Bariatric Surgery1
Kevin Tymitz
Thomas Magnuson
Michael Schweitzer
1Abbreviations: BMI, body mass index; D-RYGB, distal Roux-en-Y gastric bypass; DS-BPD, duodenal switch with biliopancreatic diversion; IF, intrinsic factor; JIB, jejunoileal bypass; LAGB, laparoscopic adjustable gastric band; LVSG, laparoscopic vertical sleeve gastrectomy; RYGB, Roux-en-Y gastric bypass; TPN, total parenteral nutrition.
Obesity is a significant health concern in this country. It is a disease that is created by a multitude of genetic and environmental factors. The consequences of obesity are as equally complex as its etiology, affecting every organ system in the human body as well as imposing serious psychological stress often associated with social isolation, depression, and numerous other psychologic comorbidities. Medical management, unfortunately, usually fails to achieve sustained weight loss; and currently, bariatric surgical procedures are the most effective means to achieve sustained weight loss and also provide durable treatment of obesity-associated morbidities.
Weight-loss surgery is not a simple “cure” for this very complex and debilitating disease. It does, however, provide a powerful tool for patients to achieve success. A successful long-term outcome depends on the patient’s commitment to a lifetime of dietary and lifestyle changes. For this reason, there must be a multidisciplinary approach that includes surgeons, primary care physicians, psychologists, nurses, and dietitians to provide critical instructions to help patients adhere to the dietary and lifestyle changes consistent with the surgery.
The several types of bariatric surgery differ in expected outcomes in terms of weight loss and the likelihood of predisposing patients to nutritional deficiencies postoperatively. To understand these deficiencies and their appropriate management fully, it is imperative to understand the origin of the deficit. The purpose of this chapter is to review the various surgical procedures currently offered and the potential nutritional deficiencies that may ensue. Health care professionals must be aware of these deficiencies and the practice guidelines that must be followed to prevent these deficiencies because some of them may have serious consequences.
OVERVIEW
The prevalence of obesity continues to increase at an alarming rate throughout industrialized nations. Obesity is a disease that affects 34% of adults 20 years old and older in the United States, and this amounts to more than 72 million people. Approximately 33.3% of US men and about 35.3% of US women are obese. Nearly 6% of adults are classified as morbidly obese, with a body mass index (BMI) greater than 40 (1).
Obesity is a leading preventable cause of death worldwide, with increasing prevalence in adults and children. It is viewed as one of the most serious public health problems of the twenty-first century. Obesity is stigmatized in much of the modern world (particularly in the Western world), although it was widely perceived as a symbol of wealth and fertility at other times in history and still is in some parts of the world.
Health care professionals need to be concerned about the prevalence of obesity because of the well-established relationships between excess body weight and serious medical conditions such as type 2 diabetes, hypertension, and heart disease, just to name a few. These relationships have long been established in the adult obese population and more recently also have been observed at an increasing rate in the adolescent population.
Unfortunately, no single solution to prevent or treat obesity is beneficial for everyone. Treatment of obesity
may include a combination of diet, exercise, behavior modification, and medications. For most patients, although these methods may provide a moderate amount of weight loss, the benefits are usually short lived. Hence, bariatric surgery has evolved over the past couple of decades and has been shown to be effective in reducing obesity-related comorbidities, improving the quality of life, and decreasing the number of sick days, monthly medication costs, and overall mortality. With the increasing rates of weight loss procedures, the quality, efficacy, and surgical outcomes have improved with the creation of Bariatric Centers of Excellence designated by the American Society of Metabolic and Bariatric Surgery and the American College of Surgeons. The benefits of bariatric procedures in morbidly obese patients outweigh the risks. With the advent of minimally invasive surgical procedures, bariatric surgery is a reasonable treatment option in those who strongly desire substantial weight loss and have life-threatening comorbid conditions.
may include a combination of diet, exercise, behavior modification, and medications. For most patients, although these methods may provide a moderate amount of weight loss, the benefits are usually short lived. Hence, bariatric surgery has evolved over the past couple of decades and has been shown to be effective in reducing obesity-related comorbidities, improving the quality of life, and decreasing the number of sick days, monthly medication costs, and overall mortality. With the increasing rates of weight loss procedures, the quality, efficacy, and surgical outcomes have improved with the creation of Bariatric Centers of Excellence designated by the American Society of Metabolic and Bariatric Surgery and the American College of Surgeons. The benefits of bariatric procedures in morbidly obese patients outweigh the risks. With the advent of minimally invasive surgical procedures, bariatric surgery is a reasonable treatment option in those who strongly desire substantial weight loss and have life-threatening comorbid conditions.
Definition of Morbid Obesity
The definition and classification of obesity are based on calculation of the BMI—calculated as weight in kilograms divided by height in meters squared. For the majority of the population (except athletes), BMI provides a reliable indicator of the body fat composition. It is used to stratify patients into categories that may lead to health problems. Patients with a BMI of 30 to 35 kg/m2 are considered to have class I obesity, a BMI of 35 to 40 kg/m2 is class II, and a BMI higher than 40 kg/m2 is class III. Morbid obesity is defined as a BMI of 40 kg/m2 or higher or a BMI of 35 kg/m2 or higher in patients with comorbidities. Patients are defined as suffering from superobesity or megaobesity if their BMI is higher than 50 or 70 kg/m2, respectively.
Indications
The National Institutes of Health issued a consensus statement in 1991 (2) regarding the effectiveness of bariatric surgery. The statement outlined patient selection criteria that are still in place today (Table 60.1). Patients are considered candidates for bariatric surgery if they have a BMI of 40 kg/m2 or greater or a BMI between 35 and 40 kg/m2 if an obesity-related comorbid condition exists, such as diabetes or hypertension. In general, appropriate candidates for surgery should demonstrate prior unsuccessful attempts at medically supervised weight reduction programs and should have realistic expectations regarding the long-term outcomes achieved with the surgery. Relative contraindications include an inability to comply with postoperative requirements and follow-up, active alcohol or substance abuse, and uncontrolled psychiatric disease.
TABLE 60.1 INDICATIONS FOR BARIATRIC SURGERY FOR MORBID OBESITY | ||
|---|---|---|
|
Preoperative Assessment of the Obese Patient
The evaluation of potential patients for bariatric surgery should involve a multidisciplinary team approach. This team should include a dietitian and a mental health professional familiar with bariatric surgery. Their purposes are to obtain a complete past dietary and behavioral eating history, educate the patient on postoperative dietary expectations, examine the social support structure, and ensure that any psychiatric or behavioral disorders are optimally controlled. At the Johns Hopkins Center for Bariatric Surgery in Baltimore, all patients are required to attend a multidisciplinary preoperative education seminar. Postoperative participation in support groups is also encouraged.
Nutritional Deficits in the Obese Patient
Nutritional assessment must be an essential part of the preoperative evaluation of the obese patient. Despite the increased caloric intake of the obese population, many suffer from various nutritional deficiencies, particularly the morbid obese with a BMI higher than 40. Consumption of excess calories does not usually correlate with overconsumption of fresh fruits and vegetables or high-quality, nutrient-dense foods. Instead, this more likely correlates with the consumption of higher calorie processed foods that are of low nutritional quality that is very common in developed countries such as the United States. In fact, it is estimated that 27% to 30% of the daily caloric intake of the average US adult or child consists of these low-nutrient-dense food sources, with sweeteners and desserts contributing an estimated 18% to 24% of the total (3, 4).
As the obesity epidemic continues to flourish, obesity should be recognized as a risk factor for many nutrient deficiencies. For example, obese individuals tend to have lower mean levels of vitamin D and calcium compared with lean subjects (5). There are many theories behind this observation including decreased consumption of vitamin D-fortified milk, sedentary lifestyle, reduced exposure to sunlight, and sequestration of the lipid-soluble vitamin in the excess adipose tissue, which can be verified by studies that show serum 25-hydroxyvitamin D (25[OH]D) levels to be inversely proportional to increasing fat mass (6, 7). Decreased vitamin D levels can have deleterious effects on the immune system and may play a role in increasing
the risk of cancers, diabetes mellitus, autoimmune diseases, and cardiovascular disease (8). It is estimated that 25% to 80% of adult patients before bariatric surgery may have baseline vitamin D deficiency (9, 10). Other studies looking at baseline nutritional deficits of adults presenting for bariatric surgery also showed decreased levels of the other fat-soluble vitamins A, K, and E (11, 12).
the risk of cancers, diabetes mellitus, autoimmune diseases, and cardiovascular disease (8). It is estimated that 25% to 80% of adult patients before bariatric surgery may have baseline vitamin D deficiency (9, 10). Other studies looking at baseline nutritional deficits of adults presenting for bariatric surgery also showed decreased levels of the other fat-soluble vitamins A, K, and E (11, 12).
Low vitamin B12 levels have been reported in up to 18% of severely obese adults (13), and vitamin B1 (thiamin) deficiency has been noted in up to 29% of patients undergoing bariatric surgery (9). Deficiencies of other B vitamins are not currently known because they are not frequently included in screening. Unfortunately, depending on the type of surgical procedure and compliance with postoperative supplementation, these deficiencies can become highly exacerbated.
TYPES OF PROCEDURES
The dramatic growth in bariatric surgical procedures performed over the past couple of decades can be attributed to many factors. Increased patient acceptance is one major factor, and it can be attributed in large part to the introduction of laparoscopic and minimally invasive surgical techniques. Significant advantages are offered with laparoscopic and minimally invasive surgery such as less pain, fewer wound complications, and early recovery with relatively low complication rates. Advances in anesthesia, critical care, and parenteral nutrition are other milestones in the success of bariatric procedures.
The bariatric surgical options can be classified into the following three categories: restrictive procedures, malabsorptive procedures, and combined restrictive and malabsorptive procedures. Purely restrictive procedures depend on restriction of the amount of food that enters the foregut. In contrast, malabsorptive procedures depend on the malabsorption of nutrients by bypassing various segments of the small intestine. Combined restrictive and malabsorptive procedures are a combination of the two.
Purely Restrictive Procedures
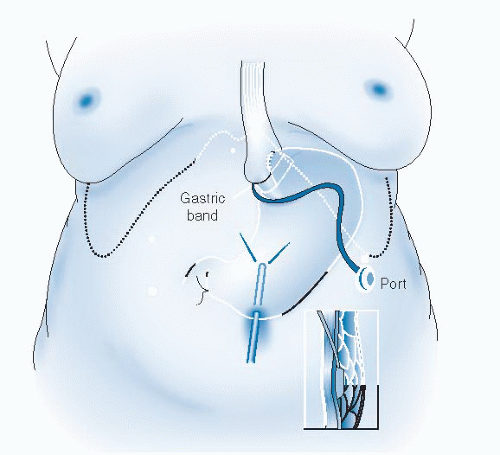
The laparoscopic adjustable gastric band (LAGB) received Food and Drug Administration approval in 2001 and has been in clinical use in the United States since that time. The LAGB is the only device that is adjustable after surgery, thus allowing for tightening or loosening of the band through a subcutaneous port placed for fluid injection. Other advantages of the band include relative ease of placement, lack of operative staple lines or need for bowel transection, and reversibility. The band does require, however, an average of five to six adjustments in the first year after surgery; and its success depends in part on patient compliance and close follow-up.
