Chapter 20 Bones and Joints
1 What are the main anatomic portions of tubular long bones?
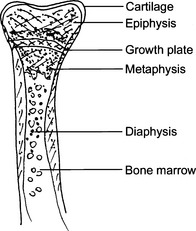
The midportion of a tubular long bone is called the diaphysis. The articular portion of these bones is called epiphysis. The part of the bone between the epiphysis and the diaphysis is called the metaphysis. In growing bones of children and adolescents, the midportion of the metaphysis contains the physis or the cartilaginous growth plate. The calcifying growth plates, easily recognizable on x-ray, are called secondary ossification centers, in contrast to primary ossification centers, a term used for the subperiosteal cortical bone formation. See Fig. 20-1.
2 Name the main bone-forming cells in the bone
 Osteocytes: These mature resting cells are involved in the maintenance of the basic functional and anatomic units of the bone, called osteons. Osteocytes also participate in the maintenance of the blood concentration of calcium and phosphates.
Osteocytes: These mature resting cells are involved in the maintenance of the basic functional and anatomic units of the bone, called osteons. Osteocytes also participate in the maintenance of the blood concentration of calcium and phosphates. Osteoblasts: These bone-forming cells synthesize osteoid and participate in its calcification. Osteoblasts can be stimulated by parathyroid hormone, vitamin D, and estrogens.
Osteoblasts: These bone-forming cells synthesize osteoid and participate in its calcification. Osteoblasts can be stimulated by parathyroid hormone, vitamin D, and estrogens. Osteoclasts: These bone-resorbing cells are closely related to macrophages. Thus they are derived from the same bone marrow precursors responding to granulocyte-macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor. In contrast to mononuclear macrophages, osteoclasts are multinucleated.
Osteoclasts: These bone-resorbing cells are closely related to macrophages. Thus they are derived from the same bone marrow precursors responding to granulocyte-macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor. In contrast to mononuclear macrophages, osteoclasts are multinucleated.4 What are the most important bone diseases?
DEVELOPMENTAL ABNORMALITIES
6 What is amelia?
A congenital abnormality characterized by an absence of upper or lower extremities or both.
13 List the causes of dwarfism
 Defects in bone formation, such as achondroplasia and osteogenesis imperfecta, and various mucopolysaccharidoses
Defects in bone formation, such as achondroplasia and osteogenesis imperfecta, and various mucopolysaccharidosesMETABOLIC DISORDERS
18 What are the risk factors for developing osteoporosis?
 Genetic factors: Osteoporosis runs in families and is considered to be a multifactorial disease. People who have thin bones and a small skeleton are more likely to develop osteoporosis than those who have a large frame (peak bone mass).
Genetic factors: Osteoporosis runs in families and is considered to be a multifactorial disease. People who have thin bones and a small skeleton are more likely to develop osteoporosis than those who have a large frame (peak bone mass). Hormones: Deficiency of estrogen in the postmenopausal period accelerates osteoporosis. Estrogen replacement therapy may retard the development of osteoporosis.
Hormones: Deficiency of estrogen in the postmenopausal period accelerates osteoporosis. Estrogen replacement therapy may retard the development of osteoporosis. Nutritional status: Calcium and vitamin D are essential for the maintenance of the skeleton, and a deficiency of these nutrients promotes osteoporosis.
Nutritional status: Calcium and vitamin D are essential for the maintenance of the skeleton, and a deficiency of these nutrients promotes osteoporosis.19 Is primary osteoporosis a single entity?
 Type 1 primary osteoporosis typically occurs in postmenopausal women. It is caused by increased activity of osteoclasts, related to decreased levels of estrogen in the circulation. Lack of estrogen is associated with an increased release of cytokines, such as interleukin (IL)-1 and IL-6, which stimulate osteoclasts.
Type 1 primary osteoporosis typically occurs in postmenopausal women. It is caused by increased activity of osteoclasts, related to decreased levels of estrogen in the circulation. Lack of estrogen is associated with an increased release of cytokines, such as interleukin (IL)-1 and IL-6, which stimulate osteoclasts.22 Does osteoporosis cause biochemical abnormalities that can be detected in the clinical laboratory?
25 What is the cause of osteomalacia?
 Abnormal vitamin D metabolism (e.g., deficiency of vitamin D receptors or deficiency of 1-hydroxylase, an enzyme that transforms the 25(OH)2 vitamin D in the kidneys into the active form 1,25(OH)2 of vitamin D)
Abnormal vitamin D metabolism (e.g., deficiency of vitamin D receptors or deficiency of 1-hydroxylase, an enzyme that transforms the 25(OH)2 vitamin D in the kidneys into the active form 1,25(OH)2 of vitamin D) Phosphate deficiency states encountered in some inborn errors of metabolism, such as renal Fanconi syndrome (renal wastage of phosphate, amino acids, and glucose)
Phosphate deficiency states encountered in some inborn errors of metabolism, such as renal Fanconi syndrome (renal wastage of phosphate, amino acids, and glucose)30 Are the bone lesions of hyperparathyroidism localized or diffuse?
 Osteitis fibrosa: Fibrous tissue replacing bone trabeculae in numerous bones or the entire skeleton.
Osteitis fibrosa: Fibrous tissue replacing bone trabeculae in numerous bones or the entire skeleton. Osteitis fibrosa cystica (von Recklinghausen disease): Cystic lesions caused by extensive resorption of cortical bone and subsequent cystic expansion of the bone defect.
Osteitis fibrosa cystica (von Recklinghausen disease): Cystic lesions caused by extensive resorption of cortical bone and subsequent cystic expansion of the bone defect.39 Describe how clinical laboratory data help in the diagnosis of metabolic bone diseases
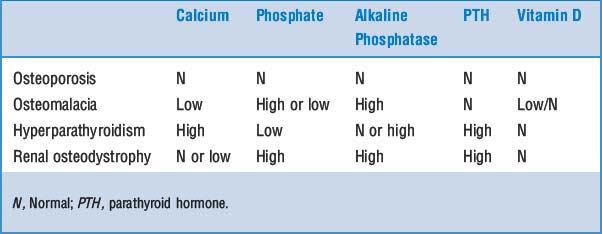
The clinical laboratory has an invaluable role in the study of bone diseases that present radiologically as osteopenia or osteopenia combined with osteosclerosis. The complete workup of the patient will typically require information on the serum calcium, phosphate, and alkaline phosphatase, which then can be supplemented with more expensive tests, such as measurement of PTH and vitamin D in blood. Typical findings are listed in Table 20-1.
FRACTURES
45 How do bone fractures heal?
The healing of bone fractures is a continuous process that can be divided into three stages:
 Provisional callus (procallus): It forms during the first week after fracture and is composed of granulation tissue, newly formed cartilage, and osteoid. It is typically fusiform, filling the defect caused by fracture, but also bulging over the edges of the fractured bone fragments.
Provisional callus (procallus): It forms during the first week after fracture and is composed of granulation tissue, newly formed cartilage, and osteoid. It is typically fusiform, filling the defect caused by fracture, but also bulging over the edges of the fractured bone fragments. Fibrocartilaginous callus: Formed during the second week from the procallus, it consists of more abundant collagenous matrix, cartilage, and osteoid that is in the process of calcification.
Fibrocartilaginous callus: Formed during the second week from the procallus, it consists of more abundant collagenous matrix, cartilage, and osteoid that is in the process of calcification.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree