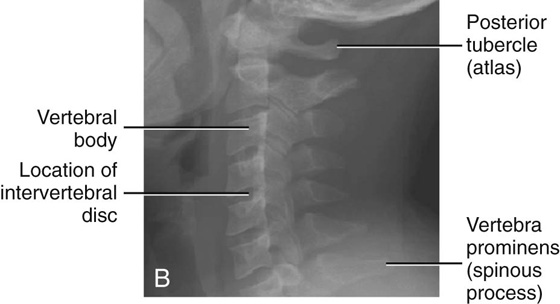
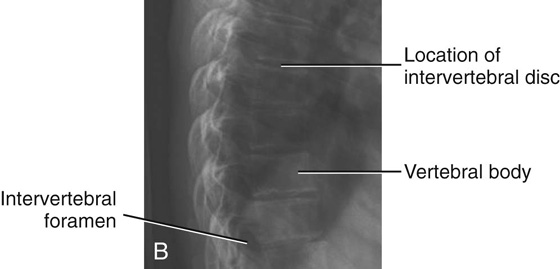
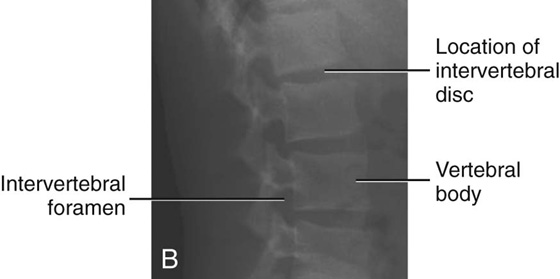
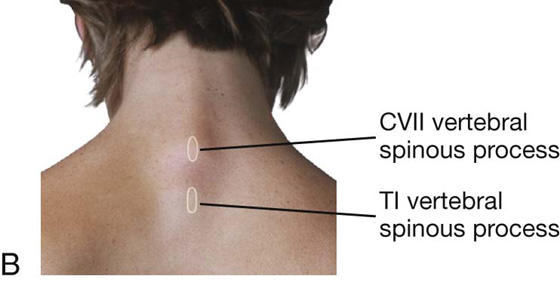
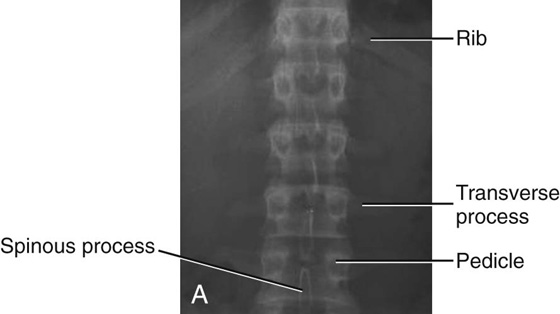
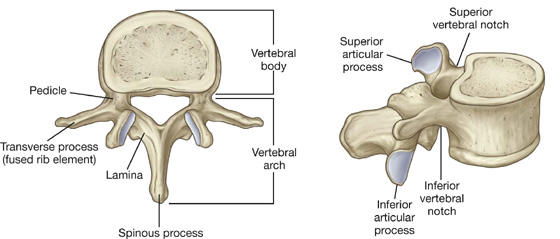
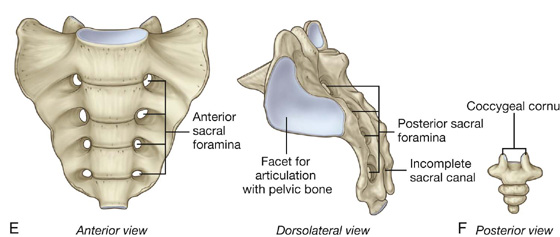
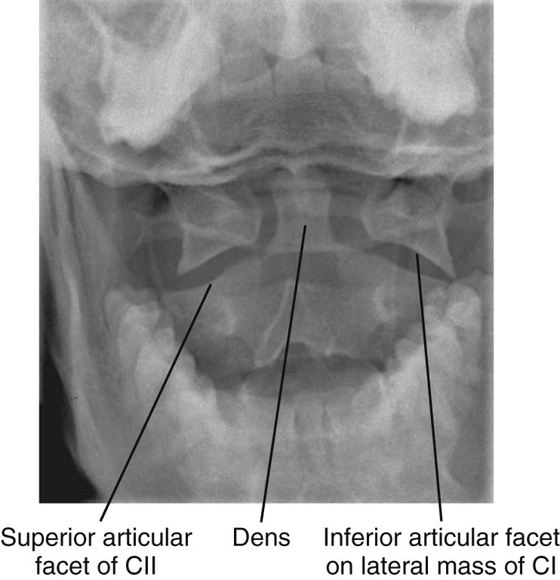
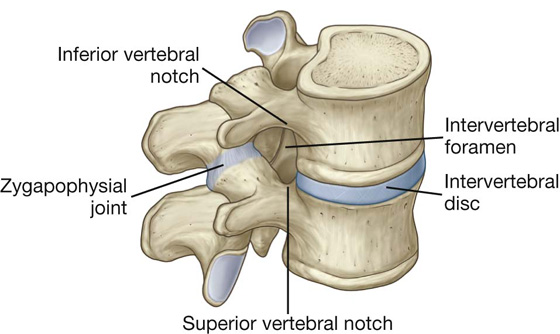
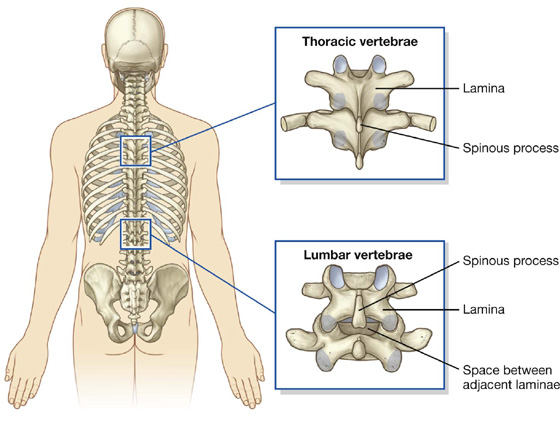
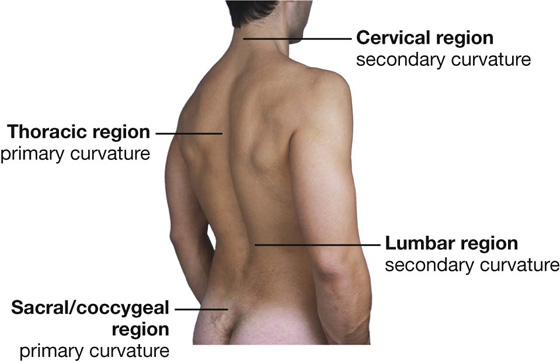
2 Posterior spaces between vertebral arches Curvatures of vertebral column Joints between vertebrae in the back Anterior and posterior longitudinal ligaments Supraspinous ligament and ligamentum nuchae Superficial group of back muscles Intermediate group of back muscles Arrangement of structures in the vertebral canal Cervical degenerative joint disease The back consists of the posterior aspect of the body and provides the musculoskeletal axis of support for the trunk. The back also contains the spinal cord and proximal parts of the spinal nerves, which send and receive information to and from most of the body. Skeletal components of the back consist mainly of the vertebrae and associated intervertebral discs. The skull, scapulae, pelvic bones (ileum, ischium, pubis), and ribs also contribute to the bony framework of the back and provide sites for muscle attachment. There are approximately 33 vertebrae, which are subdivided into five groups based on morphology and location (Fig. 2.1): Fig. 2.1 Vertebrae. Imaging app Typical cervical vertebrae Fig. 2.2 Radiographs of cervical region of vertebral column. A. Anterior-posterior view. B. Lateral view. Imaging app Typical thoracic vertebrae Fig. 2.3 Radiograph of thoracic region of vertebral column. A. Anterior-posterior view. B. Lateral view. Imaging app Typical lumbar vertebrae Fig. 2.4 Radiograph of lumbar region of vertebral column. A. Anterior-posterior view. B. Lateral view. A typical vertebra consists of a vertebral body and a posterior vertebral arch (Fig. 2.5). Extending from the vertebral arch are a number of processes for muscle attachment and articulation with adjacent bone. Fig. 2.5 Typical vertebra. The vertebral body is the weightbearing part of the vertebra and is linked to adjacent vertebral bodies by intervertebral discs and ligaments. The size of vertebral bodies increases inferiorly as the amount of weight supported increases. The vertebral arch forms the lateral and posterior parts of the vertebral foramen. The vertebral foramina of all the vertebrae together form the vertebral canal, which contains and protects the spinal cord. Superiorly, the vertebral canal is continuous, through the foramen magnum of the skull, with the cranial cavity of the head. The vertebral arch of each vertebra consists of pedicles and laminae (Fig. 2.5): A spinous process projects posteriorly and inferiorly from the junction of the two laminae and is a site for muscle and ligament attachment. A transverse process extends posterolaterally from the junction of the pedicle and lamina on each side and is a site for articulation with ribs in the thoracic region. Also projecting from the region where the pedicles join the laminae are superior and inferior articular processes (Fig. 2.5), which articulate with the inferior and superior articular processes, respectively, of adjacent vertebrae. Between the vertebral body and the origin of the articular processes, each pedicle is notched on its superior and inferior surfaces. These superior and inferior vertebral notches participate in forming intervertebral foramina. The seven cervical vertebrae are characterized by their small size and by the presence of a foramen in each transverse process. A typical cervical vertebra has the following features (Fig. 2.6A): The first and second cervical vertebrae—the atlas and axis—are specialized to accommodate movement of the head. Vertebra CI (the atlas) articulates with the head (Figs. 2.6B, 2.7). Its major distinguishing feature is that it lacks a vertebral body (Fig. 2.6B). In fact, the vertebral body of CI fuses onto the body of CII during development to become the dens of CII. As a result, there is no intervertebral disc between CI and CII. When viewed from above, the atlas is ring shaped and composed of two lateral masses interconnected by an anterior arch and a posterior arch. Each lateral mass articulates above with an occipital condyle of the skull and below with the superior articular process of vertebra CII (the axis). The superior articular facets are bean shaped and concave, whereas the inferior articular facets are almost circular and flat. The atlanto-occipital joint allows the head to nod up and down on the vertebral column. The posterior surface of the anterior arch has an articular facet for the dens, which projects superiorly from the vertebral body of the axis. The dens is held in position by a strong transverse ligament of atlas posterior to it and spanning the distance between the oval attachment facets on the medial surfaces of the lateral masses of the atlas (Fig. 2.6B). Imaging app Articulation between atlas and axis Fig. 2.7 Radiograph showing CI (atlas) and CII (axis) vertebrae. Open mouth, anterior-posterior (odontoid peg) view. How to identify specific vertebral spinous processes Identification of vertebral spinous processes (Fig. 2.8A) can be used to differentiate between regions of the vertebral column and facilitate visualizing the position of deeper structures, such as the inferior ends of the spinal cord and subarachnoid space. The spinous process of vertebra CII can be identified through deep palpation as the most superior bony protuberance in the midline inferior to the skull. Most of the other spinous processes, except for that of vertebra CVII, are not readily palpable because they are obscured by soft tissue. The spinous process of CVII is usually visible as a prominent eminence in the midline at the base of the neck (Fig. 2.8B), particularly when the neck is flexed. Inferior to the spinous process of CVII is the spinous process of TI, which is also usually visible as a midline protuberance. Often it is more prominent than the spinous process of CVII. The root of the spine of the scapula is at the same level as the spinous process of vertebra TIII, and the inferior angle of the scapula is level with the spinous process of vertebra TVII. The spinous process of vertebra TXII is level with the midpoint of a vertical line between the inferior angle of the scapula and the iliac crest. A horizontal line between the highest point of the iliac crest on each side crosses through the spinous process of vertebra LIV. The LIII and LV vertebral spinous processes can be palpated above and below the LIV spinous process, respectively. The sacral dimples that mark the position of the posterior superior iliac spine are level with the SII vertebral spinous process. The tip of the coccyx is palpable at the base of the vertebral column between the gluteal masses. The tips of the vertebral spinous processes do not always lie in the same horizontal plane as their corresponding vertebral bodies. In thoracic regions, the spinous processes are long and sharply sloped downward so that their tips lie at the level of the vertebral body below. In other words, the tip of the TIII vertebral spinous process lies at vertebral level TIV. In lumbar and sacral regions, the spinous processes are generally shorter and less sloped than in thoracic regions, and their palpable tips more closely reflect the position