1 Basic Epidemiologic Concepts and Principles
I What is Epidemiology?
Epidemiology can best be understood as the basic science of public health. It provides methods to study disease, injury, and clinical practice. Whereas health care practitioners collect data on a single patient, epidemiologists collect data on an entire population. The scientific methods used to collect such data are described in the Epidemiology section of this text, Chapters 1 to 7, and the methods used to analyze the data are reviewed in the Biostatistics section, Chapters 8 to 13.
The scientific study of disease can be approached at the following four levels:
1. Submolecular or molecular level (e.g., cell biology, genetics, biochemistry, and immunology)
2. Tissue or organ level (e.g., anatomic pathology)
3. Level of individual patients (e.g., clinical medicine)
Investigators involved in clinical epidemiology often use research designs and statistical tools similar to those used by classical epidemiologists. However, clinical epidemiologists study patients in health care settings rather than in the community at large. Their goal is to improve the prevention, early detection, diagnosis, treatment, prognosis, and care of illness in individual patients who are at risk for, or already affected by, specific diseases.1
II Etiology and Natural History of Disease
A Stages of Disease
The development and expression of a disease occur over time and can be divided into three stages: predisease, latent, and symptomatic. During the predisease stage, before the disease process begins, early intervention may avert exposure to the agent of disease (e.g., lead, trans-fatty acids, microbes), preventing the disease process from starting; this is called primary prevention. During the latent stage, when the disease process has already begun but is still asymptomatic, screening for the disease and providing appropriate treatment may prevent progression to symptomatic disease; this is called secondary prevention. During the symptomatic stage, when disease manifestations are evident, intervention may slow, arrest, or reverse the progression of disease; this is called tertiary prevention. These concepts are discussed in more detail in Chapters 15 to 17.
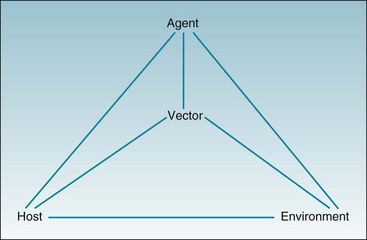
C Host, Agent, Environment, and Vector
The causes of a disease are often considered in terms of a triad of factors: the host, the agent, and the environment. For many diseases, it is also useful to add a fourth factor, the vector (Fig. 1-1). In measles, the host is a human who is susceptible to measles infection, the agent is a highly infectious virus that can produce serious disease in humans, and the environment is a population of unvaccinated individuals, which enables unvaccinated susceptible individuals to be exposed to others who are infectious. The vector in this case is relatively unimportant. In malaria, however, the host, agent, and environment are all significant, but the vector, the Anopheles mosquito, assumes paramount importance in the spread of disease.
Vectors of disease include insects (e.g., mosquitoes associated with spread of malaria), arachnids (e.g., ticks associated with Lyme disease), and mammals (e.g., raccoons associated with rabies in eastern U.S.). The concept of the vector can be applied more widely, however, to include human groups (e.g., vendors of heroin, cocaine, and methamphetamine) and even inanimate objects that serve as vehicles to transmit disease (e.g., contaminated needles associated with hepatitis and AIDS). A vector may be considered part of the environment, or it may be treated separately (see Fig. 1-1). To be an effective transmitter of disease, the vector must have a specific relationship to the agent, the environment, and the host.
D Risk Factors and Preventable Causes
Risk factors for disease and preventable causes of disease, particularly life-threatening diseases such as cancer, have been the subject of much epidemiologic research. In 1964 a World Health Organization (WHO) expert committee estimated that the majority of cancer cases were potentially preventable and were caused by “extrinsic factors.” Also that year, the U.S. Surgeon General released a report indicating that the risk of death from lung cancer in smokers was almost 11 times that in nonsmokers.2
Advances in knowledge have consolidated the WHO findings to the point where few, if any, researchers now question its main conclusion.3 Indeed, some have gone further, substituting figures of 80% or even 90% as the proportion of potentially preventable cancers, in place of WHO’s more cautious estimate of the “majority.” Unfortunately, the phrase “extrinsic factors” (or its near-synonym, “environmental factors”) has often been misinterpreted to mean only man-made chemicals, which was certainly not the intent of the WHO committee. In addition to man-made or naturally occurring carcinogens, the 1964 report included viral infections, nutritional deficiencies or excesses, reproductive activities, and a variety of other factors determined “wholly or partly by personal behavior.”
1 BEINGS Model
The acronym BEINGS can serve as a mnemonic device for the major categories of risk factors for disease, some of which are easier to change or eliminate than others (Box 1-1). Currently, genetic factors are among the most difficult to change, although this field is rapidly developing and becoming more important to epidemiology and prevention. Immunologic factors are usually the easiest to change, if effective vaccines are available.
“B”—Biologic and Behavioral Factors
Increasing attention has focused on the rapid increase in overweight and obesity in the U.S. population over the past two decades. The number of deaths per year that can be attributed to these factors is controversial. In 2004 the U.S. Centers for Disease Control and Prevention (CDC) estimated that 400,000 deaths annually were caused by obesity and its major risk factors, inactivity and an unhealthy diet.4 In 2005, using newer survey data and controlling for more potential confounders, other CDC investigators estimated that the number of deaths attributable to obesity and its risk factors was only 112,000.5 Regardless, increasing rates of obesity are found worldwide as part of a cultural transition related to the increased availability of calorie-dense foods and a simultaneous decline in physical activity, resulting in part from mechanized transportation and sedentary lifestyles.6–11
Obesity and overweight have negative health effects, particularly by reducing the age at onset of, and increasing the prevalence of, type 2 diabetes. Obesity is established as a major contributor to premature death in the United States,12,13 although the exact magnitude of the association remains controversial, resulting in part from the complexities of the causal pathway involved (i.e., obesity leads to death indirectly, by contributing to the development of chronic disease).
Multiple behavioral factors are associated with the spread of some diseases. In the case of AIDS, the spread of human immunodeficiency virus (HIV) can result from unprotected sexual intercourse between men and from shared syringes among intravenous drug users, which are the two predominant routes of transmission in the United States. HIV infection can also result from unprotected vaginal intercourse, which is the predominant transmission route in Africa and other parts of the world. Other behaviors that can lead to disease, injury, or premature death (before age 65) are excessive intake of alcohol, abuse of both legal and illegal drugs, driving while intoxicated, and homicide and suicide attempts. In each of these cases, as in cigarette smoking and HIV infection, changes in behavior could prevent the untoward outcomes. Many efforts in health promotion depend heavily on modifying human behavior, as discussed in Chapter 15.
“E”—Environmental Factors
Epidemiologists are frequently the first professionals to respond to an apparent outbreak of new health problems, such as legionnaires’ disease and Lyme disease, which involve important environmental factors. In their investigations, epidemiologists describe the patterns of the disease in the affected population, develop and test hypotheses about causal factors, and introduce methods to prevent further cases of disease. Chapter 3 describes the standard approach to investigating an epidemic.
“N”—Nutritional Factors
In the 1950s it was shown that Japanese Americans living in Hawaii had a much higher rate of MI than people of the same age and gender in Japan, while Japanese Americans in California had a still higher rate of MI than similar individuals in Japan.14–16 The investigators believed that dietary variations were the most important factors producing these differences in disease rates, as generally supported by subsequent research. The Japanese eat more fish, vegetables, and fruit in smaller portions.
Denis Burkitt, the physician after whom Burkitt’s lymphoma was named, spent many years doing epidemiologic research on the critical role played by dietary fiber in good health. From his cross-cultural studies, he made some stunning statements, including the following17:
“By world standards, the entire United States is constipated.”
“Don’t diagnose appendicitis in Africa unless the patient speaks English.”
“African medical students go through five years of training without seeing coronary heart disease or appendicitis.”
“Populations with large stools have small hospitals. Those with small stools have large hospitals.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree