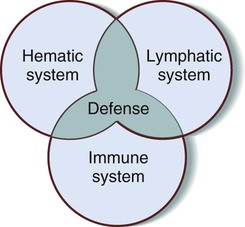
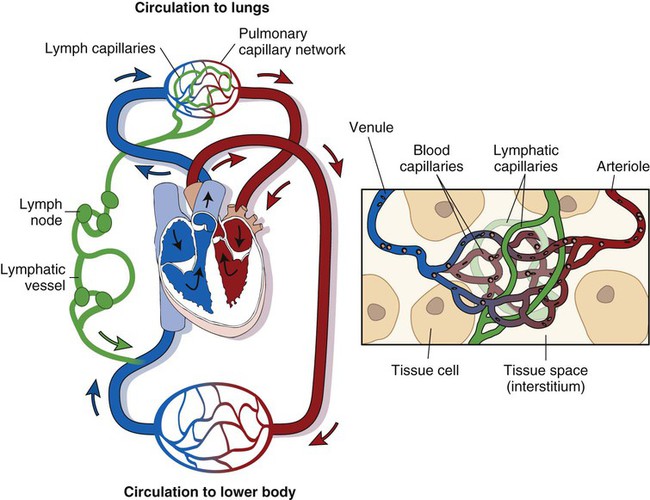
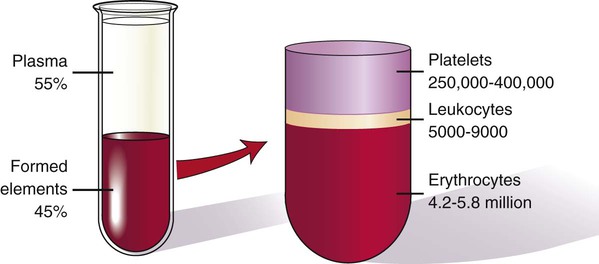
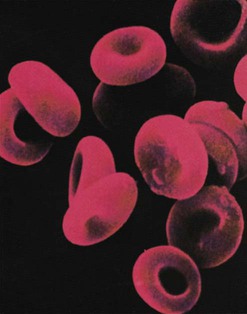
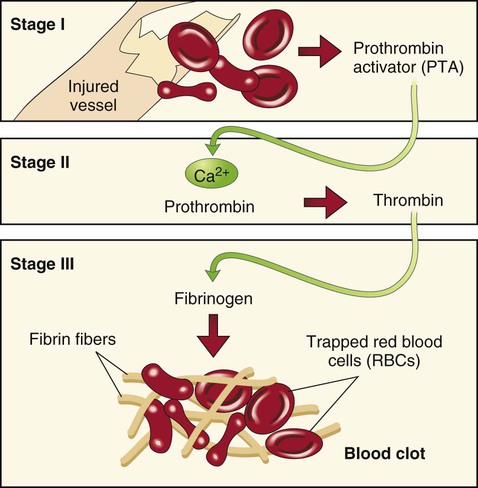
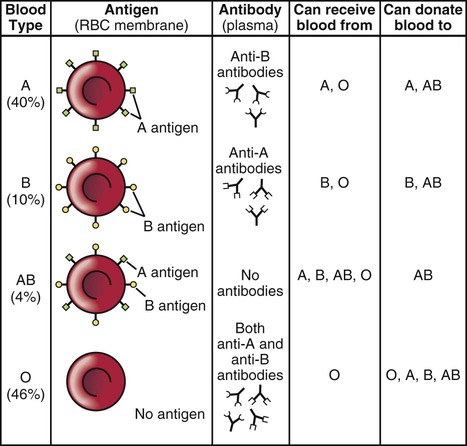
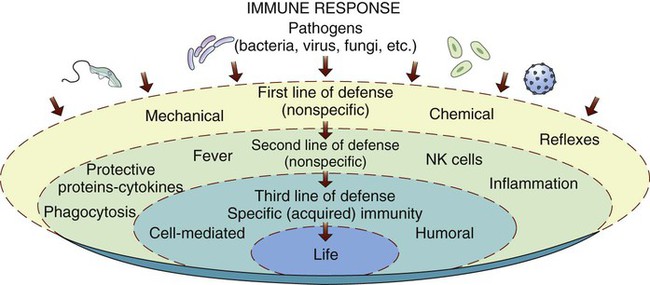
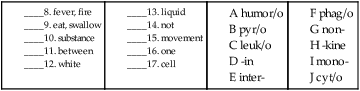
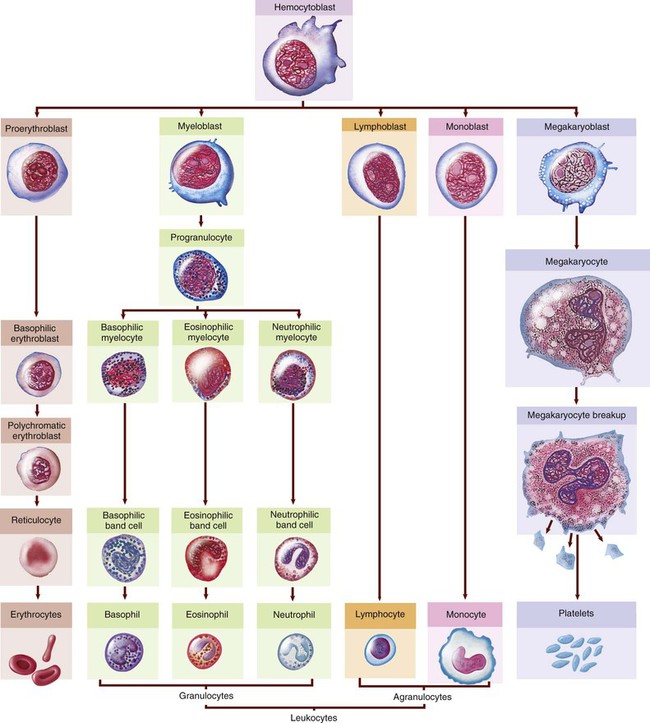
Excludes1 eosinophilia (D72.1) D72.820. Lymphocytosis (symptomatic) D72.821. Monocytosis (symptomatic) Excludes1 infectious mononucleosis (B27.-) Excludes1 confirmed infection—code to infection leukemia (C91.-, C92.-, C93.-, C94.-, C95.-) D72.828. Other elevated white blood cell count D72.829. Elevated white blood cell count, unspecified D72.89. Other specified disorders of white blood cells The blood is responsible for the following: • Transportation of gases (oxygen [O2] and carbon dioxide [CO2]), chemical substances (hormones, nutrients, salts), and cells that defend the body. • Regulation of the body’s fluid and electrolyte balance, acid-base balance, and body temperature. • Protection of the body from infection. • Protection of the body from loss of blood by the action of clotting. The lymph system is responsible for the following: • Cleansing the cellular environment. • Returning proteins and tissue fluids to the blood (drainage). • Providing a pathway for the absorption of fats and fat-soluble vitamins into the bloodstream. • Defending the body against disease. • The lymphatic system is discussed in Chapter 9 as part of the circulatory system. Explaining its role in protecting the body against disease, however, requires a discussion of how it interacts with the hematic and immune systems. The immune system is responsible for the following: Figure 8-1 is a Venn diagram of the interrelationship among the three systems, with the shared goals of homeostasis and protection at the intersection of the three circles. Figure 8-2 shows the relationship of the lymphatic vessels to the circulatory system. Note the close relationship between the distribution of the lymphatic vessels and the venous blood vessels. Tissue fluid is drained by the lymphatic capillaries and is transported by a series of larger lymphatic vessels toward the heart. The hematic system is composed of blood and the vessels that carry the blood throughout the body. The formation of blood, hematopoiesis, begins in the bone marrow with a single type of cell, a multipotential (pluripotent) hematopoietic stem cell (HSC), or hemocytoblast. This cell divides into cells that mature in lymphatic tissue (band T lymphocytes) and cells that mature in the bone marrow. Refer to Figure 8-3 to follow the development from the stem cell to specialized mature blood cells. Whole blood is composed of a solid portion that consists of formed elements, or cells, and a liquid portion called plasma. Blood cells make up 45% of the total blood volume, and plasma makes up the other 55% (Fig. 8-4). The solid portion of blood is composed of three different types of cells: 1. Erythrocytes, also called red blood cells (RBCs). 2. Leukocytes, also called white blood cells (WBCs). 3. Thrombocytes, also called clotting cells, cell fragments, or platelets. The erythrocytes (which are normally present in the millions) have the important function of transporting O2 and CO2 throughout the body (Fig. 8-5). The vehicle for this transportation is a protein-iron pigment called hemoglobin. When combined with oxygen, it is termed oxyhemoglobin. 1. Eosinophils (eosins) are cells that absorb an acidic dye, which causes them to appear reddish. An increase in eosinophils is a response to a need for their function in defending the body against allergens and parasites. 2. Neutrophils (neuts), the most numerous WBCs, are cells that do not absorb either an acidic or a basic dye and consequently are a purplish color. They are also called phagocytes because they specialize in phagocytosis and generally combat bacteria in pyogenic infections. This means that these cells are drawn to the site of a pathogenic “invasion,” where they consume the enemy and remove the debris resulting from the battle. Because the nucleus in immature neutrophils has a long “bandlike” shape, these cells are often referred to as band cells. They are also called stabs; the name is from the German word for rods because of their rodlike appearance. As the cells continue to mature, the bands divide, and the adult cells are renamed segs because now the nuclei are divided into clumps (segmented). 3. Basophils (basos) are cells that absorb a basic (or alkaline) dye and stain a bluish color. Especially effective in combating parasites, they release histamine (a substance that initiates an inflammatory response) and heparin (an anticoagulant), both of which are instrumental in healing damaged tissue. 1. Monocytes: These cells, named for their single, large nucleus, transform into macrophages, which eat pathogens (phagocytosis) and are effective against severe infections. 2. Lymphocytes (lymphs): These cells are key in what is called the immune response, which involves the “recognition” of dangerous, foreign (viral) substances and the manufacture of their neutralizers. The foreign substances are called antigens, and the neutralizers are called antibodies. Platelets (also known as thrombocytes or plats) have a round or oval shape and are so named because they look like small plates. Platelets aid in coagulation, the process of changing a liquid to a solid. When blood cells escape their normal vessels, they agglutinate, or clump together, by the following process: First, they release factor X (formerly called thrombokinase), which, in the presence of calcium, reacts with the blood protein prothrombin to form thrombin. Thrombin then converts another blood protein, fibrinogen, to fibrin, which eventually forms a