Benign Proliferative Lesions of the Male Breast
MELISSA P. MURRAY
EDI BROGI
PAPILLOMA
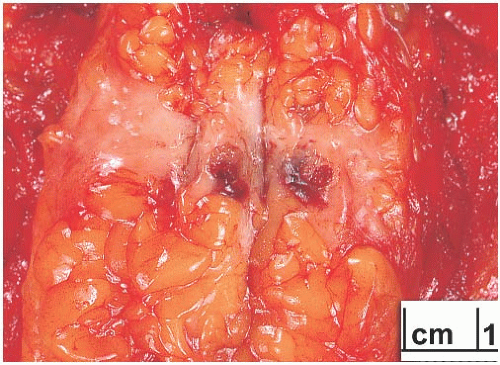
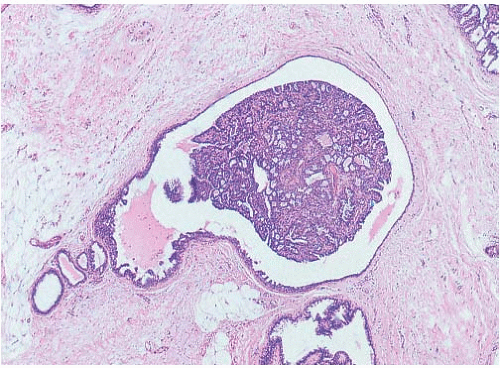
Several examples of intraductal papilloma arising in the male breast have been reported1,2,3,4 (Figs. 35.1 and 35.2). The patients have ranged in age from 3 months to 82 years. The usual presenting symptom is nipple discharge that is bloody or blood tinged. Cystic lesions may be palpable. The ultrasound appearance of benign cystic papillary tumors of the male breast has been documented.5,6,7 One patient treated with phenothiazines for more than 10 years had a multiloculated cystic tumor measuring 7 × 6 × 3 cm that recurred as a 1 × 1 cm cystic lesion 6 months after initial excision.3 Microscopic examination revealed an orderly benign papillary tumor composed of cells with apocrine features and prominent secretory activity. A cystic papilloma described by Shim et al.6 also had apocrine features.
Local recurrence of a multiloculated cystic papilloma in an 82-year-old man was described by David.8 Because of the relatively high proportion of papillary carcinomas of the adult male breast, all male papillary tumors should be carefully evaluated pathologically. It is useful to investigate lowgrade orderly papillary lesions of the male breast that may be papillomas with immunostains for myoepithelial cells, such as smooth muscle actin (SMA), p63, CD10, and cytokeratin (CK) 5/6. The absence of myoepithelium supports the diagnosis of papillary carcinoma, whereas the presence of myoepithelium is consistent with papilloma or papillary DCIS. In the latter circumstance, structural and cytologic features of the epithelium must be relied upon (see Chapters 5 and 14).
FIBROEPITHELIAL TUMORS
Fibroepithelial lesions in the male breast usually arise in patients with gynecomastia.12,13,14,15,16,17,18,19 A number of these patients had been treated with estrogens or antiandrogen therapy, resulting in gynecomastia with lobular differentiation.13,20,21,22 Rare examples of fibroadenoma (FA) have been reported in
transsexual men.17,18 Most PT in men have been histologically and clinically benign. In one case,21 the stromal component of a 30-cm tumor was described as malignant, but the histologic appearance of the lesion was not illustrated.
transsexual men.17,18 Most PT in men have been histologically and clinically benign. In one case,21 the stromal component of a 30-cm tumor was described as malignant, but the histologic appearance of the lesion was not illustrated.
FA occur in the male breast, but in retrospect, many of the lesions described in case reports were poorly documented or appear to have been nodular foci of gynecomastia (Fig. 35.3). Tumors measuring up to 5 cm have been described.16 Four male patients with FA were reported from the Armed Forces Institute of Pathology (AFIP).12 Age at diagnosis in this series ranged from 37 to 71 years. One patient had been treated with estrogens, and another had received methyldopa and chlordiazepoxide. Gynecomastia with lobular differentiation was present microscopically in each case. A particularly unusual patient was a 15-year-old boy with a 7-cm benign fibroepithelial tumor that arose in unilateral gynecomastia.23 He had not received any medications. Gynecomastia was found histologically in the surrounding breast tissue, but there was no evidence of lobular differentiation.
Bilateral FA were described in a 66-year-old man under treatment with Lupron for prostatic carcinoma.19 Cells in the stroma of one FA contained inclusion bodies identical to those found in infantile digital fibromas. A 75-year-old man under treatment for prostate cancer developed a 9-mm mass that increased in size on subsequent imaging. A core biopsy of the mass showed a FA.13 In both cases, the FA arose in a background of gynecomastia.
Nielsen15 documented a 16-cm fibroadenomatoid tumor that arose in one breast of a 69-year-old man with bilateral gynecomastia. The patient had chronic heart disease treated with digoxin and furosemide for 23 years, during which time his breasts appeared clinically normal. Breast enlargement and the appearance of the unilateral tumor began after spironolactone was added to his medication regimen, suggesting that this drug contributed to the mammary lesion. Gynecomastia has been associated with use of digitalis24 and spironolactone.25
DUCT ECTASIA
Duct dilation or ectasia with periductal mastitis, a relatively common condition in the female breast, has also been rarely described in men.1,26,27 Andersen and Gram26 found duct ectasia in 9 (26%) of 35 “normal” breasts and in 19 (35%) of 55 breasts with gynecomastia examined at autopsy. Downs et al.28 have reported a case of duct ectasia in a man with human immunodeficiency virus (HIV) infection, but it is unclear whether the lesion was due to the viral infection or may have been related to some form of estrogen treatment. The histologic appearance is similar in men and women, there being less inflammation and fibrosis in lesions that are clinically asymptomatic.
FIBROCYSTIC CHANGES
Proliferative fibrocystic changes (FCC) resembling those in women are only rarely encountered in the male breast. Several case reports document men who were under 50 years of age at the time of diagnosis.29,30,31,32 Two of the men were described as karyotypically and phenotypically normal.29,30 One patient reported having a swelling of the affected breast for 17 years, which doubled in size during the year prior to biopsy.31 Grossly, each patient had a circumscribed multicystic tumor. The FCC include cysts with apocrine metaplasia, papillary apocrine metaplasia, duct hyperplasia, and duct stasis with mastitis. Gynecomastia was evident histologically in two cases. The gross and microscopic features in these lesions resemble juvenile papillomatosis.31 Sanguinetti et al.33 described a circumscribed, 1.5-cm grossly multicystic lesion with histologic features of juvenile papillomatosis that was excised from a 17-year-old boy. No images of the histopathology were provided.
Sclerosing adenosis (SA) arising in lobules was described as an incidental finding in the postmortem examination of a 41-year-old man with disseminated pulmonary oat cell
carcinoma.34 Grossly, the lesion was a unilateral, firm, white 1.8 × 1.5 × 1.0 cm nodule. Ectopic hormone production was not documented in this case.
carcinoma.34 Grossly, the lesion was a unilateral, firm, white 1.8 × 1.5 × 1.0 cm nodule. Ectopic hormone production was not documented in this case.
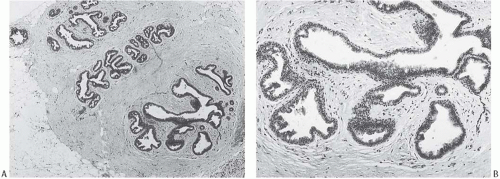 FIG. 35.3. Fibroadenomatoid gynecomastia. A,B: Nodular gynecomastia with early lobular differentiation. The patient was being treated with estrogen for prostatic carcinoma. |
An unusual retroareolar mass in a 38-year-old man proved to be a 2.5-cm cyst lined by benign squamous epithelium.35 There were no skin appendage glands in the cyst wall, and surrounding tissue contained mammary gland ducts.
GYNECOMASTIA
Clinical Presentation
Gynecomastia (gynecain = Greek word for female; mastos = Greek word for breast) is the most common clinical and pathologic abnormality of the male breast. The initial clinical signs of gynecomastia are breast enlargement and a palpable mass that may be accompanied by pain or tenderness in patients with more recent onset. Enlargement of the nipple and areola occurs in a minority of patients. Nipple retraction and discharge are rarely encountered. The palpable mass is located in the central subareolar region in all but a very small number of patients, who have eccentric or peripherally located lesions. On clinical examination, the mass may measure 10 cm or larger, but in most cases it spans 2 to 6 cm in diameter.
Both breasts are affected in the majority of patients with gynecomastia at all ages. Among those with unilateral gynecomastia, the left breast is involved more often than the right.36 Bilateral involvement is usually synchronous, but it may be asynchronous. Patients with bilateral involvement tend to have diffuse lesions, whereas unilateral gynecomastia is more likely to produce a discrete mass. Some patients report pain associated with the mass. In one study,37 administration of gamolenic acid was associated with reduced pain. Clinically, invasive carcinoma arising in gynecomastia can usually be detected as a localized, asymmetric area of firmness.
Radiology
Two mammographic patterns are associated with gynecomastia: a dendritic configuration featuring a retroareolar density with prominent radial extensions and a triangular subareolar density lacking radiating extensions. The triangular pattern is more common in gynecomastia of recent onset, whereas gynecomastia present for 6 months or longer tends to have the dendritic configuration. Mammography is helpful for distinguishing between gynecomastia and carcinoma, and it may identify carcinoma developing in gynecomastia.38 Presently, the combined use of ultrasonography and mammography is considered the optimal approach for evaluating a patient who presents with clinical findings of gynecomastia in order to rule out carcinoma.39,40,41
Etiology
Idiopathic and/or physiologic gynecomastia accounts for the majority of cases. Gynecomastia is fairly common in newborn male infants, reflecting exposure to maternal estrogens. It usually regresses spontaneously in a few weeks. Gynecomastia in prepubertal boys is relatively infrequent,42 but it has been reported in 30% to 40% of adolescent43 and adult males.44,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree