7
Upper Limb
Gateways to the posterior scapular region
Gateways in the posterior wall
Anterior compartment of the forearm
Posterior compartment of forearm
Carpal tunnel and structures at the wrist
ADDITIONAL LEARNING RESOURCES FOR CHAPTER 7, UPPER LIMB, ON STUDENT CONSULT (www.studentconsult.com)
 Image Library—illustrations of upper limb anatomy, Chapter 7
Image Library—illustrations of upper limb anatomy, Chapter 7
 Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 7
Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 7
 Short Questions (not scored)—National Board style multiple-choice questions, Chapter 7
Short Questions (not scored)—National Board style multiple-choice questions, Chapter 7
 Interactive Surface Anatomy—interactive surface animations, Chapter 7
Interactive Surface Anatomy—interactive surface animations, Chapter 7
Upper quarter screening examination
See more PT Case Studies online
Extensor tendon injury of the hand
See more Medical Clinical Case Studies online
Complication of a fractured first rib
Regional anatomy
Based on the position of its major joints, the upper limb is divided into shoulder, arm, forearm, and hand (Fig. 7.1):
 The arm is between the shoulder and the elbow joint. The bone of the arm is the humerus.
The arm is between the shoulder and the elbow joint. The bone of the arm is the humerus.
Fig. 7.1 Anterior view of the upper limb.
The major function of the upper limb is to position the hand in space for use as a mechanical and sensory tool.
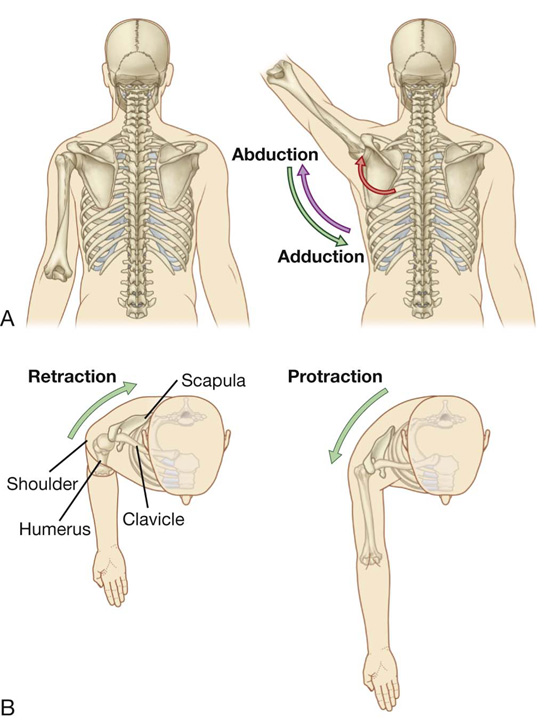
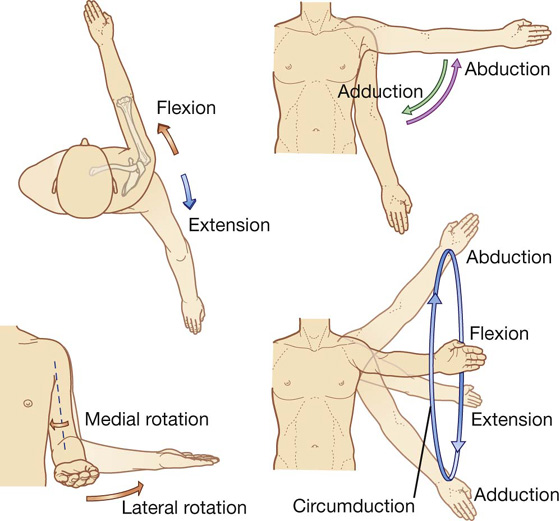
Unlike the lower limb, which is used for support, stability, and locomotion, the upper limb is designed to be flexible. The shoulder is suspended from the trunk predominantly by muscles and can therefore be moved relative to the body. Sliding (protraction and retraction) and rotating the scapula on the thoracic wall changes the position of the glenohumeral joint (shoulder joint) and extends the reach of the hand (Fig. 7.2). The glenohumeral joint allows the arm to move around three axes with a wide range of motion. Movements of the arm at this joint are flexion, extension, abduction, adduction, medial rotation (internal rotation), lateral rotation (external rotation), and circumduction (Fig. 7.3).