meshlike fibrin clot (blood clot), achieving hemostasis (control of blood flow; that is, stopping the bleeding). See Figure 8-6 for a visual explanation of the clotting process. Plasma, the liquid portion of blood, is composed of the following: 2. Inorganic substances (calcium, potassium, sodium) 3. Organic substances (glucose, amino acids, fats, cholesterol, hormones) 4. Waste products (urea, uric acid, ammonia, creatinine) 5. Plasma proteins (serum albumin, serum globulin, and two clotting proteins: fibrinogen and prothrombin) Serum (pl. sera) is plasma minus the clotting proteins. Serology is the branch of laboratory medicine that studies blood serum for evidence of infection by evaluating antigen-antibody reactions in vitro. Human blood is divided into four major different types: A, B, AB, and O. See Figure 8-7 for a table of blood types, agglutinogens, and agglutinins. The differences are due to antigens present on the surface of the red blood cells. Antigens are substances that produce an immune reaction by their nature of being perceived as foreign to the body. In response, the body produces substances called antibodies that nullify or neutralize the antigens. In blood, these antigens are called agglutinogens because their presence can cause the blood to clump. The antibody is termed an agglutinin. For example, type A blood has A antigen, type B has B antigen, type AB has both A and B antigens, and type O has neither A nor B antigens. If an individual with type A blood is transfused with type B blood, the A antigens will form anti-B antibodies because they perceive B blood as being foreign. Following the logic of each of these antigen-antibody reactions, an individual with type AB blood is a universal recipient, and an individual with type O blood is a universal donor. Another antigen, the Rh factor, is important in pregnancy because a mismatch between the fetus and the mother can cause erythroblastosis fetalis, or hemolytic disease of the newborn (HDN) (see Fig. 7-10). In this disorder, a mother with a negative Rh factor will develop antibodies to an Rh+ fetus during the first pregnancy. If another pregnancy occurs with an Rh+ fetus, the antibodies will destroy the fetal blood cells. Figure 8-8 illustrates the levels of defense. The two outside circles represent nonspecific immunity and its two levels of defense. The inner circle represents the various mechanisms of specific immunity, which can be natural (genetic) or acquired in four different ways. Most pathogens can be contained by the first two lines of nonspecific defense. However, some pathogens deserve a “special” means of protection, which is discussed in the section titled “Specific Immunity.” • Mechanical: Examples include the skin, which acts as a barrier, and the sticky mucus on mucous membranes, which serves to trap pathogens. • Physical: Examples include coughing, sneezing, vomiting, and diarrhea. Although not pleasant, these serve to expel pathogens that have gotten past the initial barriers. • Chemical: Examples include tears, saliva, and perspiration. These have a slightly acidic nature that deters pathogens from entering the body while also washing them away. In addition, stomach acids and enzymes kill germs. Defensive processes include the following: • Phagocytosis: Phagocytosis is the process of cells “eating” and destroying microorganisms. Pathogens that make it past the first line of defense and enter into the bloodstream may be consumed by neutrophils and monocytes. • Inflammation: Acquiring its name from its properties, inflammation is a protective response to irritation or injury. The characteristics (heat, swelling, redness, and pain) arise in response to an immediate vasoconstriction, followed by an increase in vascular permeability. These provide a good environment for healing. If caused by a pathogen, the inflammation is called an infection. • Pyrexia: Pyrexia is the medical term for fever. When infection is present, fever may serve a protective function by increasing the action of phagocytes and decreasing the viability of certain pathogens. Active acquired immunity can take either of the following two forms: 1. Natural: Development of memory cells to protect the individual from a second exposure. 2. Artificial: Vaccination (immunization) that uses a greatly weakened form of the antigen, thus enabling the body to develop antibodies in response to this intentional exposure. Examples are the DTP and MMR vaccines. Passive acquired immunity can take either of the following two forms: 1. Natural: Passage of antibodies through the placenta or breast milk. 2. Artificial: Use of immunoglobulins harvested from a donor who developed resistance against specific antigens.
Blood, Blood-Forming Organs, and the Immune Mechanism
 Recognize and use terms related to the anatomy and physiology of the blood and immune systems. Recognize and use terms related to the pathology of the blood and immune systems.
Recognize and use terms related to the anatomy and physiology of the blood and immune systems. Recognize and use terms related to the pathology of the blood and immune systems.
 Recognize and use terms related to the procedures for the blood and immune systems.
Recognize and use terms related to the procedures for the blood and immune systems.
ICD-10-CM Examples from Tabular
D72.82 Elevated white blood cell count
Functions of the Blood and Immune Systems
Anatomy and Physiology
Hematic System
Components of Blood
Erythrocytes (Red Blood Cells)
Leukocytes (White Blood Cells)
Granulocytes (Polymorphonucleocytes)
Agranulocytes (Mononuclear Leukocytes)
Thrombocytes (Platelets)
Plasma
Blood Groups
Immune System
Nonspecific Immunity
Specific Immunity
Types of Acquired Immunity
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Blood, Blood-Forming Organs, and the Immune Mechanism