin glue, adhesive strips can be applied. No pressure dressing is needed. A sports bra may be worn to stabilize the breast for the first 48 hours.
Skin Punch Biopsy
For any suspicious cutaneous lesion of the breast or chest wall, a biopsy can be obtained using a punch biopsy device, which consists of a circular blade. Punch biopsy devices are available in various sizes ranging from 1 mm to 8 mm, with the 2-mm and 4-mm size most commonly used in breast biopsies. The area to be biopsied is first selected. Common sites are the most abnormal-appearing site within a lesion or the edge of an actively growing lesion. The involved skin is cleansed and infiltrated with 2 to 3 mL of 1% lidocaine. The punch device is held vertically over the skin and rotated downward using a twirling motion until the subcutaneous fat or the hub of the device is reached. The specimen is then transected at the base with iris scissors. The skin is approximated with an interrupted stitch or U-stitch.

Figure 74-10. Incision placement for needle localization biopsy. A: The mammogram demonstrates that the lesion (arrow) is inferior to the point of wire entry. B: Incision placement inferior to wire entry to allow access to the lesion.
COMMON CLINICAL PROBLEMS AND MANAGEMENT ALGORITHMS
The most common clinical breast problems include breast masses, breast pain, nipple discharge, and breast infections. Clinical algorithms for the evaluation of these common breast problems have been developed to facilitate optimal care.
Breast Mass
A breast mass is defined as a palpable area in the breast that may be either benign or malignant. When a woman presents with a palpable breast finding, a thorough history and physical examination needs to be performed. The history should include a thorough review of the patient’s medical problems and any risk factors associated with breast cancer (see the section on Management of Patients at High Risk for Breast Cancer).
In women younger than 35 years with no family history of premenopausal breast cancer or other risk factors, a targeted ultrasound is an appropriate initial imaging approach for a breast mass that appears clinically benign (Algorithm 74-1). The ultrasound is used to determine whether a dominant mass is present, as normal glandular tissue of the breast, especially in young women, may feel nodular. In a review of 605 women younger than 40 years who were referred for evaluation of a breast mass, only 36% of the masses detected by patients had a surgical correlate. Furthermore, only 29% of the masses detected by primary care providers were confirmed.51 Consideration can then be made regarding the need for additional imaging such as mammography or an MRI. In women aged 35 years or older, the initial imaging approach to a palpable mass should include mammography and ultrasound. These studies should be obtained prior to any biopsies are performed as postbiopsy changes can distort subsequent imaging evaluation. Of note, all clinically suspicious palpable masses need to be biopsied even in the absence of imaging findings as 15% of breast cancers can be mammographically occult (Algorithm 74-2).46 Ultrasound also provides important information about the etiology of a breast mass and can further categorize the mass as either cystic or solid. Workup of a cystic lesion typically involves aspiration of the cyst, with further evaluation based on the results of the aspiration (Algorithm 74-3). The definitive diagnosis of a breast mass is often confirmed by a core needle biopsy, although FNA is an appropriate alternative (Table 74-3). Core needle biopsy is typically preferred to excisional biopsy.
TREATMENT
Table 74-3 Management of Breast Masses Based on Core Biopsy Diagnosis

Algorithm 74-1. Diagnosis and management of the patient with a clinically benign breast mass. The use of imaging studies varies according to age because breast carcinoma is infrequent in women younger than 35 years old.

Algorithm 74-2. Diagnosis and management of the patient with a clinically indeterminate or suspicious solid breast mass. In this circumstance, imaging studies are insufficient to exclude malignancy, and tissue sampling is required.1
Algorithm 74-3. Diagnosis and management of the patient with a cystic lesion. Bloody fluid on aspiration, failure of the mass to resolve completely, and prompt refilling of the same cyst are indications for surgical biopsy.
Breast cysts are common causes of dominant masses in premenopausal and perimenopausal women. If a cyst is found in a postmenopausal woman in the absence of hormone therapy use, it should be regarded with a high degree of suspicion. Palpable masses that present as benign solid masses include fibroadenomas, fibrocystic disease, and fat necrosis. Fibrocystic breast disease has been used to describe a variety of benign breast disorders associated with nodular breast tissue. This term, however, should be reserved for women who have a biopsy consistent with one of the histologic components of fibrocystic change. Breast surgery, blunt trauma, injection of native or foreign substance such as fat and silicone, and radiation therapy can result in fat necrosis. On clinical examination and mammographic imaging, fat necrosis can mimic a malignancy, often leading to a biopsy. However, when oil cysts, which are circumscribed masses of mixed soft tissue density and fat with a calcified rim, are present radiographically, a definitive diagnosis of fat necrosis can be made (Fig. 74-11). See the section on Benign Breast Disease.
Breast Pain
Breast pain (mastalgia, mastodynia, idiopathic breast pain) is a common concern and is rarely (0.5% to 3.3%) representative of a breast cancer. It is noted that some IBCs can present with pain. While two-thirds of patients present with cyclical breast pain, another one-third has pain that is unrelated to the menstrual cycle and more likely to be secondary to a breast or chest wall lesion.52
Cyclical breast pain is associated with hormonal changes during the menstrual cycle and often occurs the week prior to the onset of menses and often dissipates once menstrual flow is established. During the menstrual cycle, the breast undergoes significant histologic changes as described by Vogel et al. (see the section on Menstrual Cycle).31 During the secretory phase, luminal cells produce apocrine secretions and the stromal cells become edematous, which may contribute to the pathogenesis of breast pain. However, the exact physiologic events are not understood completely. Furthermore, while most women do experience mild cyclical breast pain, it is not clear why others have more pronounced pain. Cyclical breast pain is typically bilateral and involves the upper outer aspect of the breasts with radiation to the axillae or down the arms.
Noncyclical breast pain is more frequently unilateral and variable in its location in the breast. Possible etiologies include large pendulous breasts with pain resulting from stretching of the Copper’s ligaments, duct ectasia, macrocysts, medications (including antidepressants, hormones, and antibiotics), and infections.53,54 Thrombophlebitis of the lateral thoracic or superior thoracoepigastric vein (Mondor disease) is an uncommon presentation for breast pain characterized by a tender subcutaneous cord in the lateral aspect of the breast (Fig. 74-12). Mondor disease may result from trauma, radiation to the breast, and/or breast surgery. It can also occur in women with nonpalpable breast cancers, and a mammogram should be obtained when diagnosed.55 For symptomatic relief, a patient can use anti-inflammatory medications, although Mondor disease often resolves spontaneously without the need for a specific therapy. Referred pain to the breast from the chest wall or ribs can also occur. Spinal or paraspinal problems and medical conditions (biliary, pulmonary, esophageal, and cardiac disease) can also result in referred pain.

Figure 74-11. Oil cysts. The calcified rims of these cysts in a patient with a history of trauma are diagnostic.

Figure 74-12. Mondor disease. Thrombophlebitis of the thoracoepigastric vein causes retraction of the lateral portion of the breast, which crosses to the midline at the inferior areolar margin and is accompanied by a palpable cord.
The workup for breast pain should include a careful history, including questions related to the menstrual cycle, a thorough physical examination, and in women 35 years of age and older, a mammogram. If a malignancy is suspected, biopsy should be performed. If the CBE and diagnostic imaging studies are normal, reassurance that the symptoms are not consistent with breast cancer often provides significant relief for the patient.
Initial therapy for idiopathic breast pain includes lifestyle changes, the use of supportive garments such as a well-fitting brassiere with a steel underwire, a low-fat high-carbohydrate diet, and elimination of caffeine and nicotine. Oral analgesics with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) should be initiated. Topical analgesic gels containing diclofenac or salicylate can be applied to the affected breast areas. If a patient is on oral contraceptives or hormone replacement therapy, discontinuation of these medications may improve pain. However, in women not using oral contraceptives with cyclical breast symptoms, the initiation of this therapy has been shown to reduce breast pain severity and duration. Although inconclusive evidence exists for the role of evening primrose oil (3,000 mg daily),56,57 it is often part of the initial therapeutic approach. Evening primrose oil needs to be taken for at least 4 to 6 months to achieve a positive effect.