Fig. 7.2 Movements of the scapula. A. Rotation. B. Protraction and retraction.
Fig. 7.3 Movements of the arm at the glenohumeral joint.
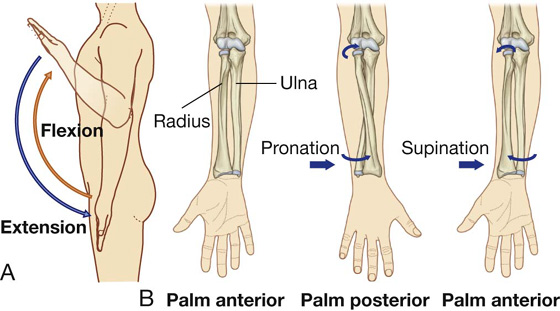
The major movements at the elbow joint are flexion and extension of the forearm (Fig. 7.4A). At the other end of the forearm, the distal end of the lateral bone, the radius, can be flipped over the adjacent head of the medial bone, the ulna. Because the hand is articulated with the radius, it can be efficiently moved from a palm-anterior position to a palm-posterior position simply by crossing the distal end of the radius over the ulna (Fig. 7.4B). This movement, termed pronation, occurs solely in the forearm. Supination returns the hand to the anatomical position.
Fig. 7.4 Movements of the forearm. A. Flexion and extension at the elbow joint. B. Pronation and supination.
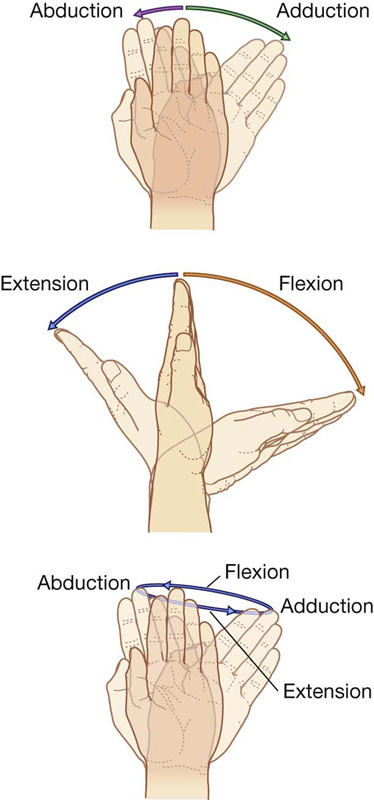
At the wrist joint, the hand can be abducted, adducted, flexed, extended, and circumducted (Fig. 7.5). These movements, combined with those of the shoulder, arm, and forearm, enable the hand to be placed in a wide range of positions relative to the body.
Fig. 7.5 Movements of the hand at the wrist joint.
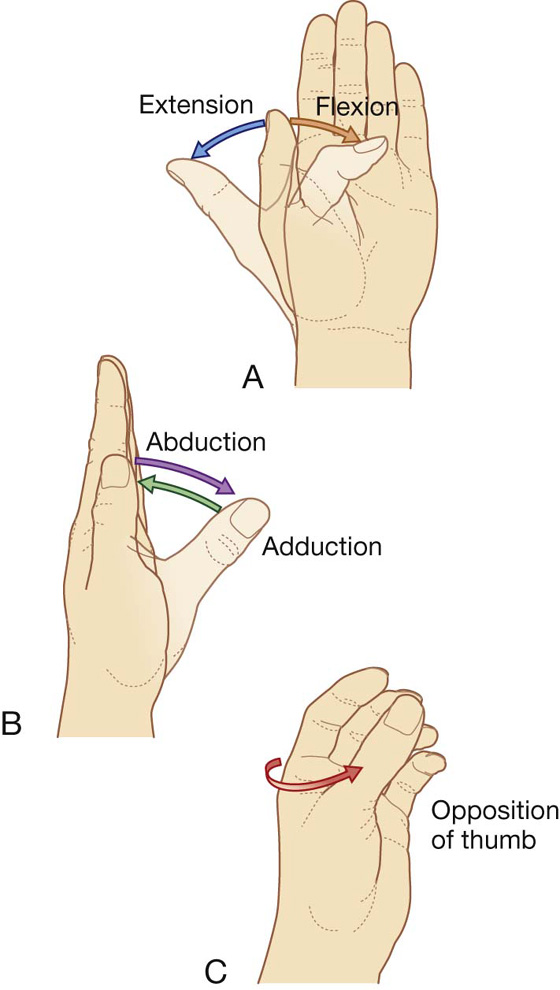
The thumb is positioned at right angles to the orientation of the index, middle, ring, and little fingers (Fig. 7.6). As a result, movements of the thumb occur at right angles to those of the other digits. For example, flexion brings the thumb across the palm, whereas abduction moves it away from the fingers at right angles to the palm (Fig. 7.6A,B).
Fig. 7.6 A–C. Movements of the thumb.
Importantly, with the thumb positioned at right angles to the palm. Only a slight rotation of the thumb brings it into a position directly facing the other fingers (Fig. 7.6C). This opposition of the thumb is essential for normal hand function.
SHOULDER
The bone framework of the shoulder consists of:
 the clavicle and scapula, which form the pectoral girdle (shoulder girdle), and
the clavicle and scapula, which form the pectoral girdle (shoulder girdle), and
 the proximal end of the humerus.
the proximal end of the humerus.
The superficial muscles of the shoulder consist of the trapezius and deltoid muscles, which together form the smooth muscular contour over the lateral part of the shoulder. These muscles connect the scapula and clavicle to the trunk and to the arm, respectively.
Bones
Clavicle
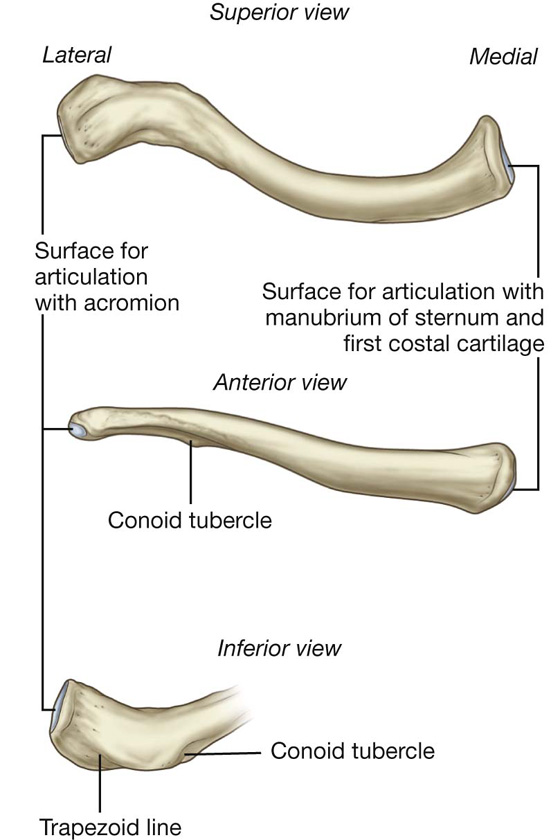
The clavicle is the only bony attachment between the trunk and the upper limb. It is palpable along its entire length and has a gentle S-shaped contour, with the forward-facing convex part medial and the forward-facing concave part lateral. The acromial (lateral) end of the clavicle is flat, whereas the sternal (medial) end is more robust and somewhat quadrangular in shape (Fig. 7.7).
Fig. 7.7 Right clavicle.
The acromial end of the clavicle has a small oval facet on its surface for articulation with a similar facet on the medial surface of the acromion of the scapula.
The sternal end has a much larger facet for articulation mainly with the manubrium of the sternum, and to a lesser extent, with the first costal cartilage.
The inferior surface of the lateral third of the clavicle possesses a distinct tuberosity consisting of a tubercle (the conoid tubercle) and lateral roughening (the trapezoid line), for attachment of the important coracoclavicular ligament.
In addition, the surfaces and margins of the clavicle are roughened by the attachment of muscles that connect the clavicle to the thorax, neck, and upper limb. The superior surface is smoother than the inferior surface.