of their corresponding vertebral bodies. As a consequence, the palpable end of the spinous process of vertebra LIV lies at approximately the LIV vertebral level. The dens acts as a pivot that allows the atlas and attached head to rotate on the axis, side to side. The transverse processes of the atlas are large and protrude farther laterally than those of the other cervical vertebrae. They act as levers for muscle action, particularly for muscles that move the head at the atlanto-axial joints. The axis is characterized by the large toothlike dens, which extends superiorly from the vertebral body (Figs. 2.6B and 2.7). The anterior surface of the dens has an oval facet for articulation with the anterior arch of the atlas. The two superolateral surfaces of the dens possess circular impressions that serve as attachment sites for strong alar ligaments, one on each side, which connect the dens to the medial surfaces of the occipital condyles. These alar ligaments check excessive rotation of the head and atlas relative to the axis (Fig. 2.6B). The twelve thoracic vertebrae are all characterized by their articulation with ribs. A typical thoracic vertebra has two partial facets (superior and inferior costal facets) on each side of the vertebral body for articulation with the head of its own rib and the head of the rib below (Fig. 2.6C). The superior costal facet is much larger than the inferior costal facet. Each transverse process also has a facet (transverse costal facet) for articulation with the tubercle of its own rib. The vertebral body of the vertebra is somewhat heart-shaped when viewed from above, and the vertebral foramen is circular. The five lumbar vertebrae are distinguished from vertebrae in other regions by their large size (Fig. 2.6D). Also, they lack facets for articulation with ribs. The transverse processes are generally thin and long, with the exception of those on vertebra LV, which are massive and somewhat cone-shaped for the attachment of iliolumbar ligaments to connect the transverse processes to the pelvic bones. The vertebral body of a typical lumbar vertebra is cylindrical and the vertebral foramen is triangular in shape and larger than in the thoracic vertebrae. The sacrum is a single bone that represents the five fused sacral vertebrae (Fig. 2.6E). It is triangular in shape with the apex pointed inferiorly, and is curved so that it has a concave anterior surface and a correspondingly convex posterior surface. It articulates above with vertebra LV and below with the coccyx. It has two large L-shaped facets, one on each lateral surface, for articulation with the pelvic bones. The posterior surface of the sacrum has four pairs of posterior sacral foramina, and the anterior surface has four pairs of anterior sacral foramina for the passage of the posterior and anterior rami, respectively, of S1 to S4 spinal nerves. The posterior wall of the vertebral canal may be incomplete near the inferior end of the sacrum. The coccyx is a small triangular bone that articulates with the inferior end of the sacrum and represents three to four fused coccygeal vertebrae (Fig. 2.6F). It is characterized by its small size and by the absence of vertebral arches and therefore a vertebral canal. Intervertebral foramina are formed on each side between adjacent parts of vertebrae and associated intervertebral discs (Fig. 2.9). The foramina allow structures, such as spinal nerves and blood vessels, to pass in and out of the vertebral canal. Fig. 2.9 Intervertebral foramen. An intervertebral foramen is formed by the inferior vertebral notch on the pedicle of the vertebra above and the superior vertebral notch on the pedicle of the vertebra below. The foramen is bordered: Each intervertebral foramen is a confined space surrounded by bone, ligaments, and joints. Pathology in any of these structures, and in the surrounding muscles, can affect structures within the foramen. In most regions of the vertebral column, the laminae and spinous processes of adjacent vertebrae overlap to form a reasonably complete bony posterior (dorsal) wall for the vertebral canal. However, in the lumbar region, large gaps exist between the posterior components of adjacent vertebral arches (Fig. 2.10). These gaps between adjacent laminae and spinous processes become increasingly wide from vertebra LI to vertebra LV. The spaces can be widened further by flexion of the vertebral column. These gaps allow relatively easy access to the vertebral canal for clinical procedures. Fig. 2.10 Spaces between adjacent vertebral arches in the lumbar region. The vertebral column has a number of curvatures (Fig. 2.11): Fig. 2.11 Curvatures of the vertebral column. Surface anatomy Primary and secondary curvatures in the sagittal plane When viewed from the side, the normal vertebral column has primary curvatures in the thoracic and sacral/coccygeal regions and secondary curvatures in the cervical and lumbar regions (Fig. 2.12). The primary curvatures are concave anteriorly. The secondary curvatures are concave posteriorly. Clinical app Spina bifida Spina bifida is a disorder in which the two sides of vertebral arches, usually in lower vertebrae, fail to fuse during development, resulting in an “open” vertebral canal. There are two types of spina bifida. Clinical app Vertebroplasty Vertebroplasty is a new technique in which the body of a vertebra can be filled with bone cement (typically methyl methacrylate). The indications for the technique include vertebral body collapse and pain from the vertebral body, which may be secondary to tumor infiltration. The procedure is most commonly performed for osteoporotic wedge fractures, which are a considerable cause of morbidity and pain in older patients. These types of fractures typically occur at the thoracolumbar region. Clinical app Scoliosis Scoliosis is an abnormal lateral curvature of the vertebral column (Fig. 2.13). Fig. 2.13 Radiograph of thoracic scoliosis. A true scoliosis involves not only the (right- or left-sided) curvature but also a rotational element of one vertebra on another. The commonest types of scoliosis are those for which we have little understanding about how or why they occur and are termed idiopathic scoliosis. These are never present at birth and tend to occur in either the infantile, juvenile, or adolescent age groups. The vertebral bodies and posterior elements (pedicles and laminae) are normal in these patients. Clinical app Kyphosis Kyphosis is abnormal curvature (exaggerated anterior concavity) of the vertebral column in the thoracic region, producing a “hunchback” deformity. This condition occurs in certain disease states, the most dramatic of which is usually secondary to tuberculosis infection of a thoracic vertebral body, where the kyphosis becomes angulated at the site of the lesion. Clinical app Lordosis Lordosis is abnormal curvature (exaggerated posterior concavity) of the vertebral column in the lumbar region, producing a swayback deformity. Clinical app Variation in vertebral numbers There are usually seven cervical vertebrae, although in certain diseases these may be fused. Fusion of cervical vertebrae can be associated with other abnormalities in which there is abnormal fusion of vertebrae CI and CII or CV and CVI. Variations in the number of thoracic vertebrae are well described. One of the commonest abnormalities in the lumbar vertebrae is a partial fusion of vertebra LV with the sacrum (sacralization of the lumbar vertebra). Partial separation of vertebra SI from the sacrum (lumbarization of first sacral vertebra) may also occur. A hemivertebra occurs when a vertebra develops only on one side. Clinical app The vertebrae and cancer The vertebrae are common sites for metastatic disease (secondary spread of cancer cells). When cancer cells grow within the vertebral bodies and the posterior elements, they destroy the mechanical properties of the bone. Importantly, vertebrae that contain extensive metastatic disease may extrude fragments of tumor into the vertebral canal, compressing the nerves and spinal cord. Clinical app Osteoporosis Osteoporosis is a pathophysiological condition in which bone quality is normal, but the quantity of bone is deficient. It is a metabolic bone disorder that commonly occurs in women in their 50s and 60s and in men in their 70s. Typical complications of osteoporosis include “crush” vertebral body fractures, distal radial fractures, and hip fractures.
Back
 Image Library—illustrations of back anatomy, Chapter 2
Image Library—illustrations of back anatomy, Chapter 2
 Self-Assessment—National Board style multiple-choice questions, Chapter 2
Self-Assessment—National Board style multiple-choice questions, Chapter 2
 Short Questions—these are questions requiring short responses, Chapter 2
Short Questions—these are questions requiring short responses, Chapter 2
 Interactive Surface Anatomy—interactive surface animations, Chapter 2
Interactive Surface Anatomy—interactive surface animations, Chapter 2
Regional anatomy
SKELETAL FRAMEWORK
Vertebrae
 The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size, bifid spinous processes, and the presence of a foramen in each transverse process (Figs. 2.1, 2.2).
The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size, bifid spinous processes, and the presence of a foramen in each transverse process (Figs. 2.1, 2.2).
 The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.1, 2.3); ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae; although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax.
The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.1, 2.3); ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae; although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax.
 Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.1, 2.4).
Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.1, 2.4).
 Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
Typical vertebra
 The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
 The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
Cervical vertebrae
 Each transverse process is trough shaped and perforated by a round foramen transversarium.
Each transverse process is trough shaped and perforated by a round foramen transversarium.
 The spinous process is short and bifid.
The spinous process is short and bifid.
 The vertebral foramen is triangular.
The vertebral foramen is triangular.
Atlas and axis
Thoracic vertebrae
Lumbar vertebrae
Sacrum
Coccyx
Intervertebral foramina
 posteriorly by the zygapophysial joint between the articular processes of the two vertebrae, and
posteriorly by the zygapophysial joint between the articular processes of the two vertebrae, and
 anteriorly by the intervertebral disc and adjacent vertebral bodies.
anteriorly by the intervertebral disc and adjacent vertebral bodies.
Posterior spaces between vertebral arches
Curvatures of vertebral column
 The commonest type is spina bifida occulta, in which there is a defect in the vertebral arch of LV or SI. This defect occurs in as many as 10% of individuals and results in failure of the posterior arch to fuse in the midline. Clinically, the patient is asymptomatic, although there may be a tuft of hair over the spinous processes.
The commonest type is spina bifida occulta, in which there is a defect in the vertebral arch of LV or SI. This defect occurs in as many as 10% of individuals and results in failure of the posterior arch to fuse in the midline. Clinically, the patient is asymptomatic, although there may be a tuft of hair over the spinous processes.
JOINTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 PT Case Studies
PT Case Studies Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.
Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.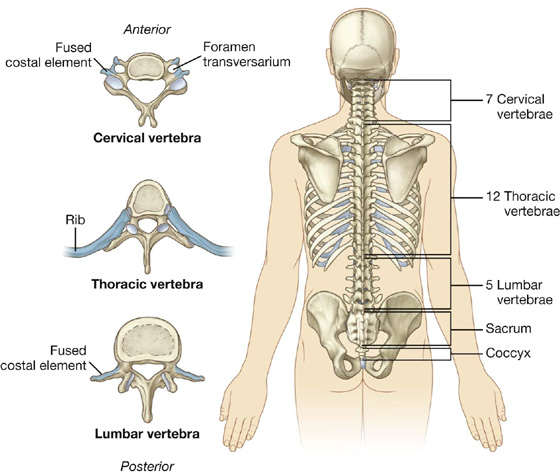

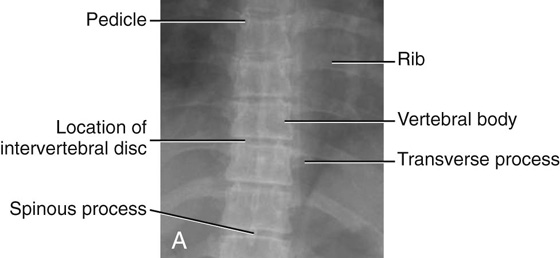
 The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.
The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.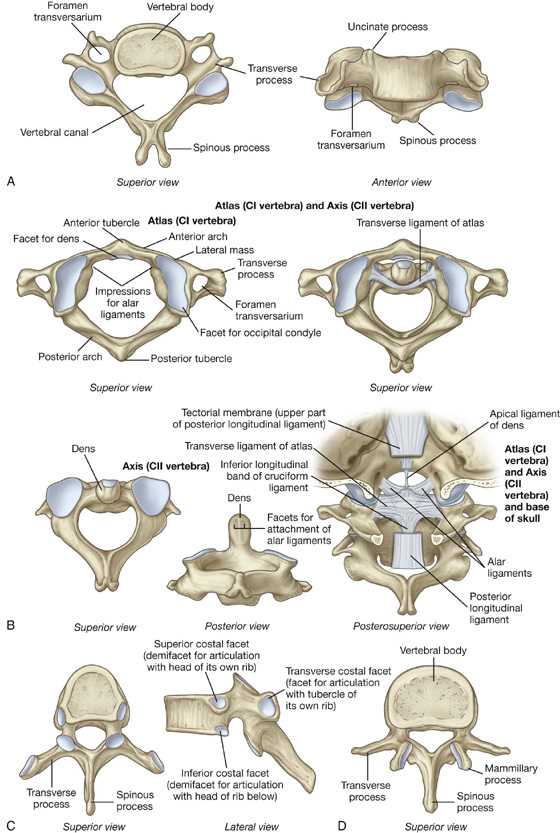
 The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults.
The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults. Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.
Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.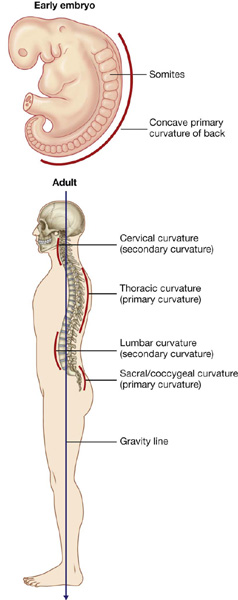
 The more severe form of spina bifida involves complete failure of fusion of the posterior arch at the lumbosacral junction with a large outpouching of the meninges. This may contain cerebrospinal fluid (a meningocele) or a portion of the spinal cord (a myelomeningocele). These abnormalities may result in a variety of neurological deficits, including problems with walking and bladder function.
The more severe form of spina bifida involves complete failure of fusion of the posterior arch at the lumbosacral junction with a large outpouching of the meninges. This may contain cerebrospinal fluid (a meningocele) or a portion of the spinal cord (a myelomeningocele). These abnormalities may result in a variety of neurological deficits, including problems with walking and bladder function.