Approximately 5% of women will still have debilitating breast pain despite lifestyle changes and the initial therapies described above. For these women, therapies such as danazol, tamoxifen, bromocriptine, and gonadotropin-releasing hormone (GnRH) agonists can be considered. However, only danazol has been approved by the FDA for the treatment of idiopathic breast pain. Danazol (100 mg to 400 mg daily) is an antigonadotropin that results in a hypoestrogenic state. However, its use is often discontinued as it also induces a hyperandrogenic state, with most women having side effects of increased facial hair, acne, deepening of the voice, and adverse blood lipid profiles.58 Tamoxifen (10 mg daily) has also been shown to be effective although side effects, including the risk of blood clots, endometrial cancer, and hot flashes limit its use.59 As both danazol and tamoxifen have significant teratogenic effects, women on these therapies must be counseled to use an effective birth control method. Although bromocriptine and GnRH agonists have been studied for use in breast pain, they are not currently recommended because of significant side effects. Therapies that have been proven to be ineffective include diuretics, progesterone, and vitamins. Surgery to excise trigger spots (in the absence of an identifiable lesion) is not recommended, as the affected area is often replaced by a painful scar.
Nipple Discharge
Nipple discharge is a common breast symptom that often results in surgical consultation. The most common cause of pathologic nipple discharge is an intraductal papilloma, but breast cancer can also present as a pathologic nipple discharge. The first step in evaluation of nipple discharge is to determine whether the nipple discharge is pathologic or physiologic. Physiologic discharge is nonspontaneous or is elicited by manual compression of the nipple. It often involves multiple ductal orifices in the nipple and is present in both breasts. The discharge is commonly white or clear (although it can also present as yellow, green, brown, or gray fluid) and is negative on occult blood test. In contrast, pathologic nipple discharge is spontaneous, is present in a single breast/ductal orifice, and is often positive on occult blood test. However, any nipple discharge that is spontaneous is considered pathologic. Age is also predictive of breast cancer risk in women with nipple discharge. In a study involving women with pathologic nipple discharge, breast cancer was present in 3% of women younger than 40 years, 10% in those 40 to 60 years of age, and 32% in those older than 60 years.60
Clinical evaluation of nipple discharge includes a careful history and physical examination. The history includes questions regarding whether the discharge is spontaneous or elicited, unilateral or bilateral. The patient should be questioned regarding any recent trauma to the breast. The medical history and medications are reviewed. Medications such as oral contraceptives, metoclopramide, phenothiazines, and selective serotonin reuptake inhibitors can be associated with nipple discharge. A premenopausal woman presenting with milky fluid discharge bilaterally or galactorrhea should be evaluated for endocrine disease. Hypogonadism as suggested by amenorrhea or hot flashes/vaginal dryness should prompt a workup for hyperprolactinemia. In addition, hypothyroidism, pituitary adenoma, and chest trauma (including thoracotomy) can result in galactorrhea. When endocrine disease is suspected, patients should undergo laboratory evaluation including quantitative hCG, prolactin level, and thyroid function tests. The physical examination should include a visual field test as often these patients may show signs of bitemporal field loss or chiasmal syndrome. A careful breast examination is performed to evaluate for any dominant masses, skin changes such as eczema/infections, nipple changes such as Paget disease, or adenopathy. Each of the quadrants of the involved breast is massaged from the periphery to the nipple areolar complex and then pressure is applied to the base of the nipple areolar complex to elicit discharge. This will help define the involved quadrant of the breast and whether the discharge is from a single ductal orifice. The color of any nipple discharge should be noted, and an occult blood test should be performed.
After initial evaluation, no further workup is required in women who have physiologic discharge, and these women should be advised to avoid manual compression of the nipples.
Imaging evaluation is indicated for patients with pathologic nipple discharge and includes an ultrasound, and for patients older than 30 years, a mammogram is also recommended. In patients with an imaging abnormality, a biopsy should be considered. Additional diagnostic tests that may be helpful include ductography and ductoscopy. Ductography is performed by instilling contrast medium into the involved duct to identify any lesions in the ductal system. Lesions will appear as a complete ductal obstruction, irregularities in the duct wall, or as an intraductal filling defect (Fig. 74-13). However, the absence of a lesion on ductography does not rule out a cancer.61 Ductoscopy is often performed in the operating room and involves the use of a small fiberoptic ductoscope that is placed into the involved duct. The benefit of ductoscopy is that it allows for direct visualization of any potential lesions, which may result in more precise excision.
The most common etiology of pathologic nipple discharge is a papilloma, which is a benign epithelial lesion with supporting stroma that grows within a duct. When a papilloma is diagnosed by core biopsy, the standard recommendation is to proceed with surgical excision as it may be associated with atypia or ductal carcinoma in situ (DCIS). Other causes for pathologic nipple discharge include malignancy (most commonly DCIS, 5% to 15% of cases) and duct ectasia, which is characterized by ductal dilatation with loss of elastin in the duct walls and the presence of chronic inflammatory cells. It is not known, however, whether the inflammatory cells result from a primary or secondary infection and antibiotics are not recommended.
If a malignancy is identified as the etiology of a pathologic nipple discharge, it should be managed accordingly with the appropriate cancer surgery typically as the first treatment. In the absence of a known malignancy, pathologic nipple discharge should be treated with terminal duct excision. Prior to excision, the patient should refrain from any nipple stimulation. If the involved duct can be identified intraoperatively, a lacrimal duct or instillation of methylene blue may aid with the duct excision. Terminal duct excision is commonly performed with a circumareolar incision and involves removal of the duct from its proximal to distal extent, which is often a distance of 2 to 3 cm. Alternatively, ductoscopy can be performed as previously prescribed and then the outer sheath of the cannula can be left in place as a guide for surgical excision of the involved duct. If there is difficulty isolating the involved duct or multiple ducts are involved, central or total terminal duct excision may be indicated. The potential risks of terminal duct excision include inability to breast-feed and hyposensitivity or hypersensitivity of the nipple.
Breast Infections
Breast infections are uncommon outside of the postpartum period. As such, breast infections can be classified as lactating or nonlactating infections. Lactating breast infections occur commonly during the initial 6 weeks of breast-feeding and during the process of weaning. In the initial stages of infection, a mastitis or cellulitis is typically found, with associated pain, erythema, induration, and fever. A woman should not be counseled to discontinue breast-feeding. Commonly, the cellulitis results from Staphylococcus aureus. Treatment includes pain management (acetaminophen, NSAIDs) and an antibiotic such as dicloxacillin. Alternative antibiotics include cephalexin and erythromycin. The mastitis should improve within 24 to 48 hours after initiation of antibiotics. If symptoms or fever persists, an abscess should be ruled out. For small or superficial abscesses, needle aspiration may be attempted. However, incision and drainage should be considered for large or complex abscesses, understanding the risks associated with milk fistula formation.
Nonlactating breast infections can present as periareolar abscesses or less commonly as peripheral abscesses. For small abscesses (less than 3 cm), needle aspiration and/or drain placement can be performed. However, for larger and/or deeper abscesses, incision and drainage may be indicated. This is commonly performed in the operating room under general anesthesia, although if the abscess is superficial or small, it may be possible to perform the incision and drainage at the bedside with infiltration of a local anesthetic. A preoperative ultrasound can be obtained to better evaluate the size and location of the abscess. The patient is placed in supine position and the surgical site is prepped and draped in the usual sterile fashion. Palpation of the abscess is performed, then using a no. 11 blade scalpel, a skin incision is made directly over the abscess. Often, the abscess is not located directly under the area of greatest erythema, and careful breast examination should be performed to localize the area of greatest fluctuance. Using a Kelly or Burlisher clamp, loculations are broken up in the cavity to fully drain the abscess. Biopsy of the cavity should always be considered, as breast infection may be an unusual breast cancer presentation. The abscess cavity is then copiously irrigated. For a subareolar abscess, removal of the sinus tract as well as the segmental duct should be considered. If the abscess is small, no packing is necessary. However for larger abscesses, we advocate loosely packing the wound with wet to dry gauze, which should be changed daily. Alternatively, an advanced wound care dressing can be used. The amount of the packing should be decreased daily and usually after 1 week, no further packing is needed. Alternatively, the incision can be loosely approximated with interrupted 4-0 nylon sutures leaving a 1.5-cm opening for a Penrose drain to be placed. The drain and the sutures should be removed within 4 to 7 days. Antibiotic, such as cephalexin 500 mg QID, is commonly prescribed for 7 to 10 days postoperatively, although once a wound is properly drained and cellulitis subsides, the patient can discontinue all antibiotics. For chronic subareolar abscesses, it may be necessary to completely excise the involved duct. During an acute exacerbation, patients are first treated with antibiotics and during the resolution phase, surgical excision is performed. Intraoperatively, the infected duct or fistula is identified using a lacrimal duct probe. A radial elliptical incision is then made incorporating the entire duct from the nipple to the subareolar breast tissue. Excision is then performed with care to fully dissect the subareolar duct system from the underlying breast tissue. Interrupted suture of 4-0 plain gut is then used to reapproximate the nipple from its apex to its base. The deep dermal layer of the skin is then reapproximated with 3-0 Vicryl sutures and the skin closed in a subcuticular fashion with 4-0 monocryl. The patient should be continued on antibiotics for an additional 2 weeks.
In the setting of recurrent or persistent abscess formation or inflammatory changes despite adequate surgical management, other etiologies need to be considered including idiopathic granulomatous mastitis, Wegener’s granuloma, sarcoidosis, tuberculosis, and histoplasmosis.
BENIGN BREAST DISEASE
Benign breast lesions can be classified into three groups: (1) nonproliferative breast lesions, (2) proliferative breast lesions without atypia, and (3) proliferative breast lesions with atypia (Table 74-4).
Nonproliferative Breast Lesions
Nonproliferative breast lesions include breast cysts, papillary apocrine change, epithelial-related calcifications, and mild hyperplasia of the usual type. These lesions are not associated with an increased risk of breast cancer.62 Papillary apocrine change is characterized by proliferation of ductal epithelial cells that show apocrine features and have eosinophilic cytoplasm. Benign calcifications found in normal ducts, lobules, breast stroma, and blood vessel walls are referred to as epithelial- related calcifications. Mild hyperplasia of the usual type occurs when the number of epithelial cells within a duct is more than two but not more than four cells in depth, and the epithelial cells do not cross the lumen of the involved space.63
CLASSIFICATION
Table 74-4 Classification of Benign Breast Disease

The most common nonproliferative lesions of the breast are cysts, which often present clinically as solitary masses that can be associated with pain. They are fluid-filled round or ovoid structures arising from the terminal duct lobular unit when fluid accumulates because of distension and obstruction of the efferent ductule.64 Given that cysts arise from lobular pathology, they occur mainly during lobular development, menstrual cyclic changes, and lobular involution in premenopausal and postmenopausal women, with peak incidence between 35 and 50 years of age.65,66
The three types of cysts are simple, complicated, and complex. Simple cysts are well circumscribed and on ultrasound have posterior acoustic enhancement. In addition, they are anechoic and do not have solid components or Doppler signals. If simple cysts are diagnosed by ultrasound, they are by definition benign and do not require further intervention, although cyst aspiration can be performed if the patient is symptomatic. Alternatively, FNA can also be used to diagnose simple cysts. If the aspirated fluid is nonbloody and the palpable mass completely resolves, this is also diagnostic of a simple cyst and no further diagnostic evaluation is required. A follow-up CBE with or without ultrasound can be performed in 3 to 6 months to document stability, and the patient may resume routine breast cancer screening.
Unlike simple cysts that are not associated with malignancy, complicated and complex breast cysts are associated with malignancy in <1% and 1% to 23%, respectively.67–69 On ultrasound, complicated cysts appear as masses with homogenous low-level internal echoes due to echogenic debris. However, there are no solid components, thick walls, or thick septa. Complex cysts are defined as cysts with solid components, thick walls, or thick septa. Complex cysts are characterized on ultrasound by the absence of posterior wall enhancement and the appearance of anechoic and echogenic components. Complicated cysts can be confirmed as benign by biopsy through FNA, core biopsy, or excisional biopsy. Alternatively, ultrasound imaging and mammography (if the lesion was visualized on mammography) with CBE every 6 months for 2 years can be performed to document stability. If complicated cysts develop any concerning changes such as an increase in size or development of a solid component, biopsy should be performed.70 Complex cysts mandate biopsy. If no fluid is aspirated by FNA, then core biopsy under image guidance should be performed with care to biopsy the solid component. A metallic clip marking the biopsy site facilitates surgical excision if necessary and facilitates follow-up imaging. If pathology is concordant with imaging findings, then follow-up with CBE and ultrasound imaging every 6 to 12 months for 1 to 2 years can be performed to document stability. For any concerning changes in the appearance of the lesion or increase in size, excisional biopsy should be performed. In patients who may be noncompliant with follow-up care, surgical excision should be considered for complicated and complex breast cysts.70
Proliferative Breast Lesions without Atypia
Proliferative breast lesions without atypia include ductal hyperplasia, intraductal papillomas, sclerosing adenosis, radial scars, and fibroadenomas. Ductal hyperplasia is often an incidental finding noted on biopsies obtained for mammographic abnormalities or for breast masses. Ductal hyperplasia is characterized by an increased number of cells within the ductal space; however, the cells retain the cytologic features of benign cells. Ductal hyperplasia is not associated with a significant risk for subsequent breast cancer and no additional treatment is necessary.63,71 Women with intraductal papillomas often present with pathologic nipple discharge (see section on Nipple Discharge above). These lesions consist of a monotonous array of papillary cells that grow from the wall of a duct or cyst into its lumen. Given that intraductal papillomas can harbor areas of atypia or DCIS, surgical excision is recommended when intraductal papillomas are diagnosed by core needle biopsy. If no atypia or DCIS is found at the time of excision, then no further treatment is necessary.72–76 Sclerosing adenosis typically presents as a mammographic abnormality or a mass and requires no further treatment following biopsy, as it is a benign lobular lesion resulting from increased fibrous tissue and interspersed glandular cells.77,78 Complex sclerosing lesions or radial scars are often found incidentally when a breast mass or radiologic abnormality is biopsied or excised. These lesions are characterized by a fibroelastic core with radiating ducts and lobules, and radial scars can appear spiculated on mammography.79 When diagnosed on core biopsy, radial scars should be excised as 8% to 17% are associated with malignancy at surgical excision.80–82 If the surgical excisional biopsy confirms a radial scar, no additional treatment is needed.
Fibroadenomas typically present as well-circumscribed mobile masses that are not fixed to the surrounding breast tissue. They are benign solid tumors made of glandular as well as fibrous tissue and are found most commonly in women between the ages of 15 and 35 years.83 Fibroadenomas with benign imaging characteristics can be followed with serial CBE and ultrasound imaging to ensure stability. Alternatively, core needle biopsy can be performed to confirm the diagnosis. If a fibroadenoma is asymptomatic, surgical excision is not necessary. However, if the presumed fibroadenoma is symptomatic or increases in size, excision can be performed for symptomatic relief or to rule out a malignancy such as a phyllodes tumor.84 Fibroadenomas that are associated with proliferative changes such as sclerosing adenosis, ductal epithelial hyperplasia, epithelial calcification, or papillary apocrine changes are referred to as complex fibroadenomas. Surgical excision of these lesions is often recommended to exclude a diagnosis of breast cancer,85,86 although this is controversial as some advocate that these lesions can be followed similarly as simple fibroadenomas.87
A fibroadenoma that is greater than 10 cm in size is referred to as a giant fibroadenoma and excision is recommended, as these lesions are hard to differentiate from a phyllodes tumor.63 Juvenile fibroadenomas occur in young women between the ages of 10 and 18 years and can vary in size from 5 to 20 cm in diameter. Surgical excision is recommended as these lesions can be cosmetically distressing for the young patient and are difficult to differentiate from a phyllodes tumor, although risk to the prepubertal breast bud is a potential complication.88
Proliferative Breast Lesions with Atypia
Proliferative breast lesions with atypia include ADH, ALH, flat epithelial atypia (FEA), and LCIS. Although these lesions are not considered premalignant, they are associated with an increase in the patient’s future risk of developing breast cancer (Fig. 74-14).
ADH is characterized by a proliferation of uniform epithelial cells with monomorphic round nuclei filling part, but not all, of the involved duct. ADH often presents as suspicious microcalcifications seen on mammography. In contrast, ALH is often an incidental finding found on breast biopsies performed for other reasons, such as an abnormal mammogram or breast mass. ALH is characterized by a proliferation of monomorphic, evenly spaced, dyshesive cells filling part, but not all, of the involved lobule.63 Atypical hyperplasias are associated with an increased risk of subsequent breast cancer (relative risk [RR] 3.7 to 5.3) in both the ipsilateral breast and the contralateral breast.89–93 In the past atypical hyperplasias (both ductal and lobular) that are diagnosed on core needle biopsy mandated a surgical excisional biopsy to exclude a diagnosis of malignancy. In case of atypical ductal hyperplasia, a surgical excisional biopsy is still recommended as an upgrade to DCIS or invasive breast cancer can occur in 10% to 20% of cases. However, in regards to lobular neoplasias (atypical lobular hyperplasia and LCIS), more recent evidence suggests that an association with malignancy may be as low as 1% (central pathology review) and 3% (local pathology review) and as such surgical excision for these lesions are no longer indicated.94 If the diagnosis of atypical hyperplasia is made by excisional biopsy and the area is adequately sampled, reexcision is not necessary or recommended. Instead, the patient should be counseled toward risk reduction strategies that include CBE every 6 to 12 months, annual screening mammography, and consideration for chemoprevention with a selective estrogen receptor modulator (SERM) or an aromatase inhibitor (AI).70 In addition, the patient should be counseled to perform consistent breast self-examinations (BSEs) such that she will become familiar with her breasts and report changes promptly to her provider (see the section on Management of Patients at High Risk for Breast Cancer later).

Figure 74-14. Cumulative risk for the development of invasive breast cancer after a biopsy for benign breast disease. Women with atypical hyperplasia (ductal or lobular type) are at a significantly increased risk for the development of breast cancer. (Reproduced with permission from Page DL, Dupont WD. Anatomic markers of human premalignancy and risk of breast cancer. Cancer 1990;66:1326.)
Lobular Carcinoma In Situ
LCIS is a noninvasive lesion that arises from the lobules and terminal ducts of the breast. It is characterized by solid proliferation of small cells, with small, uniform, round to oval nuclei, and variably distinct cell borders. The cytoplasms of the cells are clear to lightly eosinophilic and occasionally there are intracytoplasmic vacuoles that may be large enough to produce signet ring cell forms. LCIS tends to have a very low proliferative index and is estrogen-receptor positive.95 LCIS is more prevalent in premenopausal women and white women.96,97
3 LCIS is often diagnosed as an incidental finding on a breast biopsy that has been performed for another reason, such as an area of fibrocystic change or mammographic abnormality. Traditionally, if LCIS is identified on core biopsy, surgical excision is performed to exclude an associated cancer.97–101 However, more recent data suggests that this potential upgrade to DCIS or invasive cancer is likely 1% to 3% and as such surgical excision is no longer indicated.94,98–102 If LCIS is found on excisional biopsy, no further surgical intervention is needed. However, if pleomorphic LCIS is identified at a surgical margin on excisional biopsy, wide excision with negative margins is recommended as pleomorphic LCIS can be hard to differentiate from DCIS.103–105
RESULTS
Table 74-5 Risk for Breast Cancer Development After Lobular Carcinoma in Situ

Although it is not a premalignant lesion, LCIS conveys a substantial increased risk for breast cancer. The RR of developing an invasive cancer in women with LCIS is approximately two- to threefold higher than that in women without LCIS (Table 74-5).112 LCIS also conveys an increased risk for breast cancer to the contralateral breast. Historically, women diagnosed with LCIS were treated with bilateral prophylactic mastectomies. Most experts today consider this approach to be too aggressive given that most women with LCIS who do not have other contributory factors (e.g., family history of premenopausal breast cancer) will not develop an invasive breast cancer. Instead, a careful lifetime surveillance protocol similar to that described above for atypical hyperplasias can be followed. Chemoprevention with a SERM and/or AI can also be discussed with the patient. There are currently no randomized trials to compare the efficacy of surveillance protocol versus prophylactic mastectomy in women with LCIS.
