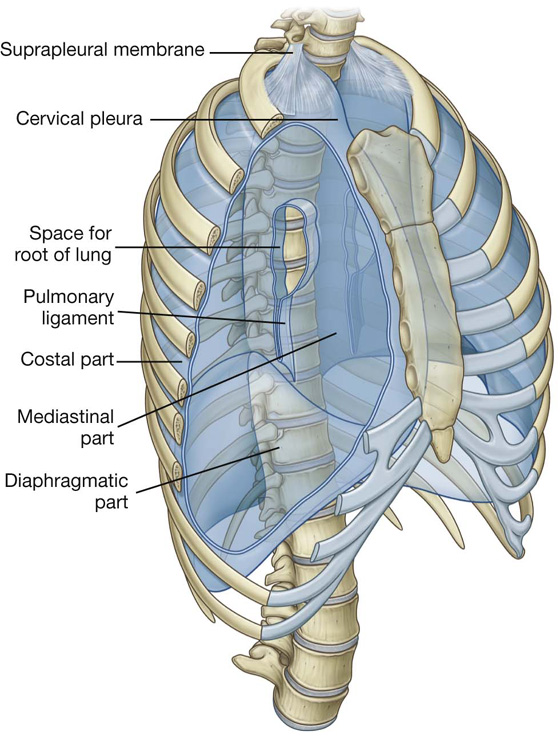
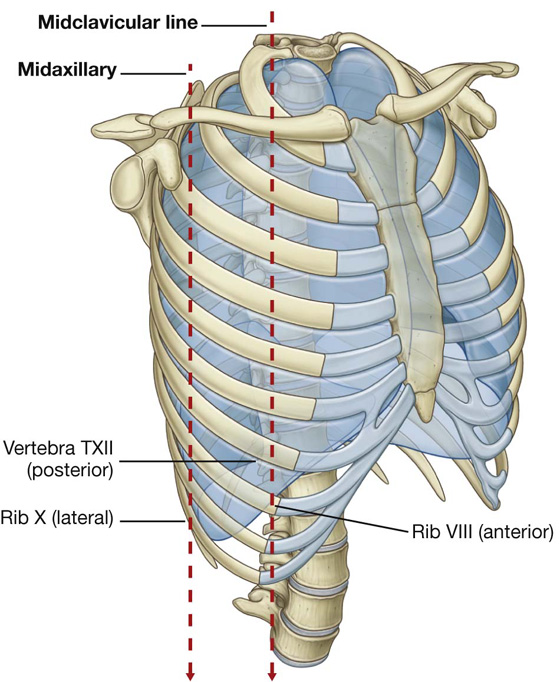
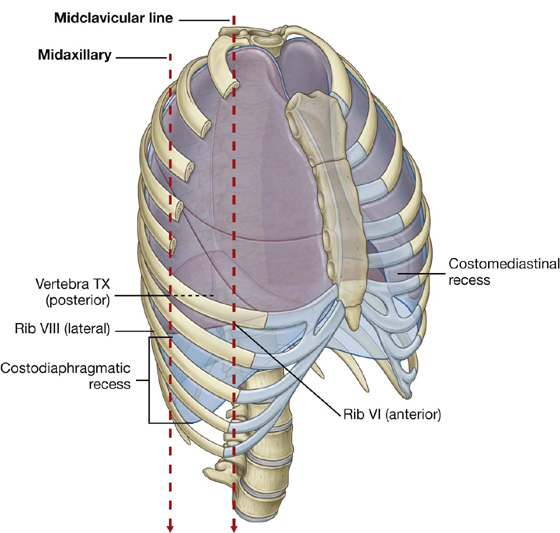
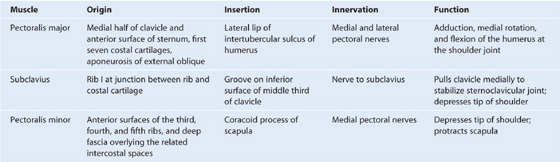
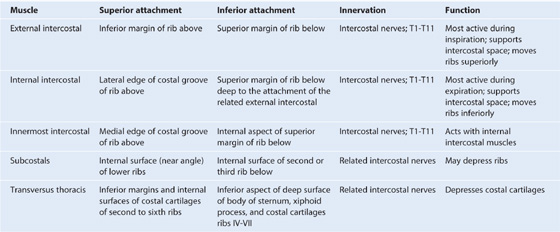
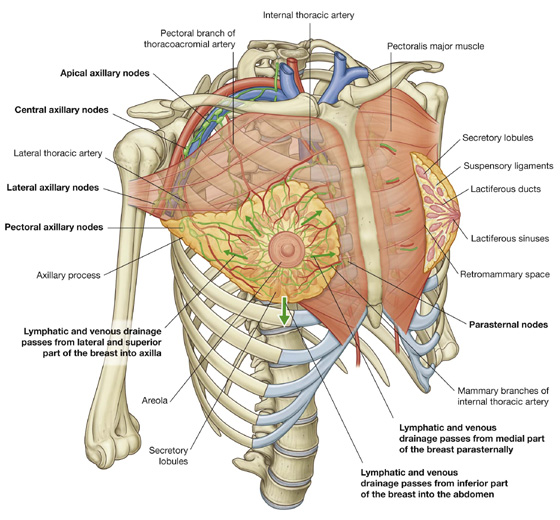
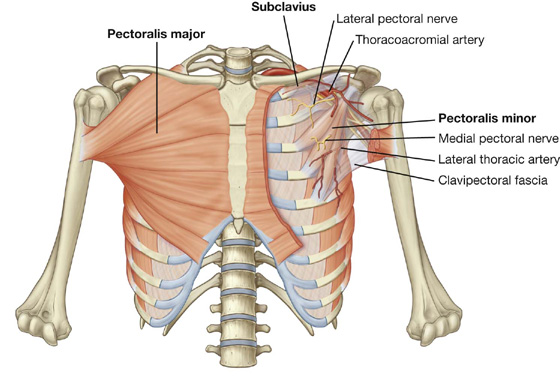
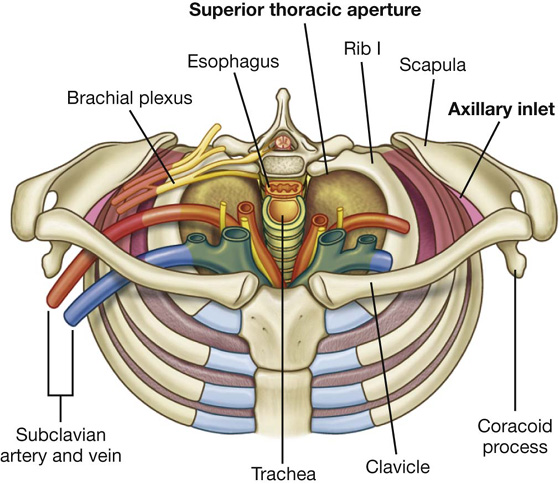
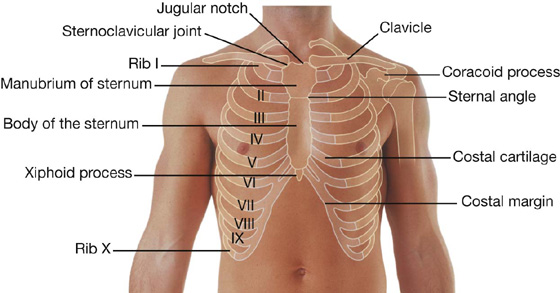
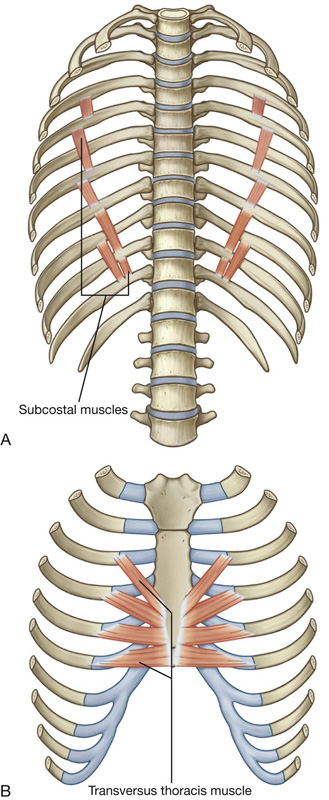
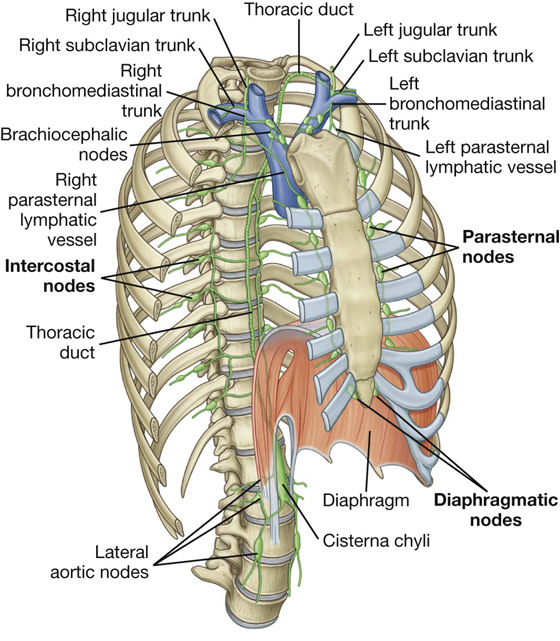
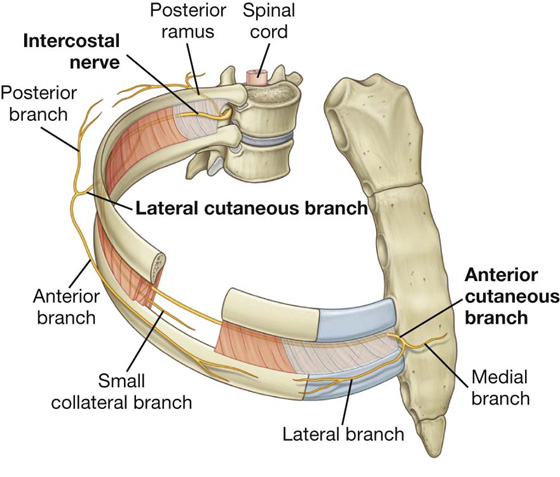
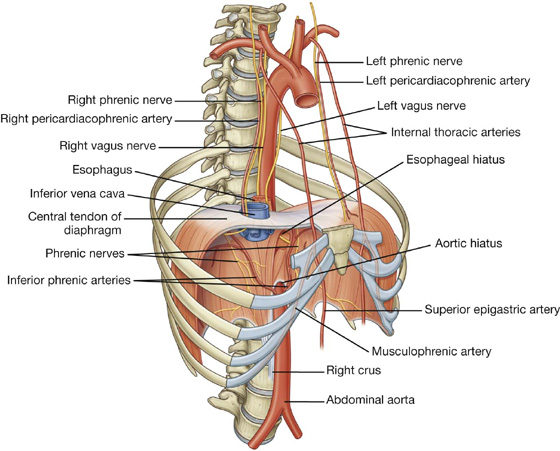
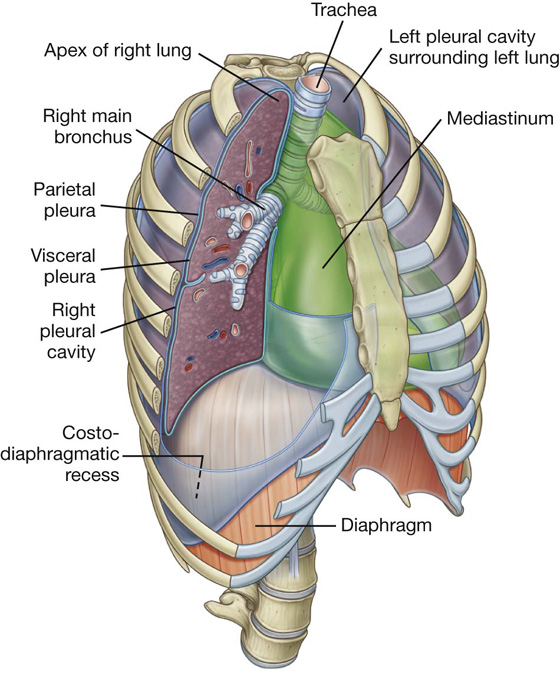
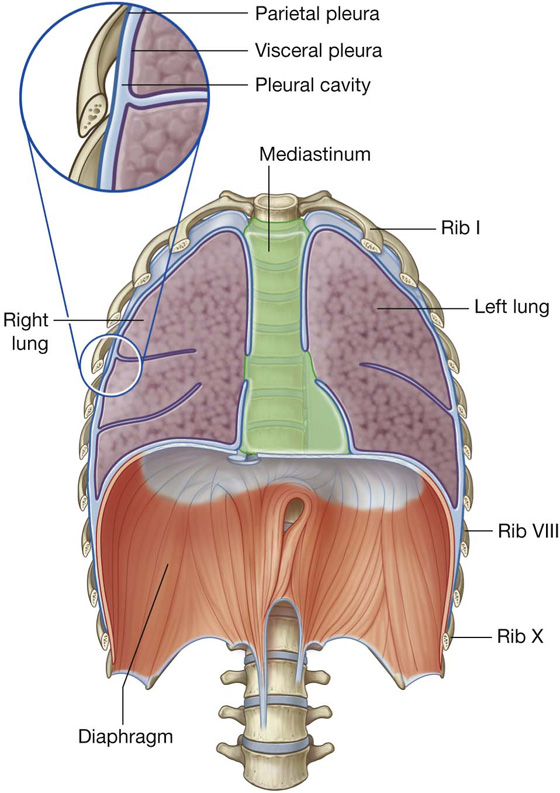
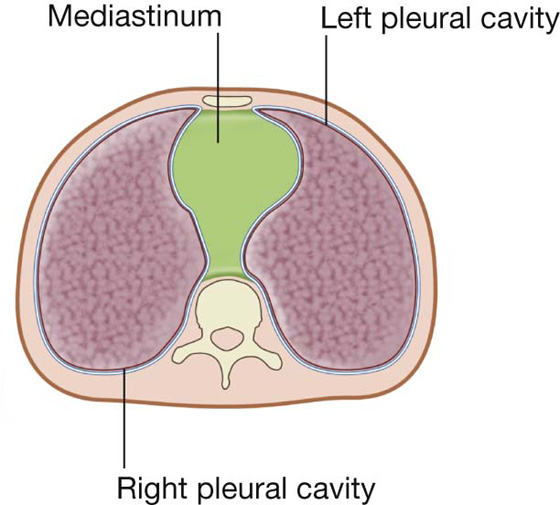
3 Muscles of the pectoral region Movements of the thoracic wall and diaphragm during breathing The thorax is an irregularly shaped cylinder with a narrow opening (superior thoracic aperture) superiorly and a relatively large opening (inferior thoracic aperture) inferiorly (Fig. 3.1). The thorax consists of: Fig. 3.1 Thoracic wall and cavity. The thorax: The thorax also provides support for the upper limb. Muscles anchored to the anterior thoracic wall provide some of this support, and together with their associated connective tissues, nerves, and vessels, and the overlying skin and superficial fascia, define the pectoral region. The pectoral region is external to the anterior thoracic wall and anchors the upper limb to the trunk. It consists of: The breasts consist of mammary glands, associated skin, and connective tissues. The mammary glands are modified sweat glands in the superficial fascia anterior to the pectoral muscles and the anterior thoracic wall (Fig. 3.2). Fig. 3.2 Breasts. The mammary glands consist of ducts and associated secretory lobules. These converge, forming 15 to 20 lactiferous ducts, which open independently onto the nipple. The nipple is surrounded by a circular pigmented area of skin, the areola (Fig. 3.2). A well-developed, connective tissue stroma surrounds the ducts and lobules of the mammary gland. In certain regions, this stroma condenses, forming well-defined ligaments, the suspensory ligaments of breast, which are continuous with the dermis of the skin and support the breast. In nonlactating women, the predominant component of the breasts is fat, whereas glandular tissue is more abundant in lactating women. The breast lies on the deep fascia of the pectoralis major muscle and other surrounding muscles. A layer of loose connective tissue (the retromammary space) separates the breast from the deep fascia and provides some degree of movement over underlying structures. Clinical app Axillary process of breast It is important for clinicians to remember when evaluating the breast for pathology that the upper lateral region of the breast can project around the lateral margin of the pectoralis major muscle and into the axilla. This axillary process (axillary tail) may perforate deep fascia and extend as far superiorly as the apex of the axilla (Fig. 3.2). The breast is related to the thoracic wall and to structures associated with the upper limb; therefore, vascular supply and drainage can occur by multiple routes (Fig. 3.2): Veins draining the breast parallel the arteries and ultimately drain into the axillary, internal thoracic, and intercostal veins. Innervation of the breast is via anterior and lateral cutaneous branches of the second to sixth intercostal nerves. The nipple is innervated by the fourth intercostal nerve. Lymphatic drainage of the breast is as follows: Axillary nodes drain into the subclavian trunks, parasternal nodes drain into the bronchomediastinal trunks, and intercostal nodes drain either into the thoracic duct or into the bronchomediastinal trunks. The breast in men is rudimentary and consists only of small ducts, often composed of cords of cells, which normally do not extend beyond the areola. Breast cancer can occur in men. Clinical app Breast cancer Breast cancer is one of the most common malignancies in women. Breast cancer develops in the cells of the acini, lactiferous ducts, and lobules of the breast. Tumor growth and spread depend on the exact cellular site of origin of the cancer. Breast tumors spread via the lymphatics and veins or by direct invasion. Subcutaneous lymphatic obstruction and tumor growth pull on connective tissue ligaments, the suspensory ligaments, in the breast resulting in the appearance of an orange peel texture (peau d’orange) on the surface of the breast. Further subcutaneous spread can induce a rare manifestation of breast cancer that produces a hard, woody texture to the skin (cancer en cuirasse). Surface anatomy The breast in women Although breasts vary in size, they are normally positioned on the thoracic wall between ribs II and VI and overlie the pectoralis major muscles. Each mammary gland extends superolaterally around the lower margin of the pectoralis major muscle and enters the axilla (Fig. 3.3). This portion of the gland is the axillary tail or axillary process. The positions of the nipple and areola vary relative to the chest wall depending on breast size. Each pectoral region contains the pectoralis major, pectoralis minor, and subclavius muscles (Table 3.1, Fig. 3.4). All originate from the anterior thoracic wall and insert into bones of the upper limb. Table 3.1 Muscles of the pectoral region Fig. 3.4 Muscles and fascia of the pectoral region. A continuous layer of deep fascia, clavipectoral fascia, encloses the subclavius and pectoralis minor and attaches to the clavicle above and to the floor of the axilla below. The muscles of the pectoral region form the anterior wall of the axilla, a region between the upper limb and the neck through which all major structures pass. The thoracic wall consists of skeletal elements and muscles (see Fig. 3.1): The thorax wall extends between: The superior thoracic aperture (Fig. 3.5; also see Fig. 3.1) consists of: Fig. 3.5 Superior thoracic aperture. The superior margin of the manubrium is in approximately the same horizontal plane as the intervertebral disc between vertebrae TII and TIII. The first ribs slope inferiorly from their posterior articulation with vertebra TI to their anterior attachment to the manubrium. Consequently, the plane of the superior thoracic aperture is at an oblique angle, facing somewhat anteriorly (Fig. 3.5). At the superior thoracic aperture, the superior aspects of the pleural cavities, which surround the lungs, lie on either side of the entrance to the mediastinum (Fig. 3.6). Fig. 3.6 Superior thoracic aperture and axillary inlet. Structures that pass between the upper limb and thorax pass over rib I and the superior part of the pleural cavity as they enter and leave the mediastinum (Fig. 3.6). Structures that pass between the neck and head and the thorax pass more vertically through the superior thoracic aperture (Fig. 3.5). The inferior thoracic aperture is large and expandable, and bone, cartilage, and ligaments form its margin (Fig. 3.7). It is closed by the diaphragm (3.7B), and structures passing between the abdomen and thorax pierce or pass posteriorly to this structure. Skeletal elements of the inferior thoracic aperture are: Fig. 3.7 A. Inferior thoracic aperture. B. Diaphragm. Clinical app Thoracic outlet syndrome Clinically, thoracic outlet syndrome is used to describe symptoms resulting from abnormal compression of the brachial plexus of nerves as it passes over the first rib and through the axillary inlet into the upper limb. The anterior ramus of T1 passes superiorly out of the superior thoracic aperture to join and become part of the brachial plexus. A connective tissue band that can extend from the tip of a cervical rib to rib I is one cause of thoracic outlet syndrome by putting upward stresses on the lower parts of the brachial plexus as they pass over the first rib. Joints between the costal margin and sternum lie roughly in the same horizontal plane as the intervertebral disc between vertebrae TIX and TX. Thus, the posterior margin of the inferior thoracic aperture is inferior to the anterior margin. The skeletal elements of the thoracic wall consist of thoracic vertebrae, intervertebral discs, ribs, and sternum. There are 12 thoracic vertebrae, each of which is characterized by articulations with the ribs. A typical thoracic vertebra has a heart-shaped vertebral body, with roughly equal dimensions in the transverse and anteroposterior directions, and a long spinous process (Fig. 3.8). The vertebral foramen is generally circular and the laminae are broad and overlap with those of the vertebra below. The superior articular processes are flat, with their articular surfaces facing almost directly posteriorly, whereas the inferior articular processes project from the laminae and their articular facets face anteriorly. The transverse processes are club shaped and project posterolaterally. Fig. 3.8 Typical thoracic vertebra. A typical thoracic vertebra has three sites for articulations with ribs on each side (Fig. 3.8). Not all vertebrae articulate with ribs in the same fashion (Fig. 3.9): Fig. 3.9 Thoracic vertebrae. There are 12 pairs of ribs, each terminating anteriorly in a costal cartilage (Fig. 3.10). Fig. 3.10 Ribs. Although all ribs articulate with the vertebral column, only the costal cartilages of the upper seven ribs, known as true ribs, articulate directly with the sternum. The remaining five pairs of ribs are false ribs: A typical rib consists of a curved shaft with anterior and posterior ends (Fig. 3.11). The anterior end is continuous with its costal cartilage. The posterior end articulates with the vertebral column and is characterized by a head, neck, and tubercle. Fig. 3.11 A typical rib. A. Anterior view. B. Posterior view of proximal end of rib. The head is somewhat expanded and typically presents two articular surfaces separated by a crest. The smaller superior surface articulates with the inferior costal facet on the body of the vertebra above, whereas the larger inferior facet articulates with the superior costal facet of its own vertebra. The neck is a short flat region of bone that separates the head from the tubercle. The tubercle projects posteriorly from the junction of the neck with the shaft and consists of two regions, an articular part and a nonarticular part: The shaft is generally thin and flat with internal and external surfaces. The superior margin is smooth and rounded, whereas the inferior margin is sharp. The shaft bends forward just laterally to the tubercle at a site termed the angle. It also has a gentle twist around its longitudinal axis so that the external surface of the anterior part of the shaft faces somewhat superiorly relative to the posterior part. The inferior margin of the internal surface is marked by a distinct costal groove. The upper and lower ribs have distinct features (Fig. 3.12). Fig. 3.12 Atypical ribs. Rib I is flat in the horizontal plane and has broad superior and inferior surfaces. From its articulation with vertebra TI, it slopes inferiorly to its attachment to the manubrium of sternum. The head articulates with the body of vertebra TI and has only one articular surface. The tubercle has a facet for articulation with the transverse process. The superior surface of the rib is characterized by a distinct tubercle, the scalene tubercle, which separates two smooth grooves that cross the rib approximately midway along the shaft. The anterior groove is caused by the subclavian vein, and the posterior groove is caused by the subclavian artery. Anterior and posterior to these grooves, the shaft is roughened by muscle and ligament attachments. Rib II, like rib I, is flat but twice as long. It articulates with the vertebral column in a way typical of most ribs. The head of rib X has a single facet for articulation with its own vertebra. Ribs XI and XII articulate only with the bodies of their own vertebrae and have no tubercles or necks. Both ribs are short, have little curve, and are pointed anteriorly. Clinical apps Cervical ribs Cervical ribs are present in approximately 1% of the population. A cervical rib is an accessory rib articulating with vertebra CVII; the anterior end attaches to the superior border of the anterior aspect of rib I. Plain radiographs may demonstrate cervical ribs as small hornlike structures. It is often not appreciated by clinicians that a fibrous band commonly extends from the anterior tip of the small cervical ribs to rib I, producing a “cervical band” that is not visualized on radiography. In patients with cervical ribs and cervical bands, structures that normally pass over rib I are elevated by, and pass over, the cervical rib and band. Clinical apps Rib fractures Single rib fractures are of little consequence, though extremely painful. After severe trauma, ribs may be broken in two or more places. If enough ribs are broken, a loose segment of chest wall, a flail segment (flail chest), is produced. When the patient takes a deep inspiration, the flail segment moves in the opposite direction to the chest wall, preventing full lung expansion and creating a paradoxically moving segment. If a large enough segment of chest wall is affected, ventilation may be impaired and assisted ventilation may be required until the ribs have healed. The adult sternum consists of three major elements: the broad and superiorly positioned manubrium of sternum, the narrow and longitudinally oriented body of sternum, and the small and inferiorly positioned xiphoid process (Fig. 3.13). Fig. 3.13 Sternum. The manubrium of sternum forms part of the bony framework of the neck and the thorax. The superior surface of the manubrium is expanded laterally and bears a distinct and palpable notch, the jugular notch (suprasternal notch), in the midline (Fig. 3.13). On either side of this notch is a large oval fossa for articulation with the clavicle. Immediately inferior to this fossa, on each lateral surface of the manubrium, is a facet for the attachment of the first costal cartilage. At the lower end of the lateral border is a demifacet for articulation with the upper half of the anterior end of the second costal cartilage. The body of the sternum is flat (Fig. 3.13). The anterior surface of the body of the sternum is often marked by transverse ridges that represent lines of fusion between the segmental elements called sternebrae, from which this part of the sternum arises embryologically. The lateral margins of the body of the sternum have articular facets for costal cartilages. Superiorly, each lateral margin has a demifacet for articulation with the inferior aspect of the second costal cartilage. Inferior to this demifacet are four facets for articulation with the costal cartilages of ribs III to VI. At the inferior end of the body of the sternum is a demifacet for articulation with the upper demifacet on the seventh costal cartilage. The inferior end of the body of the sternum is attached to the xiphoid process. The xiphoid process is the smallest part of the sternum (Fig. 3.13). Its shape is variable: it may be wide, thin, pointed, bifid, curved, or perforated. It begins as a cartilaginous structure, which becomes ossified in the adult. On each side of its upper lateral margin is a demifacet for articulation with the inferior end of the seventh costal cartilage. Collection of sternal bone marrow The subcutaneous position of the sternum makes it possible to place a needle through the hard outer cortex into the internal (or medullary) cavity containing bone marrow. Once the needle is in this position, bone marrow can be aspirated. Evaluation of this material under the microscope helps clinicians diagnose certain blood diseases such as leukemia. A typical rib articulates with: Fig. 3.14 Costovertebral joints. Together, the costovertebral joints and related ligaments allow the necks of the ribs either to rotate around their longitudinal axes, which occurs mainly in the upper ribs, or to ascend and descend relative to the vertebral column, which occurs mainly in the lower ribs. The combined movements of all of the ribs on the vertebral column are essential for altering the volume of the thoracic cavity during breathing. The two facets on the head of the rib articulate with the superior facet on the body of its own vertebra and with the inferior facet on the body of the vertebra above (Fig. 3.14). This joint is divided into two synovial compartments by an intra-articular ligament, which attaches the crest to the adjacent intervertebral disc and separates the two articular surfaces on the head of the rib. The two synovial compartments and the intervening ligament are surrounded by a single joint capsule attached to the outer margins of the combined articular surfaces of the head and vertebral column. Costotransverse joints are synovial joints between the tubercle of a rib and the transverse process of the related vertebra (Fig. 3.14). The joint is stabilized by two strong extracapsular ligaments that span the space between the transverse process and the rib on the medial and lateral sides of the joint: A third ligament, the superior costotransverse ligament, attaches the superior surface of the neck of the rib to the transverse process of the vertebra above. Slight gliding movements occur at the costotransverse joints. The sternocostal joints are joints between the upper seven costal cartilages and the sternum (Fig. 3.15). Fig. 3.15 Sternocostal joints. The joint between rib I and the manubrium is not synovial and consists of a fibrocartilaginous connection between the manubrium and the costal cartilage. The joints between rib II through VII and the sternum are synovial and have thin capsules reinforced by surrounding sternocostal ligaments. Interchondral joints occur between the costal cartilages of adjacent ribs (Fig. 3.15), mainly between the costal cartilages of ribs VII to X, but may also involve the costal cartilages of ribs V and VI. Interchondral joints provide indirect anchorage to the sternum and contribute to the formation of a smooth inferior costal margin. They are usually synovial, and the thin fibrous capsules are reinforced by interchondral ligaments. The joints between the manubrium and body of sternum and between the body of sternum and the xiphoid process are usually symphyses (Fig. 3.15). Only slight angular movements occur between the manubrium and body of sternum during respiration. The joint between the body of sternum and the xiphoid process often becomes ossified with age. Additionally, the sternal angle is on a horizontal plane that passes through the intervertebral disc between vertebrae TIV and TV (Fig. 3.16). This plane separates the superior mediastinum from the inferior mediastinum and marks the superior border of the pericardium. It also separates the end of the ascending aorta from the beginning of the arch of the aorta, the end of the arch of the aorta from the beginning of the thoracic aorta, and passes through the bifurcation of the trachea just superior to the pulmonary trunk. Fig. 3.16 Vertebral level TIV/V. Clinical app The manubriosternal joint as reference A clinically useful feature of the manubriosternal joint is that it can be palpated easily. This is because the manubrium normally angles posteriorly on the body of sternum, forming a raised feature referred to as the sternal angle. This elevation marks the site of articulation of rib II with the sternum. Rib I is not palpable because it lies inferior to the clavicle and is embedded in tissues at the base of the neck. Therefore, rib II is used as a reference for counting ribs and can be felt immediately lateral to the sternal angle. How to count ribs Knowing how to count ribs is important because different ribs provide palpable landmarks for the positions of deeper structures. To determine the location of specific ribs, palpate the jugular notch at the superior extent of the manubrium of the sternum. Move down the sternum until a ridge is felt. This ridge is the sternal angle, which identifies the articulation between the manubrium of sternum and the body of sternum. The costal cartilage of rib II articulates with the sternum at this location. Identify rib II. Then continue counting the ribs, moving in a downward and lateral direction (Fig. 3.17). Surface anatomy Visualizing structures at the TIV/V vertebral level The TIV/V vertebral level is a transverse plane that passes through the sternal angle on the anterior chest wall and the intervertebral disc between TIV and TV vertebrae posteriorly. This plane can easily be located, because the joint between the manubrium of sternum and the body of sternum forms a distinct bony protuberance that can be palpated. At the TIV/V level (Fig. 3.18): Intercostal spaces lie between adjacent ribs and are filled by intercostal muscles (Fig. 3.19). Fig. 3.19 Intercostal space. A. Anterolateral view. B. Details of an intercostal space and relationships. Intercostal nerves and associated major arteries and veins lie in the costal groove along the inferior margin of the superior rib and pass in the plane between the inner two layers of muscles (Fig. 3.19). In each space, the vein is the most superior structure and is therefore highest in the costal groove. The artery is inferior to the vein, and the nerve is inferior to the artery and often not protected by the groove. Therefore, the nerve is the structure most at risk when objects perforate the upper aspect of an intercostal space. Deep to the intercostal spaces and ribs, and separating these structures from the underlying pleura, is a layer of loose connective tissue called endothoracic fascia, which contains variable amounts of fat (Fig. 3.19B). Muscles of the thoracic wall include those that fill and support the intercostal spaces (external, internal, and innermost intercostal muscles [Table 3.2, Figs. 3.19, 3.20]); those that cross several ribs between the costal attachments (subcostal muscles [Table 3.2, Fig. 3.21A]); and those that pass between the sternum and the ribs (transversus thoracis muscles [Table 3.2, Fig. 3.21B]). Table 3.2 Muscles of the thoracic wall Fig. 3.20 Intercostal muscles. Fig. 3.21 A. Subcostal muscles. B. Transversus thoracis muscles. The muscles of the thoracic wall, together with muscles between the vertebrae and ribs posteriorly (i.e., the levatores costarum, and serratus posterior superior and serratus posterior inferior muscles), alter the position of the ribs and sternum changing the thoracic volume during breathing. They also reinforce the thoracic wall. The intercostal muscles are three flat muscles found in each intercostal space that pass between adjacent ribs (Figs. 3.19B, 3.20). Individual muscles in this group are named according to their positions: The intercostal muscles are innervated by the related intercostal nerves. As a group, the intercostal muscles provide structural support for the intercostal spaces during breathing. They can also move the ribs. Vessels that supply the thoracic wall consist mainly of posterior and anterior intercostal arteries, which pass around the wall between adjacent ribs in intercostal spaces (Fig. 3.19A). These arteries originate from the aorta and internal thoracic arteries, which in turn arise from the subclavian arteries in the root of the neck. Together, the intercostal arteries form a basket-like pattern of vascular supply around the thoracic wall. Posterior intercostal arteries originate from vessels associated with the posterior thoracic wall. The upper two posterior intercostal arteries on each side come from the supreme intercostal artery, which descends into the thorax as a branch of the costocervical trunk in the neck. The costocervical trunk is a posterior branch of the subclavian artery (Fig. 3.22). Fig. 3.22 Arteries of the thoracic wall. The remaining nine pairs of posterior intercostal arteries arise from the posterior surface of the thoracic aorta. Because the aorta is on the left side of the vertebral column, those posterior intercostal vessels passing to the right side of the thoracic wall cross the midline anterior to the bodies of the vertebrae and therefore are longer than the corresponding vessels on the left. In addition to having numerous branches that supply various components of the wall, the posterior intercostal arteries have branches that accompany lateral cutaneous branches of the intercostal nerves to the superficial regions. The anterior intercostal arteries originate directly or indirectly as lateral branches from the internal thoracic arteries (Fig. 3.22). Each internal thoracic artery arises as a major branch of the subclavian artery in the neck. It passes anteriorly over the cervical dome of pleura and descends vertically through the superior thoracic aperture and along the deep aspect of the anterior thoracic wall. On each side, the internal thoracic artery lies posterior to the costal cartilages of the upper six ribs and about 1 cm lateral to the sternum. At approximately the level of the sixth intercostal space, it divides into two terminal branches (Fig. 3.22): Anterior intercostal arteries that supply the upper six intercostal spaces arise as lateral branches from the internal thoracic artery, whereas those supplying the lower spaces arise from the musculophrenic artery. In each intercostal space, the anterior intercostal arteries usually have two branches: In addition to anterior intercostal arteries and a number of other branches, the internal thoracic arteries give rise to perforating branches that pass directly forward between the costal cartilages to supply structures external to the thoracic wall. These vessels travel with the anterior cutaneous branches of the intercostal nerves. Venous drainage from the thoracic wall generally parallels the pattern of arterial supply (Fig. 3.23). Fig. 3.23 Veins of the thoracic wall. Centrally, the intercostal veins ultimately drain into the azygos system of veins or into internal thoracic veins, which connect with the brachiocephalic veins in the neck. Often the upper posterior intercostal veins on the left side come together and form the left superior intercostal vein, which empties into the left brachiocephalic vein. Similarly, the upper posterior intercostal veins on the right side may come together and form the right superior intercostal vein, which empties into the azygos vein. Lymphatic vessels of the thoracic wall drain mainly into lymph nodes associated with the internal thoracic arteries (parasternal nodes), with the heads and necks of ribs (intercostal nodes), and with the diaphragm (diaphragmatic nodes) (Fig. 3.24). Diaphragmatic nodes are posterior to the xiphoid and at sites where the phrenic nerves penetrate the diaphragm. They also occur in regions where the diaphragm is attached to the vertebral column. Fig. 3.24 Major lymphatic vessels and nodes of the thoracic wall. Parasternal nodes drain into bronchomediastinal trunks. Intercostal nodes in the upper thorax also drain into bronchomediastinal trunks, whereas intercostal nodes in the lower thorax drain into the thoracic duct. Nodes associated with the diaphragm interconnect with parasternal, prevertebral, juxtaesophageal nodes, brachiocephalic (anterior to the brachiocephalic veins in the superior mediastinum), and lateral aortic/lumbar nodes (in the abdomen). Superficial regions of the thoracic wall drain mainly into axillary lymph nodes in the axilla or parasternal nodes. Innervation of the thoracic wall is mainly by the intercostal nerves, which are the anterior rami of spinal nerves T1 to T11 and lie in the intercostal spaces between adjacent ribs. The anterior ramus of spinal nerve T12 (the subcostal nerve) is inferior to rib XII (Fig. 3.25). Fig. 3.25 Intercostal nerves. A typical intercostal nerve passes laterally around the thoracic wall in an intercostal space. The largest of the branches is the lateral cutaneous branch, which pierces the lateral thoracic wall and divides into an anterior branch and a posterior branch that innervate the overlying skin. The intercostal nerves end as anterior cutaneous branches, which emerge either parasternally, between adjacent costal cartilages, or laterally to the midline, on the anterior abdominal wall, to supply the skin. In addition to these major branches, small collateral branches can be found in the intercostal space running along the superior border of the lower rib. In the thorax, the intercostal nerves carry: Sensory innervation from the skin overlying the upper thoracic wall is supplied by cutaneous branches (supraclavicular nerves), which descend from the cervical plexus in the neck. In addition to innervating the thoracic wall, intercostal nerves innervate other regions: Clinical app Surgical access to the chest Surgical access is challenging in the chest given the rigid nature of the thoracic cage. Moreover, the access site is also dependent on the organ that is operated upon and its relationships to subdiaphragmatic structures and structures in the neck. Minimally invasive thoracic surgery (video-assisted thoracic surgery [VATS]) involves making small (1 cm) incisions in the intercostal spaces, inserting a small camera, and manipulating other instruments through additional small incisions. A number of procedures can be performed in this manner, including lobectomy, lung biopsy, and esophagectomy. A standard incision site would include a median sternotomy to obtain access to the heart, including the coronary arteries and the cardiac valves. A left lateral thoracotomy or a right lateral thoracotomy is an incision through an intercostal space to access the lungs and the more lateral mediastinal structures. Thoracostomy (chest) tube insertion Insertion of a chest tube is a commonly performed procedure and is indicated to relieve air or fluid trapped in the thorax between the lung and the chest wall (pleural cavity). This procedure is done for pneumothorax, hemothorax, hemopneumothorax, malignant pleural effusion empyema, hydrothorax, chylothorax, and also after thoracic surgery. The position of the thoracostomy tube should be between the anterior axillary and midaxillary anatomical lines from anterior to posterior and either the fourth or fifth intercostal space from cephalad to caudad. The position of the ribs in this region should be clearly marked. Anesthetic should be applied to the superior border of the rib and the inferior aspect of the intercostal space, including one rib and space above and one rib and space below. The neurovascular bundle runs in the neurovascular plane, which lies in the superior aspect of the intercostal space (just below the rib), hence the reason for positioning the tube on the superior border of a rib (i.e., at the lowest position in the intercostal space). Clinical app Intercostal nerve block Local anesthesia of intercostal nerves produces excellent analgesia in patients with chest trauma and those patients requiring anesthesia for a thoracotomy, mastectomy, and upper abdominal surgical procedures. The intercostal nerves are situated inferior to the rib borders in the neurovascular bundle. Each neurovascular bundle is situated deep to the external and internal intercostal muscle groups. The nerve block may be undertaken using a “blind” technique or under direct imaging guidance. The patient is placed in the appropriate position to access the rib. Typically, under ultrasound guidance, a needle may be advanced into the region of the subcostal groove followed by an injection with local anesthesia. Depending on the type of local anesthetic, analgesia may be short- or long-acting. Given the position of the neurovascular bundle and the subcostal groove, complications may include puncture of the parietal pleura and an ensuing pneumothorax. Bleeding may also occur if the artery or vein is damaged during the procedure. The diaphragm is a thin musculotendinous structure that fills the inferior thoracic aperture and separates the thoracic cavity from the abdominal cavity (Figs. 3.26, 3.27, and see Chapter 4). It is attached peripherally to the: Fig. 3.26 Major structures passing between abdomen and thorax. Fig. 3.27 Diaphragm. From these peripheral attachments, muscle fibers converge to join the central tendon. The pericardium is attached to the middle part of the central tendon. In the median sagittal plane, the diaphragm slopes inferiorly from its anterior attachment to the xiphoid, approximately at vertebral level TVIII/IX, to its posterior attachment to the median arcuate ligament, crossing anteriorly to the aorta at approximately vertebral level TXII. Structures traveling between the thorax and abdomen pass through the diaphragm or between the diaphragm and its peripheral attachments (Figs. 3.26, 3.27): Other structures outside the posterior attachments of the diaphragm lateral to the aortic hiatus include the sympathetic trunks and the least splanchnic nerves. The greater and lesser splanchnic nerves penetrate the crura. The arterial supply to the diaphragm is from vessels that arise superiorly and inferiorly to it (see Fig. 3.27). From above, pericardiacophrenic and musculophrenic arteries supply the diaphragm. These vessels are branches of the internal thoracic arteries. Superior phrenic arteries, which arise directly from lower parts of the thoracic aorta, and small branches from intercostal arteries contribute to the supply. The largest arteries supplying the diaphragm arise from below it. These arteries are the inferior phrenic arteries, which branch directly from the abdominal aorta. Venous drainage of the diaphragm is by veins that generally parallel the arteries. The veins drain into: The diaphragm is innervated by the phrenic nerves (C3, C4, and C5), which penetrate the diaphragm and innervate it from its abdominal surface (Fig. 3.27). Contraction of the domes of the diaphragm flattens the diaphragm, increasing thoracic volume. Movements of the diaphragm are essential for normal breathing. During breathing, the dimensions of the thorax change in the vertical, lateral, and anteroposterior directions. Elevation and depression of the diaphragm significantly alter the vertical dimensions of the thorax. Depression results when the muscle fibers of the diaphragm contract. Elevation occurs when the diaphragm relaxes. Changes in the anteroposterior and lateral dimensions result from elevation and depression of the ribs (Fig. 3.28). The posterior ends of the ribs articulate with the vertebral column, whereas the anterior ends of most ribs articulate with the sternum or adjacent ribs. Because the anterior ends of the ribs are inferior to the posterior ends, when the ribs are elevated, they move the sternum upward and forward. Also, the angle between the body of the sternum and the manubrium may become slightly less acute. When the ribs are depressed, the sternum moves downward and backward. This “pump handle” movement changes the dimensions of the thorax in the anteroposterior direction (Fig. 3.28A). As well as the anterior ends of the ribs being lower than the posterior ends, the middles of the shafts tend to be lower than the two ends. When the shafts are elevated, the middles of the shafts move laterally. This “bucket handle” movement increases the lateral dimensions of the thorax (Fig. 3.28B). Two pleural cavities, one on either side of the mediastinum, surround the lungs (Figs. 3.29, 3.30): Fig. 3.29 Pleural cavities. Fig. 3.30 Pleural cavities. Fig. 3.31 Cross-section of the thorax showing the position of the mediastinum. Clinical app The arrangement of pleural cavities is clinically significant The pleural cavities are completely separated from each other by the mediastinum. Therefore, abnormal events in one pleural cavity do not necessarily affect the other cavity. This also means that the mediastinum can be entered surgically without opening the pleural cavities. Another important feature of the pleural cavities is that they extend above the level of rib I. The apex of each lung actually extends into the root of the neck. As a consequence, abnormal events in the root of the neck can involve the adjacent pleura and lung, and events in the adjacent pleura and lung can involve the root of the neck. Each pleural cavity is lined by a single layer of flat cells, mesothelium, and an associated layer of supporting connective tissue; together, they form the pleura. The pleura is divided into two major types, based on location: The names given to the parietal pleura correspond to the parts of the wall with which they are associated (Fig. 3.32): Fig. 3.32 Parietal pleura. Covering the superior surface of the cervical pleura is a distinct domelike layer of fascia, the suprapleural membrane (Fig. 3.32). This connective tissue membrane is attached laterally to the medial margin of the first rib and behind to the transverse process of vertebra CVII. Superiorly, the membrane receives muscle fibers from some of the deep muscles in the neck (scalene muscles) that function to keep the membrane taught. The suprapleural membrane provides apical support for the pleural cavity in the root of the neck. In the region of vertebrae TV to TVII, the mediastinal pleura reflects off the mediastinum as a tubular, sleevelike covering for structures (i.e., airway, vessels, nerves, lymphatics) that pass between the lung and mediastinum. This sleevelike covering, and the structures it contains, forms the root of the lung. The root joins the medial surface of the lung at an area referred to as the hilum of lung. Here, the mediastinal pleura is continuous with the visceral pleura. Clinical app Innervation of parietal and visceral pleura The parietal pleural is innervated by somatic afferent fibers. The costal pleura is innervated by branches from the intercostal nerves and pain would be felt in relation to the thoracic wall. The diaphragmatic pleura and the mediastinal pleura are innervated mainly by the phrenic nerves (originating at spinal cord levels C3, C4, and C5). Pain from these areas would refer to the C3, C4, and C5 dermatomes (lateral neck and the supraclavicular region of the shoulder). The visceral pleural is innervated by visceral afferent fibers that accompany bronchial vessels and pain is generally not elicited from this tissue. The peripheral reflections of parietal pleura mark the extent of the pleural cavities (Fig. 3.33). Fig. 3.33 Pleural reflections. Superiorly, the pleural cavity can project as much as 3 to 4 cm above the first costal cartilage, but does not extend above the neck of rib I. This limitation is caused by the inferior slope of rib I to its articulation with the manubrium. Anteriorly, the pleural cavities approach each other posterior to the upper part of the sternum. However, posterior to the lower part of the sternum, the parietal pleura does not come as close to the midline on the left side as it does on the right because the middle mediastinum, containing the pericardium and heart, bulges to the left. Inferiorly, the costal pleura reflects onto the diaphragm above the costal margin. In the midclavicular line, the pleural cavity extends inferiorly to approximately rib VIII (Fig. 3.34). In the midaxillary line, it extends to rib X. From this point, the inferior margin courses somewhat horizontally, crossing ribs XI and XII to reach vertebra TXII. From the midclavicular line to the vertebral column, the inferior boundary of the pleura can be approximated by a line that runs between the rib VIII, rib X, and vertebra TXII. Fig. 3.34 Parietal pleural reflections and recesses. The visceral pleura is continuous with the parietal pleura at the hilum of each lung where structures enter and leave the organ. The visceral pleura is firmly attached to the surface of the lung, including both opposed surfaces of the fissures that divide the lungs into lobes. Anteriorly, a costomediastinal recess occurs on each side where the costal pleura is opposed to the mediastinal pleura. The largest is on the left side in the region overlying the heart (Fig. 3.34). The largest and clinically most important recesses are the costodiaphragmatic recesses, which occur in each pleural cavity between the costal pleura and diaphragmatic pleura (Fig. 3.34). The costodiaphragmatic recesses are the regions between the inferior margin of the lungs and inferior margin of the pleural cavities. They are deepest after forced expiration and shallowest after forced inspiration. During quiet respiration, the inferior margin of the lung crosses rib VI in the midclavicular line, rib VIII in the midaxillary line, and then courses somewhat horizontally to reach the vertebral column at vertebral level TX. From the midclavicular line and around the thoracic wall to the vertebral column, the inferior margin of the lung can be approximated by a line running between rib VI, rib VIII, and vertebra TX. The inferior margin of the pleural cavity at the same points is rib VIII, rib X, and vertebra TXII. The costodiaphragmatic recess is the region between the two margins. During expiration, the inferior margin of the lung rises and the costodiaphragmatic recess becomes larger. Clinical app Pleural recesses The lungs do not completely fill the anterior or posterior inferior regions of the pleural cavities (Fig. 3.34). This results in recesses in which two layers of parietal pleura become opposed. Expansion of the lungs into these spaces usually occurs only during forced inspiration; the recesses also provide potential spaces in which fluids can collect and from which fluids can be aspirated. Pleural effusion A pleural effusion occurs when excess fluid accumulates within the pleural space. As the fluid accumulates within the pleural space the underlying lung is compromised and may collapse as the volume of fluid increases. Once a pleural effusion has been diagnosed, fluid often will be aspirated to determine the cause, which can include infection, malignancy, cardiac failure, hepatic disease, and pulmonary embolism. Clinical app Pneumothorax A pneumothorax is a collection of gas or air within the pleural cavity. When air enters the pleural cavity the tissue elasticity of the parenchyma causes the lung to collapse within the chest impairing the lung function. Occasionally, the gas within the pleural cavity may accumulate to such an extent that the mediastinum is “pushed” to the opposite side, compromising the other lung. This is termed a tension pneumothorax and requires urgent treatment. Most pneumothoraces are spontaneous (i.e., they occur in the absence of no known pathology and no known lung disease.) Secondly, pneumothoraces may occur as a result of trauma, inflammation, smoking, and other underlying pulmonary diseases. The symptoms of pneumothorax are often determined by the degree of air leak and the rate at which the accumulation of gas occurs and the ensuing lung collapse. They include pain, shortness of breath, and cardiorespiratory collapse if severe. The two lungs are organs of respiration and lie on either side of the mediastinum surrounded by the right and left pleural cavities. Air enters and leaves the lungs via the main bronchi, which are branches of the trachea. The pulmonary arteries deliver deoxygenated blood to the lungs from the right ventricle of the heart. Oxygenated blood returns to the left atrium via the pulmonary veins. The right lung is normally a little larger than the left lung because the middle mediastinum, containing the heart, bulges more to the left than to the right.
Thorax
 Image Library—illustrations of thoracic anatomy, Chapter 3
Image Library—illustrations of thoracic anatomy, Chapter 3
 Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 3
Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 3
 Short Questions (not scored)—National Board style multiple-choice questions, Chapter 3
Short Questions (not scored)—National Board style multiple-choice questions, Chapter 3
 Interactive Surface Anatomy—interactive surface animations, Chapter 3
Interactive Surface Anatomy—interactive surface animations, Chapter 3
Regional anatomy
 houses and protects the heart, lungs, and great vessels,
houses and protects the heart, lungs, and great vessels,
 acts as a conduit for structures passing between the neck and the abdomen,
acts as a conduit for structures passing between the neck and the abdomen,
 plays a principal role in breathing, and
plays a principal role in breathing, and
 provides support for the upper limbs.
provides support for the upper limbs.
PECTORAL REGION
 a superficial compartment containing skin, superficial fascia, and breasts; and
a superficial compartment containing skin, superficial fascia, and breasts; and
 a deep compartment containing muscles and associated structures.
a deep compartment containing muscles and associated structures.
Breast
Arterial supply
 medially, branches from the internal thoracic artery; and
medially, branches from the internal thoracic artery; and
Venous drainage
Innervation
Lymphatic drainage
 Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (see Fig. 3.2).
Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (see Fig. 3.2).
Breast in men
Muscles of the pectoral region
THORACIC WALL
 Posteriorly, it is made up of 12 thoracic vertebrae and their intervening intervertebral discs.
Posteriorly, it is made up of 12 thoracic vertebrae and their intervening intervertebral discs.
 the superior thoracic aperture bordered by vertebra TI, rib I, and the manubrium of sternum; and
the superior thoracic aperture bordered by vertebra TI, rib I, and the manubrium of sternum; and
Superior thoracic aperture
 the body of vertebra TI posteriorly,
the body of vertebra TI posteriorly,
 the medial margin of rib I on each side, and
the medial margin of rib I on each side, and
Inferior thoracic aperture
 the body of vertebra TXII posteriorly,
the body of vertebra TXII posteriorly,
 rib XII and the distal end of rib XI posterolaterally,
rib XII and the distal end of rib XI posterolaterally,
 the xiphoid process anteriorly.
the xiphoid process anteriorly.
Skeletal framework
Thoracic vertebrae
A typical thoracic vertebra
Articulation with ribs
Ribs
 The raised nonarticular part is roughened by ligament attachments.
The raised nonarticular part is roughened by ligament attachments.
Distinct features of upper and lower ribs
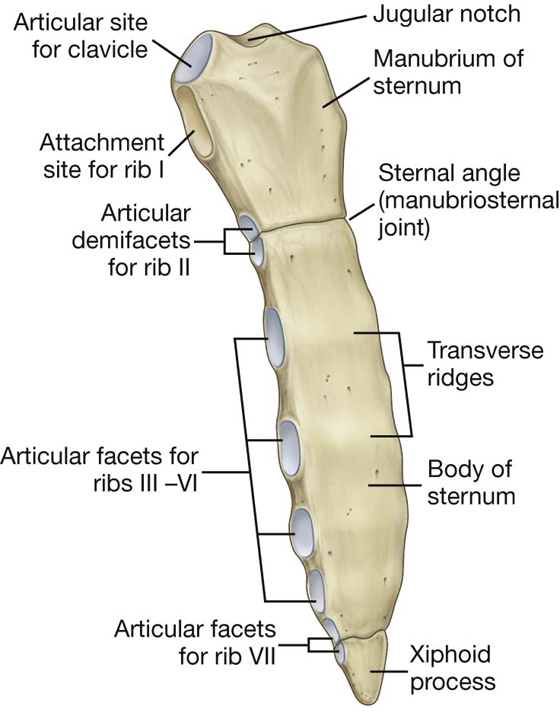
Sternum
Manubrium of sternum
Body of the sternum
Xiphoid process
Joints
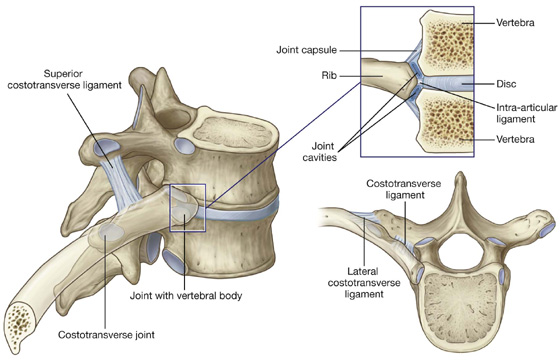
Costovertebral joints
 the bodies of adjacent vertebrae, forming a joint with the head of the rib; and
the bodies of adjacent vertebrae, forming a joint with the head of the rib; and
 the transverse process of its related vertebra, forming a costotransverse joint (Fig. 3.14).
the transverse process of its related vertebra, forming a costotransverse joint (Fig. 3.14).
Sternocostal joints
Interchondral joints
Manubriosternal and xiphisternal joints
 The costal cartilage of rib II articulates with the sternum.
The costal cartilage of rib II articulates with the sternum.
 The superior mediastinum is separated from the inferior mediastinum.
The superior mediastinum is separated from the inferior mediastinum.
 The ascending aorta ends and the arch of aorta begins.
The ascending aorta ends and the arch of aorta begins.
 The arch of aorta ends and the thoracic aorta begins.
The arch of aorta ends and the thoracic aorta begins.
Intercostal spaces
Muscles
Intercostal muscles
Arterial supply
Posterior intercostal arteries
Anterior intercostal arteries
 the superior epigastric artery, which continues inferiorly into the anterior abdominal wall;
the superior epigastric artery, which continues inferiorly into the anterior abdominal wall;
 One passes below the margin of the upper rib.
One passes below the margin of the upper rib.
Venous drainage
Lymphatic drainage
Innervation
Intercostal nerves
 somatic sensory innervation from the skin and parietal pleura, and
somatic sensory innervation from the skin and parietal pleura, and
 postganglionic sympathetic fibers to the periphery.
postganglionic sympathetic fibers to the periphery.
 The anterior ramus of T1 contributes to the brachial plexus.
The anterior ramus of T1 contributes to the brachial plexus.
 The lower intercostal nerves supply muscles, skin, and parietal peritoneum of the abdominal wall.
The lower intercostal nerves supply muscles, skin, and parietal peritoneum of the abdominal wall.
DIAPHRAGM
 xiphoid process of the sternum,
xiphoid process of the sternum,
 costal margin of the thoracic wall,
costal margin of the thoracic wall,
 ligaments that span across structures of the posterior abdominal wall, and
ligaments that span across structures of the posterior abdominal wall, and
 vertebrae of the lumbar region.
vertebrae of the lumbar region.
 The inferior vena cava passes through the central tendon at approximately vertebral level TVIII.
The inferior vena cava passes through the central tendon at approximately vertebral level TVIII.
 The vagus nerves pass through the diaphragm with the esophagus.
The vagus nerves pass through the diaphragm with the esophagus.
 The aorta passes behind the posterior attachment of the diaphragm at vertebral level TXII.
The aorta passes behind the posterior attachment of the diaphragm at vertebral level TXII.
 The thoracic duct passes behind the diaphragm with the aorta.
The thoracic duct passes behind the diaphragm with the aorta.
Arterial supply
Venous drainage
 the brachiocephalic veins in the neck,
the brachiocephalic veins in the neck,
 the azygos system of veins, or
the azygos system of veins, or
 the abdominal veins (left suprarenal vein and inferior vena cava).
the abdominal veins (left suprarenal vein and inferior vena cava).
Innervation
MOVEMENTS OF THE THORACIC WALL AND DIAPHRAGM DURING BREATHING
PLEURAL CAVITIES
 superiorly, they extend above rib I into the root of the neck;
superiorly, they extend above rib I into the root of the neck;
 inferiorly, they extend to a level just above the costal margin; and
inferiorly, they extend to a level just above the costal margin; and
 the medial wall of each pleural cavity is the mediastinum (Fig. 3.31).
the medial wall of each pleural cavity is the mediastinum (Fig. 3.31).
Pleura
 pleura associated with the walls of a pleural cavity is parietal pleura (Fig. 3.30); and
pleura associated with the walls of a pleural cavity is parietal pleura (Fig. 3.30); and
 pleura that reflects from the medial wall and onto the surface of the lung is visceral pleura (Fig. 3.30), which adheres to and covers the lung.
pleura that reflects from the medial wall and onto the surface of the lung is visceral pleura (Fig. 3.30), which adheres to and covers the lung.
Parietal pleura
 Pleura related to the ribs and intercostal spaces is termed the costal part.
Pleura related to the ribs and intercostal spaces is termed the costal part.
 Pleura covering the diaphragm is the diaphragmatic part.
Pleura covering the diaphragm is the diaphragmatic part.
 Pleura covering the mediastinum is the mediastinal part.
Pleura covering the mediastinum is the mediastinal part.
Peripheral reflections
Visceral pleura
Costomediastinal recesses
Costodiaphragmatic recesses
Lungs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases a wall,
a wall, two pleural cavities,
two pleural cavities, the lungs, and
the lungs, and the mediastinum.
the mediastinum.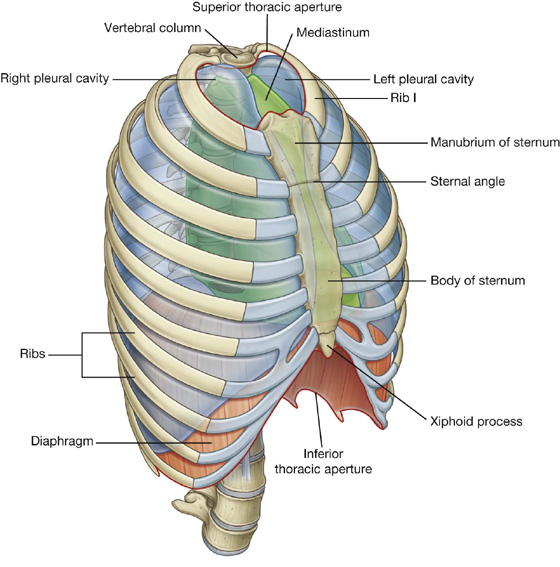
 laterally, vessels from the axillary artery—superior thoracic, thoracoacromial, lateral thoracic, and subscapular arteries;
laterally, vessels from the axillary artery—superior thoracic, thoracoacromial, lateral thoracic, and subscapular arteries; from the second to fourth intercostal arteries via branches that perforate the thoracic wall and overlying muscle.
from the second to fourth intercostal arteries via branches that perforate the thoracic wall and overlying muscle. Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery.
Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery. Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.
Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.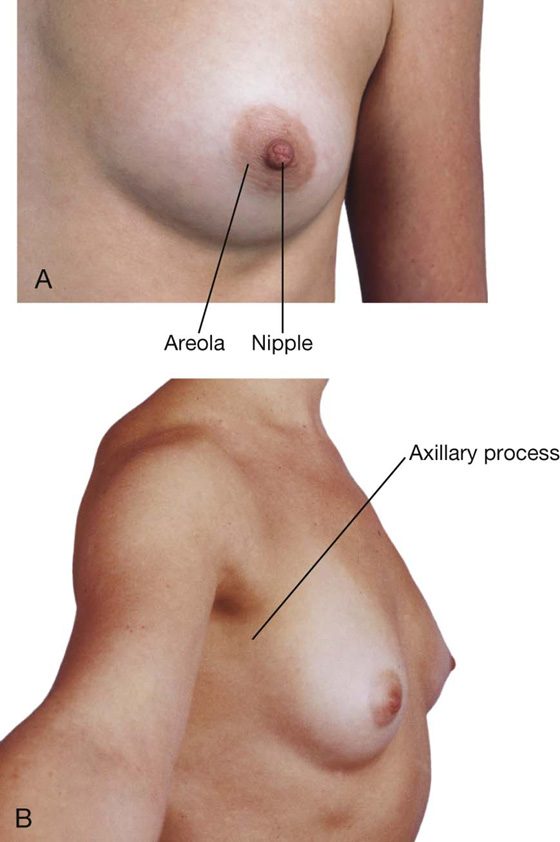
 Laterally, the wall is formed by ribs (12 on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces.
Laterally, the wall is formed by ribs (12 on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces. Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process.
Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process. the inferior thoracic aperture bordered by vertebra TXII, rib XII, the end of rib XI, the costal margin, and the xiphoid process of the sternum.
the inferior thoracic aperture bordered by vertebra TXII, rib XII, the end of rib XI, the costal margin, and the xiphoid process of the sternum. the manubrium anteriorly.
the manubrium anteriorly.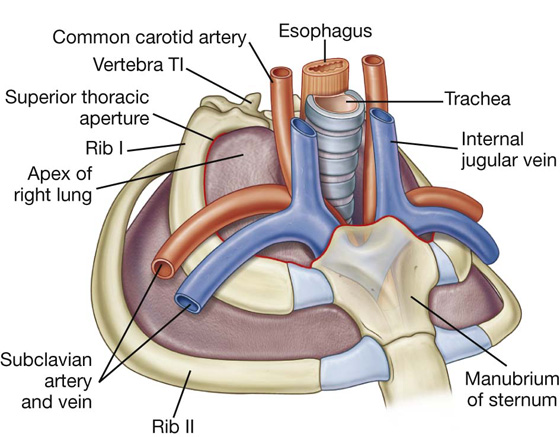
 the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and
the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and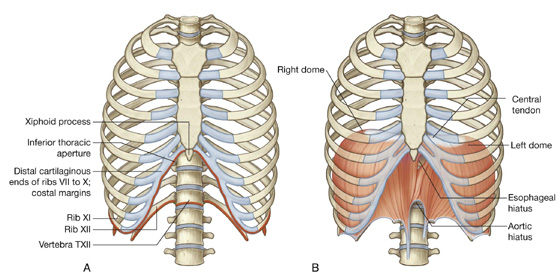
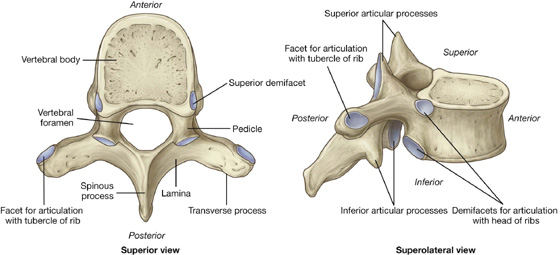
 Two demifacets (i.e., partial facets) located on the superior and inferior aspects of the body for articulation with corresponding sites on the heads of adjacent ribs. The superior costal facet articulates with part of the head of its own rib, and the inferior costal facet articulates with part of the head of the rib below.
Two demifacets (i.e., partial facets) located on the superior and inferior aspects of the body for articulation with corresponding sites on the heads of adjacent ribs. The superior costal facet articulates with part of the head of its own rib, and the inferior costal facet articulates with part of the head of the rib below. An oval facet (transverse costal facet) at the end of the transverse process articulates with the tubercle of its own rib.
An oval facet (transverse costal facet) at the end of the transverse process articulates with the tubercle of its own rib. The superior costal facets on the body of vertebra TI are complete and articulate with a single facet on the head of its own rib—in other words, the head of rib I does not articulate with vertebra CVII.
The superior costal facets on the body of vertebra TI are complete and articulate with a single facet on the head of its own rib—in other words, the head of rib I does not articulate with vertebra CVII. Similarly, vertebra TX (and often TIX) articulates only with its own ribs and therefore lacks inferior demifacets on the body.
Similarly, vertebra TX (and often TIX) articulates only with its own ribs and therefore lacks inferior demifacets on the body. Vertebrae TXI and TXII articulate only with the heads of their own ribs—they lack transverse costal facets and have only a single complete facet on each side of their bodies.
Vertebrae TXI and TXII articulate only with the heads of their own ribs—they lack transverse costal facets and have only a single complete facet on each side of their bodies.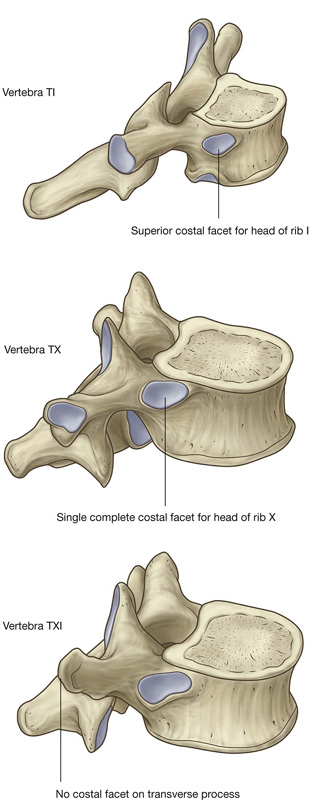
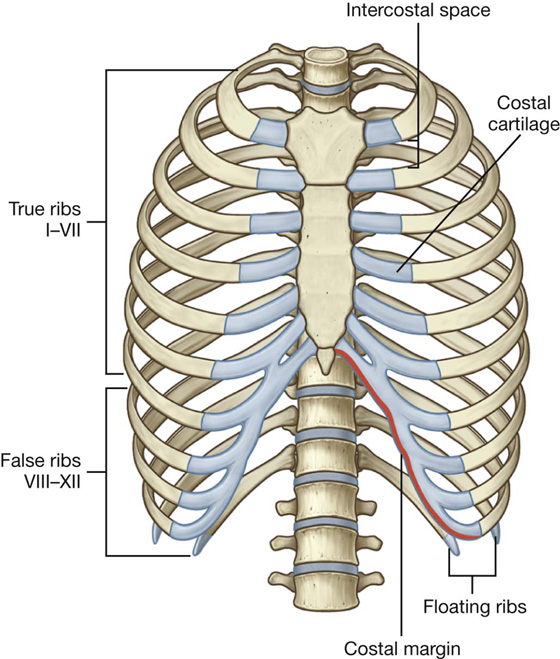
 The costal cartilages of ribs VIII to X articulate anteriorly with the costal cartilages of the ribs above.
The costal cartilages of ribs VIII to X articulate anteriorly with the costal cartilages of the ribs above. Ribs XI and XII have no anterior connection with other ribs or with the sternum and are often called floating ribs.
Ribs XI and XII have no anterior connection with other ribs or with the sternum and are often called floating ribs.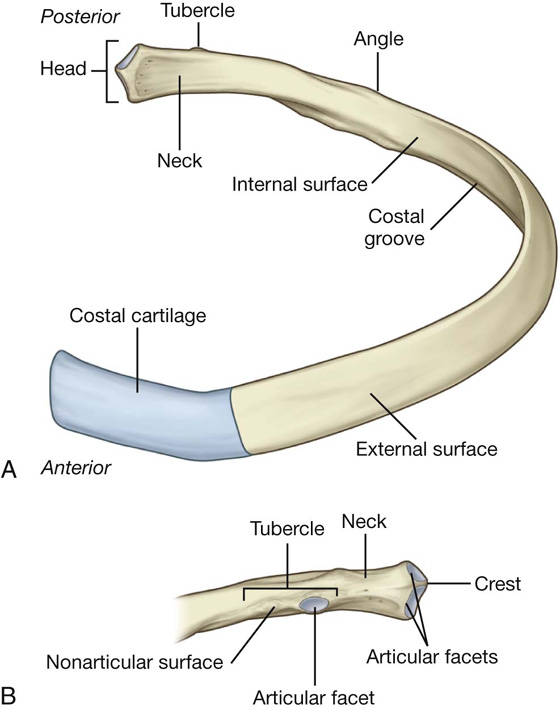
 The articular part is medial and has an oval facet for articulation with a corresponding facet on the transverse process of the associated vertebra.
The articular part is medial and has an oval facet for articulation with a corresponding facet on the transverse process of the associated vertebra.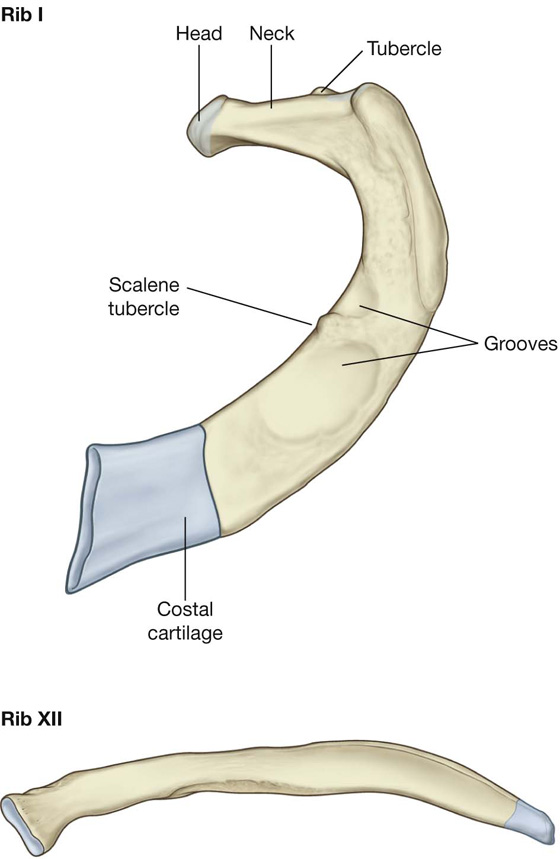
 The costotransverse ligament is medial to the joint and attaches the neck of the rib to the transverse process.
The costotransverse ligament is medial to the joint and attaches the neck of the rib to the transverse process. The lateral costotransverse ligament is lateral to the joint and attaches the tip of the transverse process to the roughened nonarticular part of the tubercle of the rib.
The lateral costotransverse ligament is lateral to the joint and attaches the tip of the transverse process to the roughened nonarticular part of the tubercle of the rib.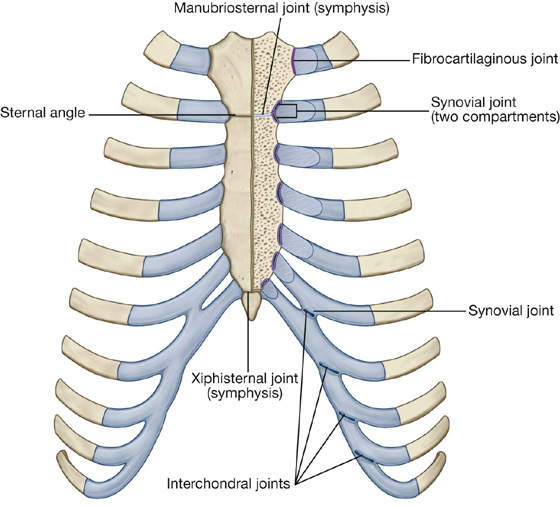
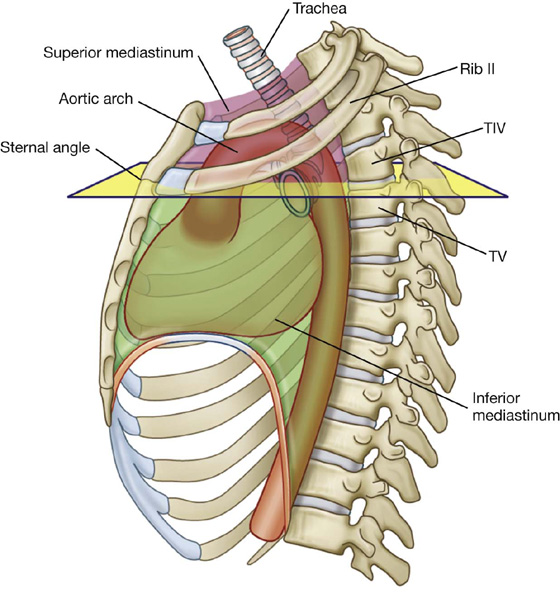
 The trachea bifurcates.
The trachea bifurcates.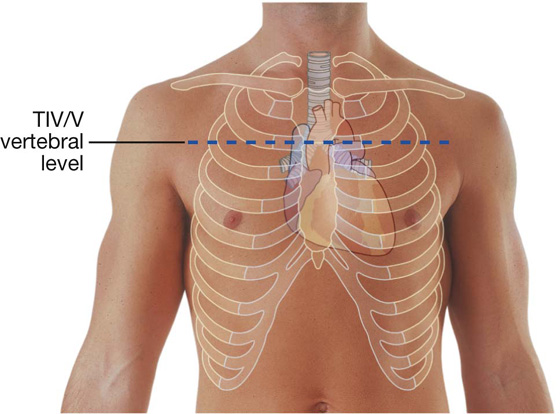
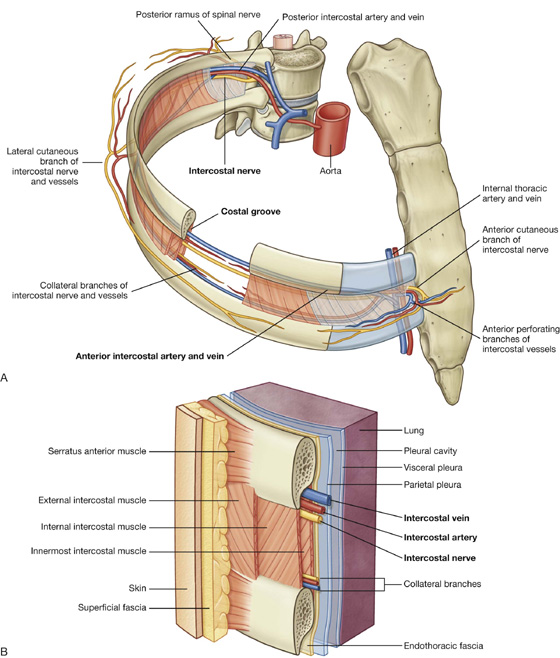
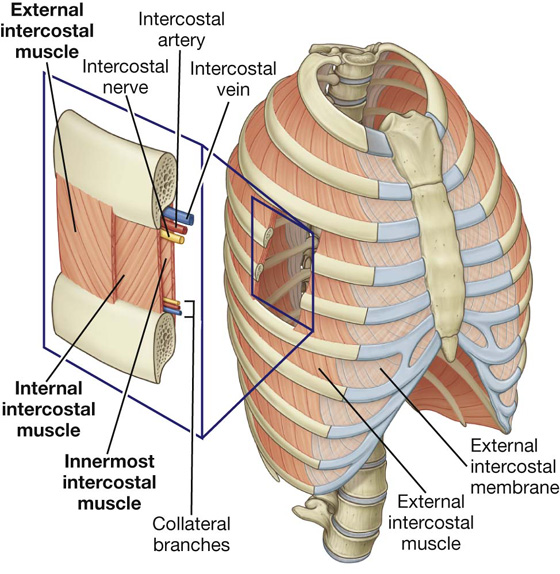
 The external intercostal muscles are the most superficial and their fibers pass from the rib above anteroinferiorly to the rib below (these muscles extend around the thoracic wall from the regions of the tubercles of the ribs to the costal cartilages, where each muscle continues as a thin connective tissue aponeurosis termed the external intercostal membrane).
The external intercostal muscles are the most superficial and their fibers pass from the rib above anteroinferiorly to the rib below (these muscles extend around the thoracic wall from the regions of the tubercles of the ribs to the costal cartilages, where each muscle continues as a thin connective tissue aponeurosis termed the external intercostal membrane). The internal intercostal muscles are sandwiched between the external and innermost muscles, and their fibers run in the opposite direction to those of the external intercostal muscles (the internal intercostal muscles extend around the thoracic wall from the sternum to the angles of the ribs, where each muscle continues as a thin connective tissue aponeurosis termed the internal intercostal membrane).
The internal intercostal muscles are sandwiched between the external and innermost muscles, and their fibers run in the opposite direction to those of the external intercostal muscles (the internal intercostal muscles extend around the thoracic wall from the sternum to the angles of the ribs, where each muscle continues as a thin connective tissue aponeurosis termed the internal intercostal membrane). The innermost intercostal muscles are the deepest of the three muscles and their fibers course in a similar direction as the internal intercostal muscles.
The innermost intercostal muscles are the deepest of the three muscles and their fibers course in a similar direction as the internal intercostal muscles.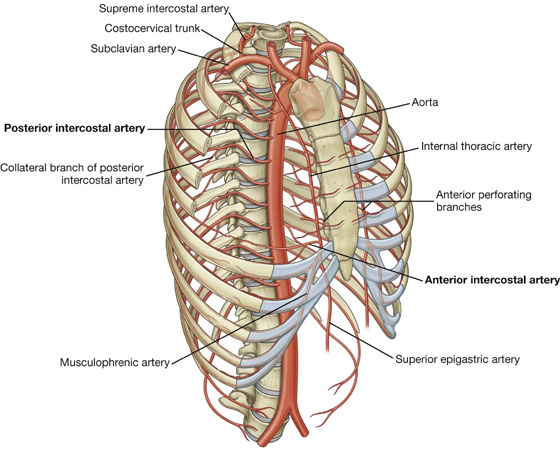
 the musculophrenic artery, which passes along the costal margin, goes through the diaphragm, and ends near the last intercostal space.
the musculophrenic artery, which passes along the costal margin, goes through the diaphragm, and ends near the last intercostal space. The other passes above the margin of the lower rib and meets a collateral branch of the posterior intercostal artery.
The other passes above the margin of the lower rib and meets a collateral branch of the posterior intercostal artery.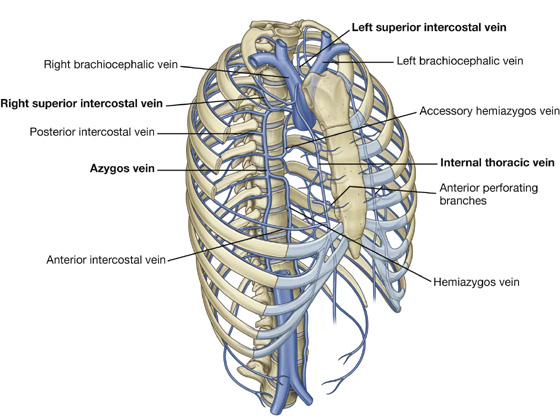
 somatic motor innervation to the muscles of the thoracic wall (intercostal, subcostal, and transversus thoracis muscles),
somatic motor innervation to the muscles of the thoracic wall (intercostal, subcostal, and transversus thoracis muscles), The lateral cutaneous branch of the second intercostal nerve (the intercostobrachial nerve) contributes to cutaneous innervation of the medial surface of the upper arm.
The lateral cutaneous branch of the second intercostal nerve (the intercostobrachial nerve) contributes to cutaneous innervation of the medial surface of the upper arm. ends of ribs XI and XII,
ends of ribs XI and XII,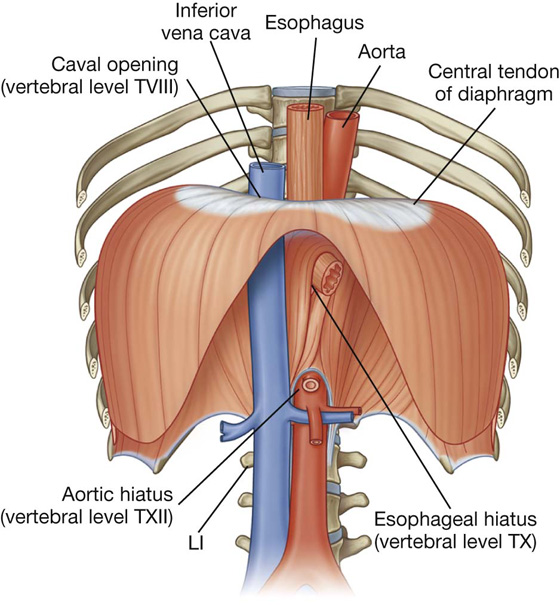
 The esophagus passes through the muscular part of the diaphragm, just to the left of midline, approximately at vertebral level TX.
The esophagus passes through the muscular part of the diaphragm, just to the left of midline, approximately at vertebral level TX. The azygos and hemiazygos veins may also pass through the aortic hiatus or through the crura of the diaphragm.
The azygos and hemiazygos veins may also pass through the aortic hiatus or through the crura of the diaphragm.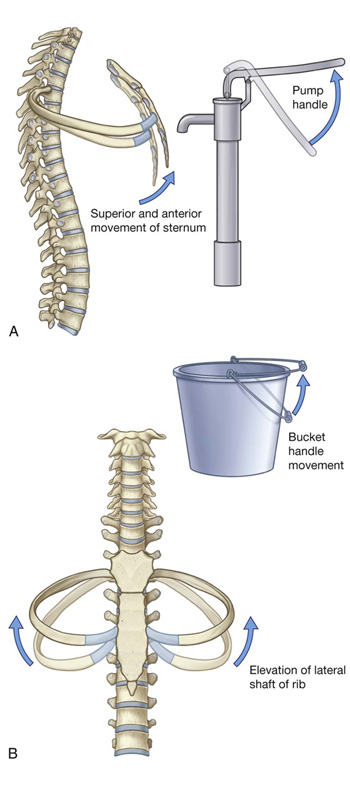
 The dome-shaped layer of parietal pleura lining the cervical extension of the pleural cavity is cervical pleura (dome of pleura or pleural cupola).
The dome-shaped layer of parietal pleura lining the cervical extension of the pleural cavity is cervical pleura (dome of pleura or pleural cupola).