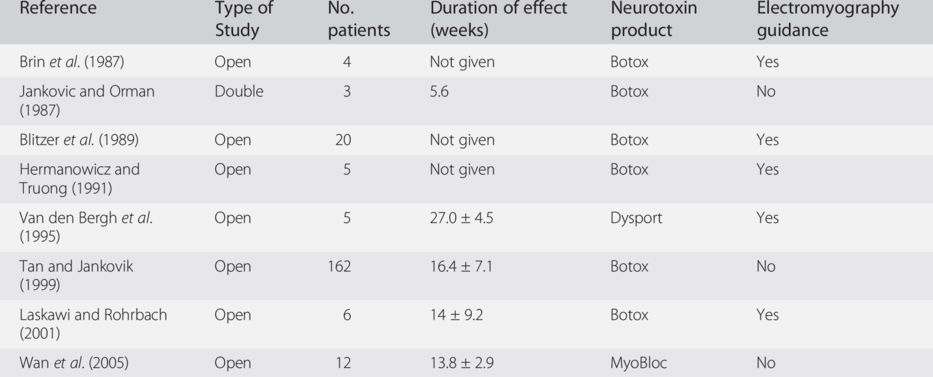
Botox, onabotulinumtoxinA; Dysport, abobotulinumtoxinA; MyoBloc, rimabotulinumtoxinB.
Dystonia is not a stereotyped disorder and its presentation in OMD is even more colorful. The treatment has to be individualized to accommodate the patient’s needs and symptoms. The various subtypes of OMD (jaw closing, jaw opening, jaw deviation, lingual, pharyngeal and mixed) need to be considered and the function of each muscle needs to be understood when assessing which muscles should be injected. Tables 9.2 and 9.3 (adapted from Bhidayasiri et al., 2006) list the muscle and their respective function.
| Muscle name | Functions |
|---|---|
| Temporalis | Close the jaw Posterior fibers retract the mandible Move jaw to the same side |
| Masseter | Close the jaw by elevating the mandible |
| Medial pterygoid | Close the jaw Protrude the jaw Moving the jaw to the opposite side |
| Lateral pterygoid | Open the mouth Protrude the jaw Move the jaw to the opposite side |
| Digastric | Open the jaw Elevate the hyoid bone |
| Mylohyoid | Open the jaw Raise the floor of the mouth |
| Geniohyoid | Open the jaw Elevate and draw hyoid bone forward |
| Subtype | Muscles involved |
|---|---|
| Jaw closing | Temporalis Masseter Medial pterygoid |
| Jaw opening | Lateral pterygoid Mylohyoid Digastric Geniohyoid |
| Jaw deviation | Contralateral lateral pterygoid Ipsilateral medial pterygoid Temporalis |
Injection techniques
Because of the lack of controlled trials and the significant heterogeneity of clinical presentation of OMD, the discussion that follows, which is subdivided according to main clinical types, is primarily based on the clinical experience of the authors.
Jaw-closing oromandibular dystonia
For jaw-closing OMD, often the masseter is the initial muscle selected for denervation (Bhidayasiri et al., 2006). If the response is not adequate, other muscles can be considered, including temporalis and pterygoid medialis. Injection is individualized for each patient and electromyography (EMG) guidance is only used to identify deep muscles that are not available to manual palpation since there is a suggestion that comparable results can be obtained without EMG (Bhidayasiri et al., 2006).
The masseter is a thick quadrilateral muscle with three parts – superficial, intermediate and deep – that arises from the zygomatic arch and inserts into the angle and the lateral surface of the ramus of the mandible (Clemente, 1984) (Fig. 9.1). It can be easily palpable by instructing the patient to clench the teeth. Very uncommonly, EMG guidance is required to reach it. In this case, it is approached using a teflon-coated needle connected to an EMG machine at 1 cm anterior to the posterior border of the ramus. The muscle discharge when the patient clenches the teeth also helps to confirm that the insertion is not in the parotid gland, which extends from the ear to the masseter and partially covers the posterior part of the muscle. A good starting dose is 50 U onabotulinumtoxinA/incobotulinumtoxinA or 100 U abobotulinumtoxinA. Experience with rimabotulinumtoxinB is not available from the literature except in two non-English journals (Cardoso, 2003; Wan et al., 2005). In our limited experience, we have used 2500 U rimabotulinumtoxinB for each masseter muscle.
Fig. 9.1 The masseter and temporalis muscles.
The medial pterygoid occupies the inner aspect of the ramus of the mandible opposite that of the masseter. It arises from the lateral pterygoid plate and the pyramical process of the palatine bone and inserts into the lower and back part of the medial surface of the ramus and angle of the mandible (Clemente, 1984) (Fig. 9.2). Because of its deep location, injection often requires EMG guidance. The medial pterygoid can be approached either intraorally or from below. When approached from below, the needle is inserted about 0.5–1 cm anterior to the angle of the mandible along the interior aspect of the mandible and angled perpendicularly to the mandible until it can be verified by the EMG with the patient clenching the teeth. Care should be taken to avoid the facial artery, which lies anteriorly. A good starting dose here is 20 U onabotulinumtoxinA/incobotulinumtoxinA, 30 U abobotulinumtoxinA Dyport (Bhidayasiri et al., 2006) or 1000 U rimabotulinumtoxinB.
Fig. 9.2 The pterygoid muscle.
The third muscle involved in jaw-closing OMD is the temporalis muscle (Fig. 9.1). This broad, radiating muscle arises from the temporal fossa. Its tendon inserts into the medial surface, apex and anterior border of the coronoid process and the anterior border of the ramus of the mandible (Clemente, 1984). The temporalis closes the jaws and its posterior fibers retract the mandible. The temporalis is approached perpendicular to its plane and possibly high in the temporal fossa as the lower part of the temporalis is mostly tendon, where the injection is painful. Because of its wide radiation pattern, three to four injections should be given. Recommended dose by the educational committee of WE MOVE is 40 U onabotulinumtoxinA (WE MOVE Spasticity Study Group, 2005). We, however, have opted for a higher dose, 50–100 U onabotulinumtoxinA/incobotulinumtoxinA. Early reports have used smaller doses (Bhidayasiri et al., 2006). Starting dose for abobotulinumtoxinA is about 100 U and adjusted according to patient’s response (Van den Bergh et al., 1995).
Jaw-opening oromandibular dystonia
The muscles involved in jaw opening include the lateral pterygoid, mylohyoid, digastric, geniohyoid and platysma (Clemente, 1984). Opening of the jaws is performed primarily by the pterygoid lateralis. In the beginning of the opening, it is assisted by the submentalis complex, which include the mylohyoid, digastric and geniohyoid (Clemente, 1984). The platysma may also play a minor role in the opening of the jaw. Most investigators reported injections of the lateral pterygoid in jaw-opening OMD, although others have claimed success with injection of the submentalis complex only (Bhidayasiri et al., 2006).
The lateral pterygoid is a short conical muscle arising from two heads: a superior from the great wing of the sphenoid bone and an inferior from the lateral surface of the lateral pterygoid plate of the sphenoid (Clemente, 1984) (Fig. 9.2). The lateral pterygoid can be approached intraorally or laterally through the mandibular notch. The entry point is about 35 mm from the external auditory canal and 10 mm from the inferior margin of the zygomatic arch. Using an EMG-guided technique, the needle is angled upward about 15 degrees to reach the inferior head of the lateral pterygoid. In close vicinity but more rostral is the pterygoid branch of the maxillary artery. The amount of BoNT reported in literature ranges from 20 to 40 U onabotulinumtoxinA (Blitzer et al., 1989; Laskawi and Rohrbach, 2001). The same amount of BoNT may be used for incobotulinumtoxinA. There is limited experience with abobotulinumtoxinA and we recommend a starting dose of about 60 U, titrating up if needed.
The digastric muscle is part of the submental complex. It arises from the mastoid notch of the temporal bone and attaches to the digastric fossa of the mandible (Fig. 9.3). It is divided into anterior and posterior bellies by the middle tendon, which is attached to the hyoid bone (Clemente, 1984). Besides elevating the hyoid bone, the digastric muscle pulls the chin backward and downward in opening the mouth, in conjunction with the lateral pterygoid. In contrast to the posterior belly, which is crowded with many nerves, the sympathetic trunk, arteries and veins, the anterior belly is open to intervention. The geniohyoid arises from the hyoid bone and inserts into the inferior genial tubercle of the mandible. It elevates the hyoid bone and base of the tongue. With the hyoid bone fixed, it depresses the mandible and opens the mouth. The mylohyoid also arises from the hyoid bone and attaches to the mylohyoid line of the mandible (Fig. 9.3). It raises the floor of the mouth during swallowing. The mylohyoid elevates the hyoid bone, thereby pushing the tongue upward (protrusion of the tongue; Clemente, 1984). It assists in opening the mouth. Muscles of the submental complex may be fused together, making it difficult to separate one from another (Clemente, 1984). This muscle group can be palpated with the patient opening his or her mouth. It is approached about 1 cm from mandible tip and injected slightly lateral from the midline (Fig. 9.3). A good starting dose of onabotulinumtoxinA/incobotulinumtoxinA is 30 U. These units are divided and injected into the two locations on each side. Higher doses up to 200 U for the submentalis complex have been reported (Tan and Jankovic, 1999) but the risk of severe dysphagia is considerable. For abobotulinumtoxinA, 90 U could be a good starting dose and for rimabotulinumtoxinB about 500 U.
Fig. 9.3 The digastric, geniohyoid and mylohyoid muscles. X, injection site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