FEA is an intraductal finding that is characterized by the replacement of native epithelial cells by a single layer, or up to 3 to 5 layers of mildly atypical cells (World Health Organization definition).113 When diagnosed on core biopsy, the risk of upgrade to a malignancy at surgical excision is 5% to 15%.114–116 When FEA is diagnosed by excisional biopsy, no further surgery is warranted. However, if FEA is diagnosed by core needle biopsy, excisional biopsy should be performed. Alternatively, radiologic surveillance can be performed and if there is absence of a residual mammographic abnormality and core biopsy was felt to be adequate, no further surgery is needed. Excisional biopsy must be performed for any residual lesions seen. When FEA is found at the margins, wider excision is not needed.114–117 Although FEA is an atypia, it conveys the same risk of breast cancer that is associated with benign proliferative disease without atypia and as such, patients should continue routine surveillance.118 There are also no data to support the use of chemoprevention.
BREAST CANCER SCREENING
Breast Self-Examination
BSE has not been shown to have an impact on the rates of breast cancer diagnosis, stage at diagnosis, or breast cancer mortality. In addition, BSE may result in higher rates of breast biopsy for benign disease. The largest study conducted was the Shanghai randomized trial involving 266,064 women who were assigned to either a BSE instruction group or a control group. The BSE group received instruction on BSE with reinforcement sessions 1 and 3 years later, supervised self- examination every 6 months for 5 years, and ongoing reminders. Intensive instruction on BSE did not reduce mortality from breast cancer but increased the rate of biopsy for benign disease.119 A review of eight other studies had similar findings.120 The US Preventive Services Task Force (USPSTF), the Canadian Task Force on Preventive Health Care (CTFPHC), the National Comprehensive Cancer Network (NCCN), and the World Health Organization do not recommend that women receive instruction on BSE. The American Cancer Society recommends that women be educated about the benefits and limitations of BSE. The American College of Obstetricians and Gynecologists recommends breast self-awareness, which can include BSE. In women who are not at high risk for breast cancer, we do not advocate for or discourage the use of BSE; however, we do promote breast self-awareness. Proper examination technique should be reviewed for women who are already routinely performing BSE, for women at high risk for the development of breast cancer, and for breast cancer survivors.
Clinical Breast Examination
Women should undergo CBE as part of their annual physical examination. However, it is difficult to determine the effectiveness of CBE as a screening tool as it is often performed with mammography. It has been suggested that CBE may modestly improve early detection of breast cancer but at the risk of increased false-positives.121,122 The effectiveness of CBE has not been proven by well-designed large clinical trials.123 As such, the USPSTF, the Canadian Task Force on Preventive Health Care, and the World Health Organization do not support CBE. The American Cancer Society and the American College of Obstetricians and Gynecologists recommend CBE every 3 years. We feel that CBE is critical to the evaluation of breast disease, as such, providers of women’s health have to become experts in this technique.
Screening Mammography
Screening mammography is widely performed but is not without controversy. Although systematic reviews of randomized trials have found a significant reduction in breast cancer mortality with mammographic screening in women aged 40 to 69 years, most of these studies were conducted before 1990, and there is concern that the current reduction in mortality is less as these trials were performed in an era prior to the adoption of modern treatment paradigms (multidisciplinary care and the use of adjuvant systemic treatments). In 2012, a meta-analysis of 11 randomized trials determined that the RR of breast cancer mortality for women undergoing screening mammography was 0.80 (95% confidence interval [CI], 0.73 to 0.89) compared with controls. This correlates with a RR reduction of 20%.124 In 2014, the Canadian National Breast Screening Study concluded a 25-year follow-up analysis. The cumulative mortality from breast cancer was similar between women randomized to the mammography arm or to the control arm. For women aged 40 to 49 years, they were randomly assigned to mammography or usual care, and for women aged 50 to 59 years, they were randomly assigned to mammography plus CBE or to CBE alone. As such, the study concluded that annual mammography in women aged 40 to 59 years does not reduce mortality from breast cancer beyond that of physical examination or usual care in the era of modern adjuvant therapy. In addition, they reported that 22% (106/484) of screen-detected invasive breast cancers were overdiagnosed.125 The primary risk of screening mammography is false-positive test results, which can result in patient anxiety, overdiagnosis, increased medical costs, and unnecessary biopsies.
Algorithm 74-4. Management of the patient with an abnormal screening mammogram. When pathology is benign, concordance or discordance with imaging findings dictates whether surgical excisional biopsy is indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






