Fig. 11.1 Anatomy of the laryngeal muscles relevant for botulinum neurotoxin injections. (a) Sagittal view showing the laryngeal structure. The arrows denote the direction for injection into the thyroarytenoid muscle for adductor spasmodic dysphonia and into the interarytenoid muscle for the tremorous spasmodic dysphonia. (b) Superior view showing the laryngeal structure and these technical aspects looking from superior angle.

Fig. 11.2 Transcutaneous injection technique. The injection should be done using electromyography control.
For patients with excessive gag reflex, 0.2 ml 1% lidocaine can be injected either through the cricothyroid membrane or underneath into the airway. The resulting cough would anesthetize the undersurface area of the vocal cord as well as the endotracheal structures, enabling the patients to tolerate the gag reflex (Truong et al., 1991).
Transoral technique
In the transoral approach, the vocal folds are indirectly visualized and the injections are performed using a device originally designed for collagen injection. Indirect laryngoscopy is used to direct the needle in an attempt to cover a broad area of motor endplates (Figs. 11.3 and 11.4) (Ford et al., 1990).

Fig. 11.3 The transoral appproach using a 90° video-endoscope.
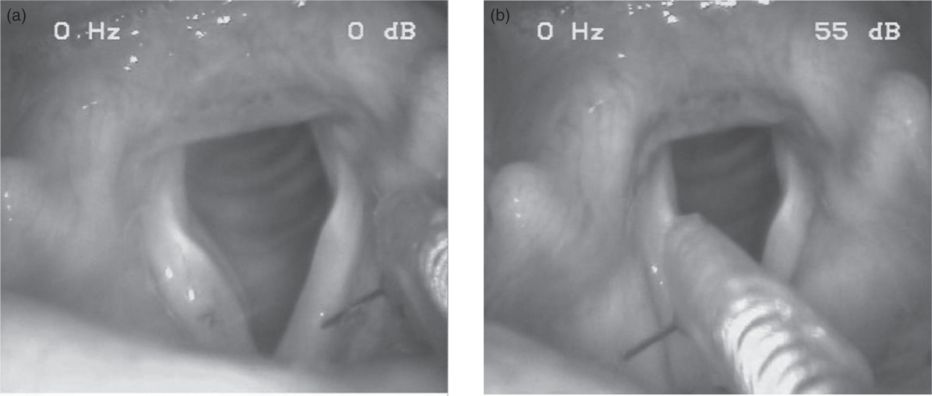
Fig. 11.4 Endoscopic view during transoral botulinum neurotoxin application (see Fig. 11.3). (a) Injection into the left vocal fold. (b) Injection into the right ventricular muscle (ventricular fold).
A large wastage of the BoNT because of the large dead volume of the long needle is a drawback of this technique.
In patients who cannot tolerate the gag reflex, a direct laryngoscopic injection can be performed under short total anesthesia (Fig. 11.5).
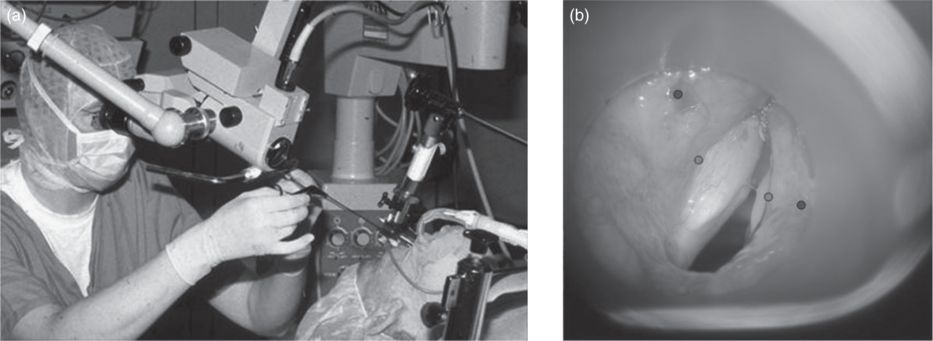
Fig. 11.5 Injection during microlaryngoscopy with a short general anesthetic. (a) The procedure, which normally does not use a tracheal tube and the injection is made during a short period of apnea. (b) Microscopical view of the larynx during microlaryngoscopy, the dots mark the typical injection points.
Transnasal technique
In the transnasal approach, BoNT is injected through a channel running parallel to the laryngoscope with a flexible catheter needle. This technique requires prior topical anesthesia with lidocaine spray (Rhew et al., 1994). The location of the injection is lateral to the true vocal fold in order to avoid damaging the vocal fold mucosa.
Point touch injections
In the point touch technique, the needle is inserted through the surface of the thyroid cartilage halfway between the thyroid notch and inferior edge of the thyroid cartilage. The BoNT is given once the needle is passed into the thyroarytenoid muscle (Green et al., 1992).
For injections into the ventricular folds, a transoral or transnasal approach is required (Fig. 11.4). Because EMG signals cannot be received from the ventricular muscle, a percutaneous technique is not recommended.
Botulinum neurotoxin doses
Doses of BoNT used for the treatment of spasmodic dysphonia vary depending on the particular brand of BoNT used. In general, although there are correlations between the doses, the appropriate dose for a given BoNT product is dictated by the possible side effects of the BoNT on the adjacent organs or muscles. The approximate dose relation between onabotulinumtoxinA, incobotulinumtoxinA, abobotulinumtoxinA and rimabotulinumtoxinB is 1: 1: 3: 50. This dose relationship should not be used as a guideline as the diffusion rates of these BoNTs differ and the close proximity of the muscle involved in swallowing should be the defining factor for the dose chosen.
In the early literature, the doses of BoNT (onabotulinumtoxinA) used for ADSD ranged from 3.75 to 7.5 U for bilateral injections (Brin et al., 1988a,b, 1989; Truong et al., 1991) to 15 U for unilateral injections (Miller et al., 1987; Ludlow et al., 1988). Later literature and common practice have recommended the use of lower doses (Blitzer and Sulica, 2001). We recommend starting with 0.5 U onabotulinumtoxinA/incobotulinumtoxinA, 1.5 U abobotulinumtoxinA or 200 U rimabotulinumtoxinB when injected bilaterally and to adjust the dose as needed. Our estimated average dose is 0.5 U onabotulinumtoxinA/incobotulinumtoxinA, 2–3 U abobotulinumtoxinA or 300 U rimabotulinumtoxinB.
Beneficial effects last about 3–4 months in our patients treated with onabotulinumtoxinA, incobotulinumtoxinA or abobotulinumtoxinA. They last about 8 weeks with rimabotulinumtoxinB (Adler et al., 2004a) but may be longer with higher doses (Guntinas-Lichius, 2003). In patients who received BoNT serotype B after type A failure, the duration was only about 2 months despite higher doses up to 1000 U per cord.
Botulinum neurotoxin treatment for abductor spasmodic dysphonia
Injection technique and muscles injected
With the thyroid lamina rotated forward, the needle is inserted behind the posterior edge and directed toward the posterior cricoarytenoid muscle. Location is verified by maximal muscle discharge when patients perform a sniff (Figs. 11.6 and 11.7) (Blitzer et al., 1992).
Fig. 11.6 Anterolateral view of the larynx and posterior cricoarytenoid muscle with the thyroid lamina rotated forward and to the other side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


