A number of factors are associated with bile duct injury during either open or laparoscopic cholecystectomy, including acute or chronic inflammation, inadequate exposure, patient obesity, and failure to identify structures before clamping, ligating, or dividing them. More specific causes of bile duct injury also exist. Bleeding from the cystic or hepatic arteries can lead to bile duct injury during attempts to gain hemostasis. The generous application of Ligaclips at either open or laparoscopic cholecystectomy to hilar areas not well visualized can result in placing a clip on or across a bile duct, with resultant injury (Fig. 62-1). Failure to recognize congenital anatomic anomalies of the bile ducts, such as insertion of the right hepatic duct into the cystic duct or a long common wall between the cystic duct and the common bile duct, can also lead to injury (Fig. 62-2). It should also be noted that a significant discussion has ensued regarding the optimal timing of performing a laparoscopic cholecystectomy in the setting of acute inflammation of the gallbladder. Although 30-day postoperative morbidity and mortality rates may remain independent of timing, it is clear that patients who undergo laparoscopic cholecystectomy beyond 24 hours are more likely to require an open procedure, and sustain significantly longer postoperative and overall lengths of hospital admission (and therefore cost).2
A number of technical factors are associated with laparoscopic cholecystectomy that can also increase the risk of bile duct injury compared with the open procedure. These factors include the use of an end-viewing laparoscope, which alters the surgeon’s perspective of the operative field. The issue of visual alignment and perspective has become even more topical with the proliferation of single incision laparoscopic cholecystectomy which is known to be associated with a higher rate of common bile duct injury than the traditional 4-incision laparoscopic technique utilizing an angled scope.3 Excessive cephalad retraction of the gallbladder fundus can cause the cystic duct and common bile duct to become aligned in the same plane. This distortion often results in the classic laparoscopic injury, in which the common bile duct is mistaken for the cystic duct and clipped and divided (Fig. 62-3).4 The role of intraoperative cholangiography (IOC) in preventing bile duct injury during laparoscopic cholecystectomy is controversial. Individual series have failed to demonstrate that either performing routine or selective IOC affects the incidence of bile duct injury. Although an initial retrospective nationwide cohort analysis of Medicare patients undergoing laparoscopic cholecystectomy between 1992 and 1999 demonstrated that common bile duct injuries occurred in 0.39% of patients in which IOC was performed versus 0.58% in patients not undergoing IOC (unadjusted relative risk, 1.49; 95% confidence interval 1.42–1.57),5 a more recent Medicare-based study (2000 to 2009) analyzing over 92,000 patients undergoing cholecystectomy identified no statistically significant association between IOC and common bile duct injury.6 The authors therefore concluded that IOC is not effective as a preventive strategy against common duct injury during cholecystectomy.6 Furthermore, the proper interpretation of IOC can minimize the extent of injury. Nevertheless, only 27% of surgeons in the United States perform IOC routinely.7 Finally, ample evidence exists to support the conclusion that the experience of the surgeon in performing laparoscopic cholecystectomy can be correlated with the risk of bile duct injury.
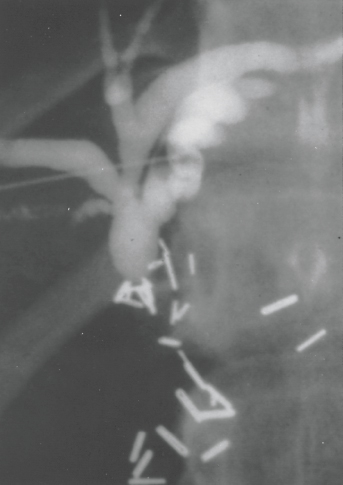
Figure 62-1. Percutaneous transhepatic cholangiogram in a patient with a bile duct stricture secondary to iatrogenic injury during cholecystectomy. Numerous surgical clips can be seen in the area of the stricture. (Reproduced with permission from Lillemoe KD, Pitt HA, Cameron JL. Postoperative bile duct strictures. Surg Clin North Am 1990;70:1356–1380.)

Figure 62-2. Operative cholangiogram demonstrating a right lobe segmental bile duct entering the cystic duct (arrow). Division of the cystic duct proximal to this insertion can result in a bile leak or obstruction of bile flow from a significant segment of the liver.

Figure 62-3. Classic laparoscopic bile duct injury. The common bile duct is mistaken for the cystic duct and transected. A variable extent of the extrahepatic biliary tree is resected with the gallbladder. The right hepatic artery, in background, is also often injured.
In recent years, there has been a growing understanding of surgeon cognitive factors associated with bile duct injury during laparoscopic cholecystectomy. An analysis examining 252 biliary injuries during laparoscopic cholecystectomy using human error factor and cognitive science techniques found that 97% of injuries were caused by visual-perceptual illusion or inadequate visualization.8 Further work from the same group has determined a major explanation for the surgeon’s frequent inability to recognize bile duct injury. These bile duct injuries appear to be associated with confirmation bias, which is a propensity to seek cues to confirm a belief and to discount cues that might discount the belief. Although cognitive factors are important for the understanding of the psychological issues associated with bile duct injuries, surgeons must continue to have the appropriate corrective mechanisms in place to minimize the chance of these injuries, including knowledge of anatomy, typical mechanisms of injury, and an appropriate level of suspicion and logic. An example of such a corrective mechanism occurs within the operative technique of laparoscopic cholecystectomy, which defines the “critical view of safety,” and therefore helps prevent misidentification and injury of the major bile ducts.9 This anatomical-based safety concept can be further developed by including the orientation and relative positions of the multiple structure of interest within adjacent regional anatomy (hepatic artery, sulcus of Rouvier, umbilical fissure, and common bile duct).
The importance of ischemia of the bile duct in the formation of postoperative strictures has been emphasized. Injury to the hepatic artery at the time of biliary injury during laparoscopic cholecystectomy has been recognized at an increased incidence, as high as 50%, when investigated at the time of presentation.10 The true impact of an arterial injury however, remains debated. It is clear that the most common site of vasculobiliary injury is the right hepatic artery.11 Damage to this vessel can lead to a higher injury level on the bile duct than the gross observed mechanical injury. Vasculobiliary injuries may also have specific effects on the arteries (pseudoaneurysm with delayed hemorrhage), bile ducts (necrosis, stenosis, cholangitis) and/or liver (necrosis, atrophy) over variable lengths of time.11 Finally, concurrent hepatic artery and portal vein injuries can have catastrophic effects on the liver, including rapid necrosis. A more clinically common cause of ischemia can be unnecessary dissection around the bile duct during cholecystectomy or bile duct anastomosis, which can divide or injure the major arteries of the bile duct that run in the 3-o’clock and 9-o’clock positions.
Another important factor contributing to the formation of biliary strictures is the intense connective tissue response with fibrosis and scarring that can occur after bile duct injury. Experimental studies of bile duct ligation in a canine model have demonstrated immediate and sustained elevation of bile duct pressure and progressive increase in bile duct diameter. Histologic changes at 1 month after ligation have shown that the bile duct wall is thickened, with a reduction of mucosal folds and loss of surface microvilli, associated with a well-defined epithelial degeneration. Biochemical analysis of connective tissue response to ligation showed that collagen synthesis and prolene hydroxylase activity is increased within 2 weeks in the obstructed bile duct and is sustained throughout the period of observation. Finally, a marked local inflammatory response can develop in the adjacent tissue in association with bile leakage, which occurs with many bile duct injuries. This inflammation can be further intensified in the face of infection. This inflammation results in fibrosis and scarring in the periductal tissue, further contributing to stricture formation. These factors can be of major importance in bile duct injuries during laparoscopic cholecystectomy, which are frequently associated with bile leaks.
After cholecystectomy and common bile duct exploration, the two most common operations associated with bile duct injury are gastrectomy and hepatic resection. The most common situation resulting in bile duct injury during gastrectomy involves dissection of the pyloric region and the first portion of the duodenum in the face of inflammation from peptic ulcer disease. The injury occurs during mobilization of the duodenum either for creation of a Billroth I gastroduodenostomy or for closure of the duodenal stump. Biliary injury during liver resection is most likely to occur during dissection of the hepatic hilum.
In addition to iatrogenic bile duct injury occurring during cholecystectomy or other operations, bile duct strictures can also occur at biliary anastomoses. Such strictures can occur at a biliary-enteric anastomosis performed for reconstruction after resection for benign or malignant disease of the pancreaticobiliary system, or after end-to-end bile duct anastomosis performed for hepatic transplantation (even in the context of chronic immunosuppressive therapy) or for repair of traumatic injury. Ischemia of the anastomosis caused by excessive skeletonization of the duct in preparation for the anastomosis is an important factor in many such strictures.

Algorithm 62-1. Algorithm for diagnosis and management of bile duct injury associated with laparoscopic cholecystectomy.
Unfortunately, the recurrence of bile duct strictures after an initial attempt at repair is not uncommon and can also account for a number of anastomotic strictures.12,13 A number of other factors have been evaluated in patients who have a recurrent bile duct stricture, including the location of the stricture, the length of follow-up, the influence of previous operations, the type of operation performed, the type of sutures used, and the use and duration of postoperative stenting.14 Previous attempts at repair, performance of a procedure other than choledochojejunostomy or hepaticojejunostomy, and stricture location higher in the biliary tree appear to be associated with a higher incidence of recurrent stricture. Finally, long-term follow-up of a bile duct anastomosis is important because strictures can develop years after the original anastomosis.
Clinical Presentation
2 Most patients with biliary injuries present early after their initial operation (Algorithm 62-1). After open cholecystectomy, only approximately 10% of postoperative strictures are actually suspected within the first week, but nearly 70% are diagnosed within the first 6 months, and more than 80% are diagnosed within 1 year of surgery. In series reporting bile duct injuries during laparoscopic cholecystectomy, the injury is usually recognized either during the procedure (25% to 30%) or, more commonly, in the early postoperative period.
Patients suspected of having a postoperative bile duct injury within days to weeks of initial operation usually present in one of two ways. One presentation is the progressive elevation of liver function test results, particularly total bilirubin and alkaline phosphatase levels. These changes can often be seen as early as the second or third postoperative day. The second mode of early presentation is with leakage of bile from the injured bile duct. This presentation appears to occur most often in patients presenting with bile duct injuries after laparoscopic cholecystectomy. Bilious drainage from operatively placed drains or through the wound after cholecystectomy is abnormal and represents some form of biliary injury. In patients without drains (including patients in whom the drains have been removed), the bile can leak freely into the peritoneal cavity or it can loculate as a collection. Free accumulation of bile into the peritoneal cavity results in either biliary ascites or bile peritonitis. Similarly, a loculated bile collection can result in sterile biloma (Fig. 62-4) or in an infected subhepatic or subdiaphragmatic abscess.
Patients with postoperative bile duct strictures who present months to years after the initial operation frequently have evidence of cholangitis. The episodes of cholangitis are often mild and respond to antibiotic therapy. Repetitive episodes usually occur before the definitive diagnosis. Less commonly, patients may present with painless jaundice and no evidence of sepsis. Finally, patients with markedly delayed diagnoses may present with advanced biliary cirrhosis and its complications.

Figure 62-4. Large bile duct collection (biloma; arrow) occurring after bile duct injury. (Reproduced with permission from Lillemoe KD, Pitt HA, Cameron JL. Postoperative bile duct strictures. Surg Clin North Am 1990;70:1355–1380.)

Figure 62-5. A: Percutaneous transhepatic cholangiogram demonstrating bile duct stricture at hepatic duct bifurcation with proximal duct dilatation. B: Percutaneous transhepatic cholangiogram demonstrating stricture (arrow) at a hepaticojejunostomy anastomosis. BD, bile duct; int, intestine.
Laboratory Investigation
Liver function tests usually show evidence of cholestasis. In patients with bile leakage, the bilirubin can be normal or minimally elevated because of absorption from the peritoneal cavity. When elevated, serum bilirubin usually ranges from 2 to 6 mg/dL, unless secondary biliary cirrhosis has developed. Serum alkaline phosphatase is usually elevated. Serum aminotransferase levels can be normal or minimally elevated except during episodes of cholangitis. If advanced liver disease exists, hepatic synthetic function can be impaired, with lowered serum albumin and a prolongation of prothrombin time. Serum electrolytes and complete blood count are typically normal unless there is associated biliary sepsis.
Radiologic Examination
The imaging techniques of abdominal ultrasound and computed tomography (CT) play an important initial role in the evaluation of patients with benign postoperative biliary strictures. In patients who present in the early postoperative period with evidence of a bile leak or biliary sepsis, these studies are useful to rule out the presence of intra-abdominal collections that might require drainage (Fig. 62-4). CT and ultrasound are also important in the initial evaluation of the patient presenting with a bile duct stricture months to years after initial operation. Both studies can confirm biliary obstruction by demonstrating a dilated biliary tree. CT is especially useful in identifying the level of obstruction of the extrahepatic bile duct.
In patients suspected of having early postoperative bile duct injury, a radionucleotide biliary scan can confirm bile leakage. In patients with postoperative external bile fistula, injection of water-soluble contrast media through the drainage tract (sinography) can often define the site of leakage and the anatomy of the biliary tree.
3 The “gold standard” for evaluation of patients with bile duct strictures is cholangiography. Percutaneous transhepatic cholangiography (PTC) is usually more valuable than endoscopic retrograde cholangiography (ERC) in patients with major bile duct injuries following laparoscopic cholecystectomy. PTC is more useful in that as it defines the anatomy of the proximal biliary tree that is to be used in the surgical reconstruction (Fig. 62-5). Furthermore, PTC can be followed by placement of percutaneous transhepatic catheters, which can be useful in decompressing the biliary system both to treat or prevent cholangitis and to control an ongoing bile leak. These catheters can also be of assistance in surgical reconstruction and provide access to the biliary tree for nonoperative dilation. ERC is less useful than PTC in major bile duct transections during laparoscopic cholecystectomy because the discontinuity of the extrahepatic bile duct usually prevents adequate filling of the proximal biliary tree (Fig. 62-6). Often, ERC can demonstrate a normal-sized distal bile duct up to the site of the stricture without visualization of the proximal biliary system (Fig. 62-7). This finding is frequently the case in patients with injury during laparoscopic cholecystectomy, when the distal bile duct is often clipped and divided. The development of magnetic resonance cholangiopancreatography (MRCP) has provided a noninvasive technique that provides excellent delineation of the biliary anatomy. The quality of these images has led some surgeons to advocate this technique as the initial step in the evaluation of patients with suspected bile duct injuries and may eliminate the need for a diagnostic ERC in many patients. MRCP is especially worth considering if the referral surgeon has a low pretest probability of utilizing transhepatic stents for subsequent reconstructive purposes.

Figure 62-6. A: Endoscopic retrograde cholangiogram showing a relatively normal biliary tree in a patient with a postoperative bile collection (see Fig. 62-5). B: Percutaneous transhepatic cholangiogram of the same patient, showing entire right hepatic posterior lobe segment obstructed as the result of ligation of the segmental duct. The patient had an unrecognized anatomic variant similar to that shown in Figure 62-2.
Preoperative Management
4 The preoperative management of a patient with a postoperative bile duct stricture depends primarily on the timing of the presentation. Patients presenting in the early postoperative period can be septic with either cholangitis or intra-abdominal bile collections. Sepsis must be controlled first with broad-spectrum parenteral antibiotics, percutaneous biliary drainage, and percutaneous or operative drainage of biliary leaks. Once sepsis is controlled, there is no hurry in proceeding with surgical reconstruction of the bile duct stricture. The combination of proximal biliary decompression and external drainage allows most biliary fistulas to be controlled or even to close. The patient can then be discharged home to allow several weeks to elapse for resolution of the inflammation in the periportal region and recovery of overall health.

Figure 62-7. Endoscopic retrograde pancreaticocholangiogram showing filling of a normal pancreatic duct (PD). The common bile duct (CBD), however, does not fill beyond the large clip that appears to be placed across the duct. (Reproduced with permission from Lillemoe KD, Pitt HA, Cameron JL. Postoperative bile duct strictures. Surg Clin North Am 1990;70:1355–1380.)
The management of a suspected bile duct injury after laparoscopic cholecystectomy presenting with a bile leak deserves special mention. Often, when bile leakage is suspected, the surgeon believes that urgent surgical exploration is necessary. Unfortunately, at laparotomy, the marked inflammation associated with bile spillage and the small decompressed biliary tree that appears retracted high into the porta hepatis make recognition of the injury and repair virtually impossible. In such cases, every attempt should be made to define the biliary anatomy by preoperative cholangiography (PTC or MRCP) and to control the bile leak with percutaneous biliary drainage. In many cases, early operative intervention is not required because the bile collections or ascites can either be drained percutaneously or simply is absorbed from the peritoneal cavity. Delayed reconstruction, aided by percutaneous biliary catheters, then allows optimal surgical results.14
In patients who present with a biliary stricture remote from the initial operation, symptoms of cholangitis can necessitate urgent cholangiography and biliary decompression. Biliary drainage is best accomplished by the transhepatic method, although successful endoscopic stent placement can also be accomplished. Parenteral antibiotics and biliary drainage should be continued until sepsis is controlled. In patients who present with jaundice but without cholangitis, cholangiography should be performed to define the anatomy. Preoperative biliary decompression in patients without cholangitis has not been demonstrated to improve outcome.
Surgical Management
The goal of operative management of bile duct stricture is the establishment of bile flow into the proximal gastrointestinal tract in a manner that prevents cholangitis, sludge or stone formation, restricture, and biliary cirrhosis. This goal is best accomplished with a tension-free anastomosis between healthy tissues. A number of surgical alternatives exist for primary repair of bile duct strictures, including end-to-end repair, Roux-en-Y hepaticojejunostomy or choledochojejunostomy, choledochoduodenostomy, and mucosal grafting. The choice of repair depends on a number of factors, including the extent and location of the strictures, the experience of the surgeon, and the timing of the repair.
Immediate Repair of Intraoperative Bile Duct Injury
In many cases, initial proper management of bile duct injury recognized at the time of cholecystectomy can avoid the development of a bile duct stricture. Unfortunately, recognition of a bile duct injury is uncommon during either open or laparoscopic cholecystectomy. If bile leakage is observed or atypical anatomy is encountered during laparoscopic cholecystectomy, early conversion to an open technique and prompt cholangiography are imperative. If a segmental or accessory duct less than 3 mm has been injured and cholangiography demonstrates segmental or subsegmental drainage of the injured ductal system, simple ligation of the injured duct is adequate. If the injured duct is 4 mm or larger, however, it is likely to drain multiple hepatic segments or the entire right or left lobe and thus requires operative repair.
If the injury involves the common hepatic duct or the common bile duct, repair should also be carried out at the time of injury. The aims of any repair should be to maintain ductal length and not to sacrifice tissue, as well as to affect a repair that will not result in postoperative bile leakage. To accomplish these goals, all repairs at the time of initial operation should involve some sort of external drainage. If the injured segment of the bile duct is short (<1 cm) and the two ends can be opposed without tension, an end-to-end anastomosis can be performed with placement of a T-tube through a separate choledochotomy either above or below the anastomosis (Fig. 62-8A). Generous mobilization of the duodenum out of the retroperitoneum (Kocher maneuver) can be useful to help approximate the injured ends of the bile duct. An end-to-end repair, however, should be avoided if the ductal injury is near the hepatic duct bifurcation. It must also be remembered that in the nontransplantation setting, the patient does not have the benefit of a lower stricture rate due to chronic immunosuppression.

Figure 62-8. All biliary anastomoses performed for the reconstruction of acute bile duct injury should have external drainage. A: If the injured segment of bile duct is short (<1 cm) and the two ends can be opposed without tension, an end-to-end anastomosis can be performed with placement of a T-tube through a separate choledochotomy either above or below the anastomosis. The T-tube should not be brought out directly through the anastomosis. B: With more proximal injuries or if the segment of injured bile duct is greater than 1 cm, an end-to-end bile duct anastomosis should be avoided and a Roux-en-Y hepaticojejunostomy should be constructed. A transanastomotic stent can be placed retrograde through the transected duct and exited to the hepatic parenchyma to allow postoperative external drainage.
5 For proximal injuries or if the injured segment of the bile duct is greater than 1 cm in length, an end-to-end bile duct anastomosis should be avoided because of the excessive tension that usually exists in these situations. In these circumstances, the distal bile duct should be oversewn, and the proximal bile duct should be debrided of injured tissue and anastomosed in an end-to-side fashion to a Roux-en-Y jejunal limb. The use of a Roux-en-Y jejunal limb is preferable to anastomosis to the duodenum because, in the latter case, an anastomotic leak results in a duodenal fistula. A transanastomotic Silastic stent can be placed retrograde through the transected duct and exiting the hepatic parenchyma (Fig. 62-8B) to allow for postoperative external drainage.
Unfortunately, most bile duct injuries during laparoscopic cholecystectomy occur in the hands of surgeons who are not experienced in performing complex biliary reconstruction. In such settings, the surgeon should consider not repairing the injury and not risk further worsening the situation. The biliary tree should be drained via a retrograde catheter to facilitate cholangiography, but the bile duct should not be ligated. More specifically, ligation of the proximal bile duct most often leads to stump necrosis, subsequent bile leakage and a more challenging reconstruction due to proximal migration of the injury itself.15 The subhepatic space should be well drained to control the biliary leak. Prompt transfer to a tertiary hepatobiliary center should then be made.
The long-term results of immediate repair of common bile duct injuries are uncertain. Most injuries occur away from major centers, and therefore, even the successes are unlikely to be reported in the literature. In a Swedish report, early primary repair with end-to-end anastomosis resulted in good outcomes in only 22% of patients. Anastomotic leak requiring reoperation occurred in 32% of patients, and late stricture occurred in another 37% of patients. In patients undergoing immediate repair with a biliary-enteric anastomosis, good results were seen in 54% of patients, with strictures occurring in only 12% of patients. Similar poor late results were observed in another series in which 29 of 36 patients with primary end-to-end repair had postoperative strictures within 4 years.
Elective Repair of Bile Duct Injuries and Established Strictures
Several principles are associated with successful repair of a biliary injury or stricture: exposure of healthy proximal bile ducts that provide drainage of the entire liver; preparation of a suitable segment of intestine that can be brought to the area of the stricture without tension, most frequently a Roux-en-Y jejunal limb; and creation of a direct biliary-enteric mucosal-to-mucosal anastomosis. A number of alternatives for elective repair of bile duct strictures exist. The choice of procedure is dictated by the location of the stricture, the history of previous unsuccessful attempts at repair, and the surgeon’s personal preference. Simple excision of a bile duct stricture and end-to-end bile duct anastomosis or repair of the damaged duct can rarely be accomplished because of the invariable loss of duct length as a result of fibrosis associated with the injury. Similarly, anastomosis of the proximal bile duct to the duodenum as a choledochoduodenostomy is not suitable for most postcholecystectomy strictures because an adequate length of bile duct for creating a tension-free anastomosis to the duodenum usually cannot be obtained. Thus, in almost all cases, hepaticojejunostomy constructed to a Roux-en-Y limb of jejunum is the preferred procedure.
Many surgeons believe that a transanastomotic stent is helpful in almost all cases. In the early postoperative period, a stent is used to decompress the biliary tree and provide access for cholangiography. If the injury involves the common bile duct or the common hepatic duct at least 2 cm distal to the hepatic duct bifurcation, and adequate proximal bile duct mucosa can be defined, the use of long-term biliary stents is not necessary. In these situations, the preoperatively placed percutaneous transhepatic catheter or operatively placed T-tube is used to decompress the biliary-enteric anastomosis for 4 to 6 weeks after surgery. When adequate proximal bile duct is not available for a good mucosa-to-mucosa anastomosis, long-term stenting of the biliary-enteric anastomosis with a Silastic transhepatic stent is recommended. For strictures involving the hepatic duct bifurcation, both the right and left main hepatic ducts should be individually stented.
An operative technique for biliary reconstruction with transhepatic stents using the preoperatively placed percutaneous transhepatic catheters begins with dissection of the porta hepatis, which usually involves separating adhesions of the duodenum and hepatic flexure of the colon to the Glisson capsule and gallbladder fossa.16 Identification of the proximal biliary segment can be difficult and can be aided by the presence of the transhepatic biliary catheter. This is particularly true for bile duct transections that will retract high into the porta. If a primary duct stricture exists, the bile duct is then divided at the lowest extent of the stricture and dissected proximally. A segment of the strictured duct should be resected and submitted for pathologic examination. The distal duct is then oversewn, and the bile duct proximal to the stricture is carefully dissected circumferentially in a cephalad direction for a distance not to exceed 5 mm. Excessive dissection should be avoided to prevent vascular compromise of this segment of duct, which will be used for the anastomosis. After mobilization and division of the bile duct, the biliary catheters protrude through the proximal end (Fig. 62-9A). A radiologic guide wire is then placed through these catheters. The preoperatively placed catheter can then be exchanged over the wire for a properly sized Silastic stent. These stents are 70 cm long and range from 12 French to 22 French. Multiple side holes are present along 40% of the length of the stent. These side holes are left to reside within the intrahepatic biliary tree and the portion of the Roux-en-Y jejunal limb used for the biliary anastomosis. The end of the stent without the side holes exits through the hepatic parenchyma and is brought out through a stab wound in the upper anterior abdomen. After stent placement, a Roux-en-Y jejunal limb is prepared, and the anastomosis is then performed as an end-to-side hepaticojejunostomy (Fig. 62-9B–D).
The importance of the hilar (epicholedochal) arterial plexus in cases of proximal bile duct injuries is also worth mention. More specifically, performing a “high” hepaticojejunostomy reconstruction to an intact proximal hilar bridge between the right and left hepatic ducts utilizes robust crossing arterial anatomy and is believed by many surgeons to minimize the risk of subsequent biliary stenosis.
An alternative technique has been described for management of bile duct strictures involving the bifurcation and one or both of the hepatic ducts in which a side-to-side anastomosis of the left hepatic duct to the Roux-en-Y limb is constructed. A long opening along the anterior surface of the left hepatic duct is anastomosed to the side of the Roux-en-Y limb. Because it is possible to dissect the anterior surface of the left hepatic duct high up into the hepatic parenchyma, this procedure permits anastomosis to normal mucosa, even though there can be fibrosis and stricture at the bifurcation of the ducts and in the distal portion of the hepatic duct. This technique can avoid the need for postoperative stenting.
Surgical Outcome
Morbidity and Mortality
Repairs of bile duct strictures are performed primarily in major medical centers by experienced surgeons, yet these operations are still associated with significant morbidity and mortality. In 1982, a review of 38 series published since 1900 that included more than 7,643 procedures performed on 5,586 patients reported an overall operative mortality rate of 8.3%.17 More recently the incidence of operative mortality has decreased markedly with improved technology and a multidisciplinary approach, as well as improved surgical experience. A recent series of 200 consecutive patients managed at the Johns Hopkins Hospital reported three deaths in patients who did not undergo an attempt at repair who were referred with sepsis secondary to an uncontrolled biliary leak, for a mortality rate of 1.5%. Definitive surgical reconstruction was performed in 175 patients with a perioperative mortality of only 1.7%.18 In this series the timing of repair, the mode of presentation, previous attempts of repair, and the level of injury did not influence outcome. Chronic liver disease can be an important factor for operative mortality and morbidity with advanced biliary cirrhosis and portal hypertension leading to mortality rates approaching 30%. Fortunately in the modern era, such advanced disease is uncommon. In most series postoperative morbidity rates are in the range of 20% to 40%. In the recent Hopkins series, complications occurred in 41% of patients. Most of the complications were minor and could be managed with either interventional radiology techniques or conservative management. No patient required reoperation for postoperative complications. The median length of stay in this series was 8 days.

Figure 62-9. Technique of biliary reconstruction. A: A Silastic stent is sutured to the preoperatively placed transhepatic catheter, which protrudes through the transected hepatic duct and through the catheter tract in the hepatic parenchyma. B: A Roux-en-Y jejunal loop is then anastomosed to the hepatic duct and (C) the Silastic stent is placed through the anastomosis. D: A completed Roux-en-Y hepaticojejunostomy with a transanastomotic stent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