Dissection for the LAGB (Fig. 60.1) is first performed bluntly at the angle of His, thus freeing up attachments for later insertion of the band. The gastrohepatic ligament is then opened, and the plane posterior to the gastroesophageal junction is bluntly dissected. The adjustable band is placed in the abdomen through a trocar in the left upper quadrant and is secured around the gastroesophageal junction, with a slightly diagonal orientation up toward the angle of His. One to four sutures are then placed from the fundus to the proximal stomach around the band, to secure the band in place and minimize the possibility of band migration or herniation. The band tubing is brought out through the left upper quadrant trocar site, where it is secured to the subcutaneous injection port. Fascia is cleared in this area, and the port is secured to the fascia with care taken not to entrap or kink the band tubing. The band is left empty until 6 weeks postoperatively, when patients receive their first fill. Frequent office visits are usually necessary, especially over the first year, for fluid fills or removal to obtain an appropriate restriction with food ingestion to sustain an appropriate weight loss.
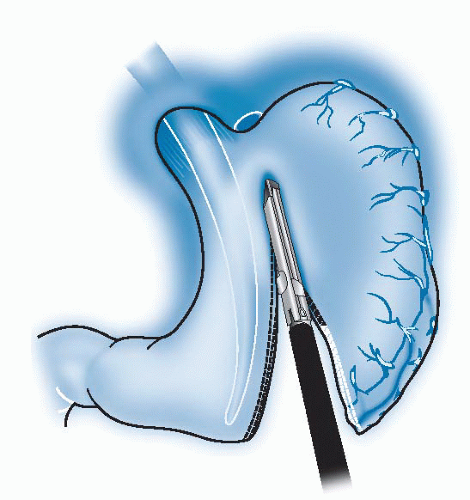
Of the commonly performed bariatric procedures, the laparoscopic vertical sleeve gastrectomy (LVSG) is the most recently introduced, and only limited outcomes data (5 years) are available. Unlike the band, the LVSG does not involve an implanted foreign body that can potentially erode or migrate, and it does not require frequent adjustments. The sleeve resection may also achieve weight loss by affecting satiety. Serum levels of ghrelin, a proappetite hormone produced in the fundus, are reduced after the LVSG because that area of the stomach has been resected. In addition, the sleeve procedure is not reversible because a partial gastrectomy is performed, but it can be converted to a gastric bypass or duodenal switch later if greater weight loss is desired.
The LVSG (Fig. 60.2) is performed by first dividing the short gastric vessels along the greater curve of the stomach beginning near the antrum and extending to the angle of His. A 40F bougie is placed in the stomach and is directed along the lesser curve. The stomach is then divided with the laparoscopic stapler by using the bougie as a guide, beginning 6 cm from the pylorus on the greater curve side and continuing up to the angle of His. The lateral stomach specimen is then removed from one of the trocar sites.
Malabsorptive Procedures
Jejunoileal bypass (JIB) is a purely restrictive procedure that was very common in the 1960s and 1970s despite lack of scientific study of its mechanism of action. This particular procedure bypasses approximately 90% of the small intestine. The proposed mechanism of action was induced weight loss by a surgically induced short gut syndrome. This procedure is based on canine studies performed in the mid-1950s that showed that 50% of the small intestine in dogs can be removed without apparent effects, with profound interference with fat absorption associated with weight loss (14). Many complications were associated with bypassing a large portion of the small intestine, however. Patients suffered frequent flatulence and diarrhea secondary to bypassing the site of bile acid reabsorption. Electrolyte deficiencies were common secondary to loss of potassium, calcium, and magnesium. Various vitamin deficiencies frequently led to neuropathies, bone demineralization, and protein malnutrition. Exposure of colonic mucosa to excessive bile salts created calcium oxalate renal stones. In addition, bacterial overgrowth in the bypassed small intestine led to hepatic decomposition and arthritis. It was later determined that the actual mechanism of action of weight loss from this procedure was learned behavior. The rectal complications and intense anal irritation from the diarrhea led to patients’ changes in eating habits (15). Patients learned very quickly that, to function in society, they had to consume only minimal fat and nutrients before venturing away from their homes. For these reasons, the JIB procedure has long been abandoned, but it did pave the way for the more recent techniques of bariatric surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree