Benign Mesenchymal Neoplasms
MELINDA F. LERWILL
FREDERICK C. KOERNER
FIBROMATOSIS
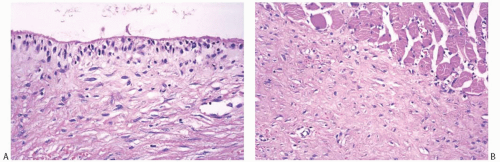
Fibromatosis is an infiltrating, histologically low-grade, spindle cell proliferation composed of fibroblastic cells and variable amounts of collagen. Relatively few instances of fibromatosis originating in the breast or mammary subcutaneous tissue have been reported. With few exceptions,1,2,3,4,5,6 the literature on this subject consists of anecdotal case reports.7,8,9,10,11,12,13,14 Alternative diagnoses used for these lesions include extra-abdominal desmoid, low-grade or grade I fibrosarcoma, and aggressive fibromatosis.
Adair and Herrmann15 referred to a 2-cm mammary “desmoid” in the breast and pectoral muscle of a recently parturient 32-year-old woman in 1946. More than two decades later, Norris and Taylor16 mentioned two tumors with “a desmoid pattern” in a review of mammary sarcomas. One woman was pregnant, and both tumors “appeared to involve the deep dermis secondarily.” Three instances of mammary involvement by fibromatosis were listed by Das Gupta et al.17 in a review of extra-abdominal desmoids. A patient with Gardner syndrome and fibromatosis of the breast was reported in 1964,18 and 6 years later a case of bilateral mammary fibromatosis associated with this genetic syndrome was described.10 Most authors have preferred the term “fibromatosis” rather than “extra-abdominal desmoid tumor” when referring to examples in the breast. Very few of these patients have clinical evidence of Gardner syndrome.
Clinical Presentation
The age of patients with mammary fibromatosis ranged from 14 to 83 years at diagnosis, averaging 37,2 43,3 and 48.71 years, in three reported series. The median age at diagnosis was 25 years in one series,2 and 37.5, 45, and 51 years in others.3,5,6 Females are more commonly affected than men. The lesions are usually painless, but pain and tenderness have been described.13 Patients with mammary fibromatosis almost always present with a palpable, firm or hard tumor in the breast that may suggest carcinoma on clinical examination. When present, dimpling or retraction of the overlying skin may reinforce the clinical impression of carcinoma. The tumor is typically found in one of the quadrants and infrequently in the subareolar area. The left and right breasts are affected with approximately equal frequency. Six patients with bilateral fibromatosis were included among 177 cases (3%) in published series,1,2,3,4,5,6,19 and there are a few other reported examples of bilateral mammary fibromatosis. Only one of these patients had Gardner syndrome.10 The bilateral lesions appear to have been independent processes, because extension across the midline was not reported. With the exception of one woman with asynchronous tumors separated by a 2-year interval, bilateral lesions have been simultaneous. Origin in axillary breast tissue has been reported.11,20 A case of multiple pedunculated lesions described as “fibromatosis of the breast” appears, on review, to be an example of dermatofibrosarcoma protuberans.21
Mammography reveals a stellate tumor that may be indistinguishable from carcinoma.1,3,8,9,11 Calcifications are rarely formed in mammary fibromatosis, but they may be present in a benign proliferative lesion such as sclerosing adenosis (SA) that has been engulfed by the tumor. Rarely, the tumor may be nonpalpable and initially detected by mammography.9,22
Predisposing Factors
Antecedent injury or trauma has been reported at the site of fibromatosis in some patients, but this has been described infrequently for mammary lesions. One patient developed fibromatosis in a breast struck by falling concrete,23 and in another the tumor arose at an operative site 3 years after surgical drainage of postpartum mastitis.8 Also reported are one patient who had prior surgery for a fibroadenoma (FA) and another who had trauma in the area where fibromatosis developed.2 Most studies report low rates of antecedent breast surgery (0% to 6%),2,3,4,5 but in one series of 32 patients with mammary fibromatosis, 44% had a history of prior breast surgery, and fibromatosis was diagnosed at a median of 24 months postoperatively.6 Nevertheless, it appears unlikely that trauma is responsible for the development of mammary fibromatosis in most patients.
An association with breast augmentation implants has been reported in a small number of cases24 (Fig. 38.1). None of the patients is known to have had Gardner syndrome. Fibromatosis has been reported more often in association with silicone implants (14 cases) than with saline ones (6 cases), but this observation may simply reflect the prevalence of silicone implant use.24,25 Tumors are identified at a mean interval of 3 years after implant placement.25 They are typically unilateral and arise in or around the implant
capsule.24 Fibrosarcoma and pleomorphic undifferentiated sarcoma have also been reported to arise at the site of breast implants.24 Current evidence does not suggest that biomaterials by themselves play a causative role in the formation of these mesenchymal neoplasms.24
capsule.24 Fibrosarcoma and pleomorphic undifferentiated sarcoma have also been reported to arise at the site of breast implants.24 Current evidence does not suggest that biomaterials by themselves play a causative role in the formation of these mesenchymal neoplasms.24
Rare examples of mammary fibromatosis have been associated with familial adenomatous polyposis (FAP), a condition in which somatic fibromatosis (desmoid tumor) frequently occurs.10,18,26 FAP is the result of germline mutations in the adenomatous polyposis coli (APC) gene located on chromosome 5q. The APC gene product, the APC tumor suppressor protein, regulates β-catenin, a component of the cadherin cell-to-cell adhesion system and of the Wnt signaling pathway.27 Altered regulation of β-catenin results in its accumulation within the nucleus, where it functions as a transcriptional activator. Somatic mutations in the β-catenin gene can also lead to abnormal accumulation of this protein in the nucleus. Both FAP-associated and sporadic examples of somatic fibromatosis frequently demonstrate nuclear accumulation of β-catenin protein, which can be detected by immunohistochemistry (IHC).
Other potential predisposing genetic conditions are not known. The positive family history of breast carcinoma mentioned in a few case reports9,13 is probably coincidental. Rare patients have had invasive ductal carcinoma (IDC) of the contralateral breast.2 One woman was 22 years old when she developed unilateral mammary fibromatosis 5 years after treatment of Hodgkin disease by chemotherapy alone.2
A number of clinical observations have suggested that hormonal disturbances may contribute to the development of fibromatosis at various sites. Estrogen receptor (ER) expression has been detected via ligand-binding assays in a subset of fibromatosis cases.28




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree