• Affects more than 50% of men in their lifetime: incidence increases with advancing age: 5%-10% at age 30 years, more than 90% among those older than 85 years. • Genetic predisposition: hereditary benign prostatic hyperplasia (BPH; early-onset enlarged prostate) is autosomal dominant or codominant. More common late-onset BPH has weaker genetic aspect. Alleles of genes coding for cytochrome P450c17alpha enzyme, which mediates sex steroid synthesis, are implicated in BPH and prostate cancer. Hereditary BPH may be recalcitrant to natural means alone; late-onset type may be more responsive. Treatments described below modify sex steroid metabolism and decrease symptoms; they are recommended for both types of BPH. • Androgen-dependent disorder of metabolism: free testosterone decreases with age; prolactin, estradiol, sex hormone–binding ligand, luteinizing hormone, and follicle-stimulating hormone increase. Synthesis of potent androgen dihydrotestosterone (DHT) from testosterone by 5-alpha-reductase increases and hydroxylation metabolism of testosterone and DHT decreases from inhibition by elevated estrogens. • Ultimate effect: increased intraprostatic DHT. Prostatic androgen receptors have a fivefold greater affinity for DHT than testosterone. BPH tissue has three- to fourfold greater net ability to increase tissue levels of DHT. • BPH originates in periurethral and transition zones of prostate as early as the third decade of life. • Develops from microscopic to palpable enlargement with age and androgen influence. • Symptomatic in only 50% to 60% of men with macroscopic enlargement. Many men symptomatic without macroscopic enlargement; hyperplasia constricts urethral lumen. • Digital palpation for diagnosis is unreliable; half of men with palpable enlargement are symptomatic, and half without palpable enlargement are symptomatic. • Dipstick or microscopic urinalysis to screen for infection or hematuria. • Serum creatinine to check kidney function. • Prostate-specific antigen (PSA) and rectal exam for men age 50 years and older. Black men and men with a first-degree relative with prostate cancer are at higher risk; screen them at age 45 years. • PSA: Normal is <4 ng/mL. PSA greater than 4.0 should be referred to a urologist. Elevation >10 is highly indicative of prostate cancer (90% of cases). Cancer may be present without PSA elevation. Mid-range elevations can occur with BPH, prostatitis, urinary retention, ejaculation, and exercise. • Natural course of untreated disease process: bladder outlet obstruction, urinary retention, kidney damage. Effective treatment, including surgery if needed, is critical. • Surgery: may be indicated in patients who have failed medical therapy or have recurrent infection, hematuria, or renal insufficiency. Transurethral resection of the prostate (TURP) has high rate of morbidity (sexual dysfunction, incontinence, and bleeding). Thermal microwave and laser, to reduce hyperplastic tissue, are also available. These newer procedures are less expensive than TURP with fewer complications, but subsequent therapies are often required. • Lifestyle and exercise: BPH is inversely association with physical activity and is linked to abdominal obesity. Increasing caloric intake increases BPH risk. Higher caloric intake does not increase BPH risk when accompanied by increased physical activity. Benefits of physical activity: increases blood flow to tissues, facilitating waste removal; decreases sympathetic stress responses, relaxing prostatic tissue; reduces abdominal obesity; decreases lower torso pressure; relaxes prostate and rectal region; and improves blood flow through tissues.
Benign Prostatic Hyperplasia
GENERAL CONSIDERATIONS
DIAGNOSTIC CONSIDERATIONS
Urine and Blood Tests
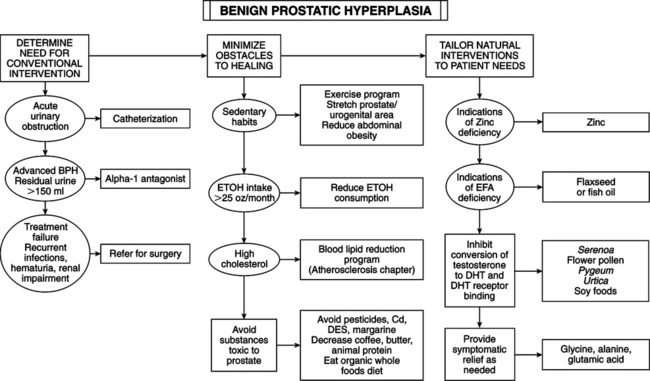
THERAPEUTIC CONSIDERATIONS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