Scapula
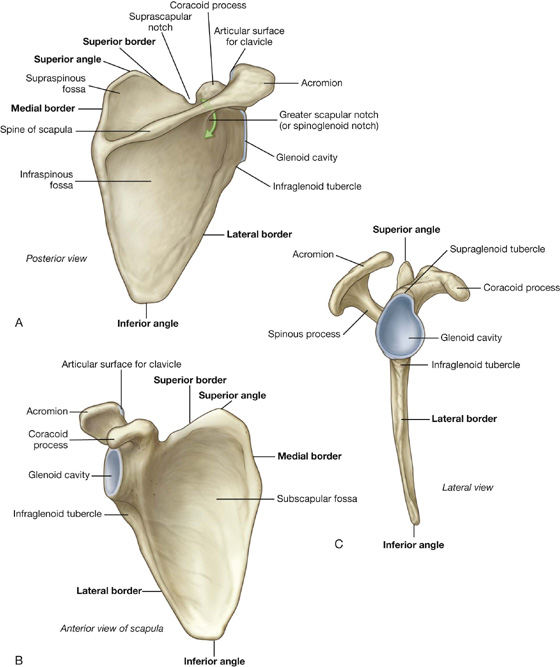
The scapula is a large, flat triangular bone with (Fig. 7.8):
 three angles (lateral, superior, and inferior);
three angles (lateral, superior, and inferior);
 three borders (superior, lateral, and medial);
three borders (superior, lateral, and medial);
 two surfaces (costal and posterior); and
two surfaces (costal and posterior); and
 three processes (acromion, spine, and coracoid process)
three processes (acromion, spine, and coracoid process)
Fig. 7.8 Scapula. A. Posterior view of right scapula. B. Anterior view of costal surface. C. Lateral view.
The lateral angle of the scapula is marked by a shallow, somewhat comma-shaped glenoid cavity, which articulates with the head of the humerus to form the glenohumeral joint (Fig. 7.8B,C).
A large triangular-shaped roughening (the infraglenoid tubercle) inferior to the glenoid cavity is the site of attachment for the long head of the triceps brachii muscle (Fig. 7.8B,C).
A less distinct supraglenoid tubercle is located superior to the glenoid cavity and is the site of attachment for the long head of the biceps brachii muscle (Fig. 7.8C).
A prominent spine subdivides the posterior surface of the scapula into a small, superior supraspinous fossa and a much larger, inferior infraspinous fossa (Fig. 7.8A).
The acromion, which is an anterolateral projection of the spine, arches over the glenohumeral joint and articulates, via a small oval facet on its distal end, with the clavicle (Fig. 7.8B).
The region between the lateral angle of the scapula and the attachment of the spine to the posterior surface of the scapula is the greater scapular notch (spinoglenoid notch) (Fig. 7.8A).
Unlike the posterior surface, the costal surface of the scapula is unremarkable, being characterized by a shallow concave subscapular fossa over much of its extent (Fig. 7.8B). The costal surface and margins provide for muscle attachment, and the costal surface, together with its related muscle (subscapularis), moves freely over the underlying thoracic wall.
The lateral border of the scapula is strong and thick for muscle attachment, whereas the medial border and much of the superior border is thin and sharp.
The superior border is marked on its lateral end by:
 the coracoid process (Fig. 7.8B,C), a hooklike structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; and
the coracoid process (Fig. 7.8B,C), a hooklike structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; and
 the small but distinct suprascapular notch (Fig. 7.8A), which lies immediately medial to the root of the coracoid process.
the small but distinct suprascapular notch (Fig. 7.8A), which lies immediately medial to the root of the coracoid process.
The spine and acromion can be readily palpated on a patient, as can the tip of the coracoid process, the inferior angle, and much of the medial border of the scapula.
Proximal humerus
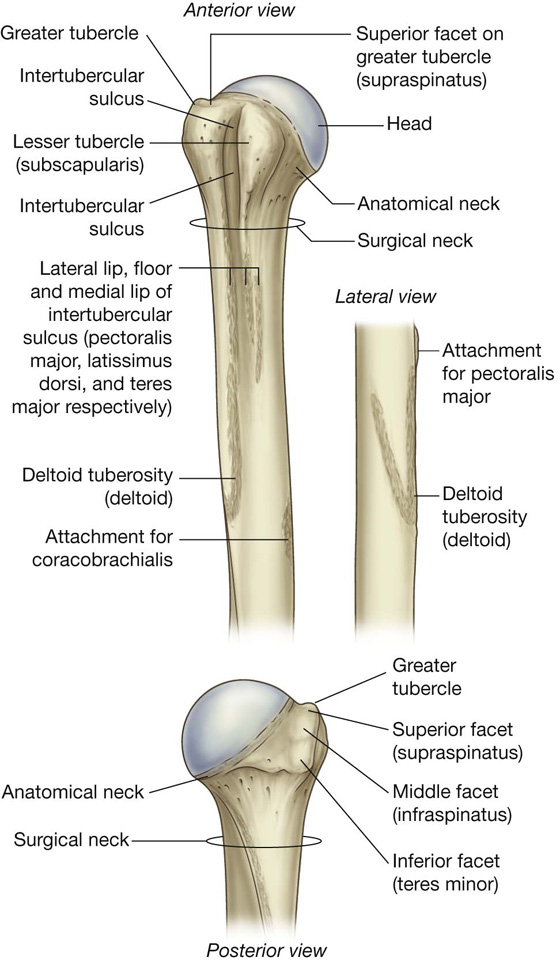
The proximal end of the humerus consists of the head, the anatomical neck, the greater and lesser tubercles, the surgical neck, and the superior half of the shaft of humerus (Fig. 7.9).
Fig. 7.9 Proximal end of right humerus.
The head is half-spherical in shape and projects medially and somewhat superiorly to articulate with the much smaller glenoid cavity of the scapula.
The anatomical neck is very short and is formed by a narrow constriction immediately distal to the head. It lies between the head and the greater and lesser tubercles laterally, and between the head and the shaft more medially.
Greater and lesser tubercles
The greater and lesser tubercles are prominent landmarks on the proximal end of the humerus and serve as attachment sites for the four rotator cuff muscles of the glenohumeral joint (Fig. 7.9).
The greater tubercle is lateral in position. Its superior surface and posterior surface are marked by three large smooth facets for muscle tendon attachment (Fig. 7.9):
 The superior facet is for attachment of the supraspinatus muscle.
The superior facet is for attachment of the supraspinatus muscle.
 The middle facet is for attachment of infraspinatus.
The middle facet is for attachment of infraspinatus.
 The inferior facet is for attachment of teres minor.
The inferior facet is for attachment of teres minor.
The lesser tubercle is anterior in position and its surface is marked by a large smooth impression for attachment of the subscapularis muscle.
A deep intertubercular sulcus (bicipital groove) separates the lesser and greater tubercles and continues inferiorly onto the proximal shaft of the humerus (Fig. 7.9). The tendon of the long head of the biceps brachii passes through this sulcus.
Roughenings on the lateral and medial lips and on the floor of the intertubercular sulcus mark sites for the attachment of the pectoralis major, teres major, and latissimus dorsi muscles, respectively.
The lateral lip of the intertubercular sulcus is continuous inferiorly with a large V-shaped deltoid tuberosity on the lateral surface of the humerus midway along its length (Fig. 7.9), which is where the deltoid muscle inserts onto the humerus.
In approximately the same position, but on the medial surface of the bone, there is a thin vertical roughening for attachment of the coracobrachialis muscle.
Surgical neck
One of the most important features of the proximal end of the humerus is the surgical neck (Fig. 7.9). This region is oriented in the horizontal plane between the expanded proximal part of the humerus (head, anatomical neck, and tubercles) and the narrower shaft. The axillary nerve and the posterior circumflex humeral artery, which pass into the deltoid region from the axilla, do so immediately posterior to the surgical neck. Because the surgical neck is weaker than more proximal regions of the bone, it is one of the sites where the humerus commonly fractures.
Clinical app
Fracture of the proximal humerus
Typically, fractures occur around the surgical neck of the humerus. Although the axillary nerve and posterior circumflex humeral artery may be damaged with this type of fracture, this rarely happens. However, it is important that the axillary nerve is tested to be sure that the injury has not damaged the nerve and that the treatment itself does not cause a neurological deficit.
Joints
The three joints in the shoulder complex are the sternoclavicular, acromioclavicular, and glenohumeral joints.
The sternoclavicular joint and the acromioclavicular joint link the two bones of the pectoral girdle to each other and to the trunk. The combined movements at these two joints enable the scapula to be positioned over a wide range on the thoracic wall, substantially increasing “reach” by the upper limb.
The glenohumeral joint (shoulder joint) is the articulation between the humerus of the arm and the scapula.
Sternoclavicular joint
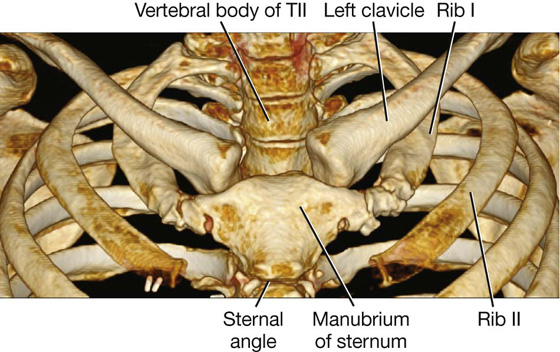
The sternoclavicular joint occurs between the proximal end of the clavicle and the clavicular notch of the manubrium of sternum together with a small part of the first costal cartilage (Fig. 7.10, 7.11). It is synovial and saddle-shaped. The articular cavity is completely separated into two compartments by an articular disc. The sternoclavicular joint allows movement of the clavicle, predominantly in the anteroposterior and vertical planes, although some rotation also occurs.
Fig. 7.10 Sternoclavicular joint.
Imaging app
Visualizing the sternoclavicular joint
Fig. 7.11 Anterior view of normal sternoclavicular joints. Volume-rendered reconstruction using multidetector computed tomography.
The sternoclavicular joint is surrounded by a joint capsule and is reinforced by four ligaments (Fig. 7.10):
Acromioclavicular joint
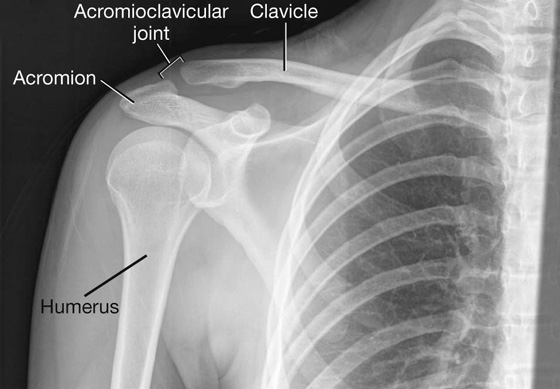
The acromioclavicular joint is a small synovial joint between an oval facet on the medial surface of the acromion and a similar facet on the acromial end of the clavicle (Figs. 7.12; 7.13). It allows movement in the anteroposterior and vertical planes together with some axial rotation.
Fig. 7.12 Right acromioclavicular joint.
Imaging app
Visualizing the acromioclavicular joint
Fig. 7.13 Radiograph of a normal right acromioclavicular joint (anteroposterior view).
The acromioclavicular joint is surrounded by a joint capsule and is reinforced by (Fig. 7.12):
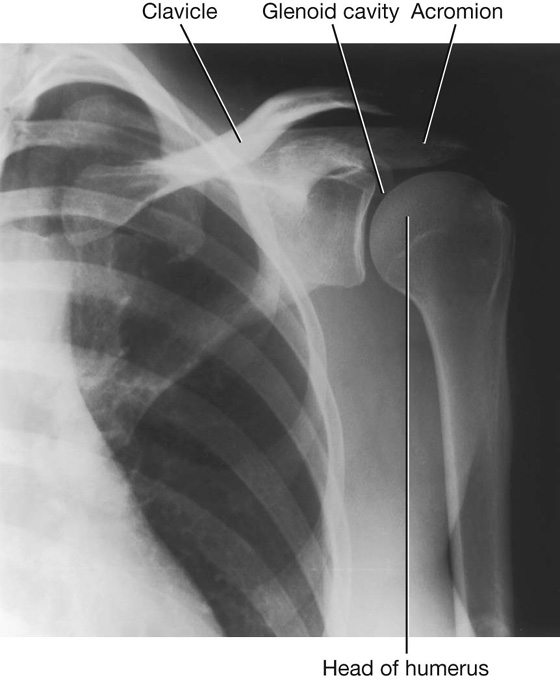
Glenohumeral joint
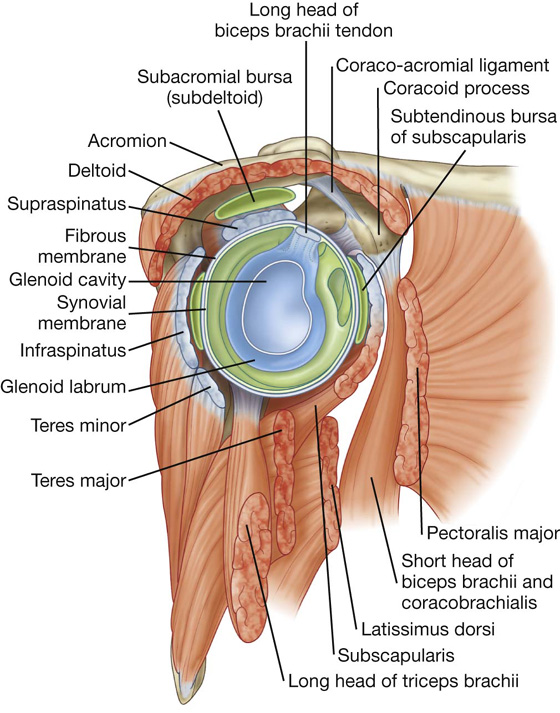
The glenohumeral joint is a synovial ball and socket articulation between the head of the humerus and the glenoid cavity of the scapula (Fig. 7.14; see Fig. 7.15). It is multiaxial with a wide range of movements provided at the cost of skeletal stability. Joint stability is provided instead by the rotator cuff muscles, the long head of the biceps brachii muscle, related bony processes, and extracapsular ligaments.
Fig. 7.14 Articular surfaces of right glenohumeral joint.
The articular surfaces of the glenohumeral joint are the large spherical head of the humerus and the small glenoid cavity of the scapula (Fig. 7.14).
The glenoid cavity is deepened and expanded peripherally by a fibrocartilaginous collar (the glenoid labrum), which attaches to the margin of the fossa (Fig. 7.14). Superiorly, this labrum is continuous with the tendon of the long head of the biceps brachii muscle, which attaches to the supraglenoid tubercle and passes through the articular cavity superior to the head of the humerus.
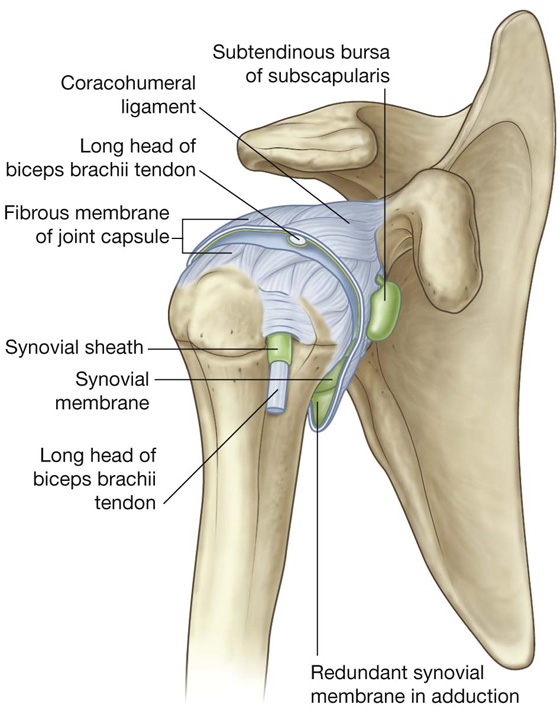
The synovial membrane attaches to the margins of the articular surfaces and lines the fibrous membrane of the joint capsule (Fig. 7.16). The synovial membrane is loose inferiorly. This redundant region of synovial membrane and related fibrous membrane accommodates abduction of the arm.
Fig. 7.16 Synovial membrane and joint capsule of right glenohumeral joint.
The synovial membrane protrudes through apertures in the fibrous membrane to form bursae, which lie between the tendons of surrounding muscles and the fibrous membrane. The most consistent of these is the subtendinous bursa of subscapularis (Figs. 7.16, 7.17), which lies between the subscapularis muscle and the fibrous membrane. The synovial membrane also folds around the tendon of the long head of the biceps brachii muscle in the joint and extends along the tendon as it passes into the intertubercular sulcus (Figs. 7.16, 7.18). All these synovial structures reduce friction between the tendons and adjacent joint capsule and bone.
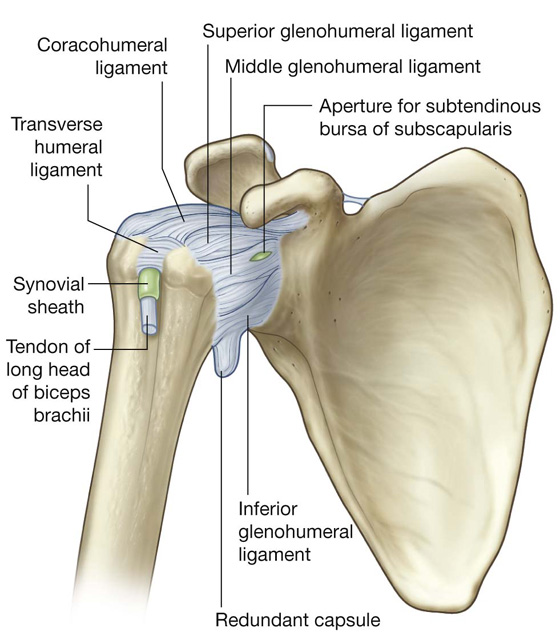
Fig. 7.18 Capsule of right glenohumeral joint.
In addition to bursae that communicate with the articular cavity through apertures in the fibrous membrane, other bursae are associated with the joint but are not connected to it. These occur:
 between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa) (Fig. 7.17);
between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa) (Fig. 7.17);
 between the acromion and skin;
between the acromion and skin;
 between the coracoid process and the joint capsule; and
between the coracoid process and the joint capsule; and
The fibrous membrane of the joint capsule attaches to the margin of the glenoid cavity, outside the attachment of the glenoid labrum and the long head of the biceps brachii muscle, and to the anatomical neck of the humerus (Fig. 7.18).
Openings in the fibrous membrane provide continuity of the articular cavity with bursae that occur between the joint capsule and surrounding muscles and around the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.
The fibrous membrane of the joint capsule is thickened (Fig. 7.18):
Joint stability is provided by surrounding muscle tendons and a skeletal arch formed superiorly by the coracoid process and acromion and the coraco-acromial ligament (Fig. 7.17).
Imaging app
Visualizing the rotator cuff muscles
Fig. 7.19 Magnetic resonance image (T1-weighted) of a normal glenohumeral joint in the sagittal plane.
Tendons of the rotator cuff muscles (the supraspinatus, infraspinatus, teres minor, and subscapularis muscles) blend with the joint capsule and form a musculotendinous collar that surrounds the posterior, superior, and anterior aspects of the glenohumeral joint (see Figs. 7.17; 7.19). This cuff of muscles stabilizes and holds the head of the humerus in the glenoid cavity of the scapula without compromising the arm’s flexibility and range of motion. The tendon of the long head of the biceps brachii muscle passes superiorly through the joint and restricts upward movement of the humeral head on the glenoid cavity.
Vascular supply to the glenohumeral joint is predominantly through branches of the anterior and posterior circumflex humeral and suprascapular arteries.
The glenohumeral joint is innervated by branches from the posterior cord of the brachial plexus, and from the suprascapular, axillary, and lateral pectoral nerves.
Clinical app
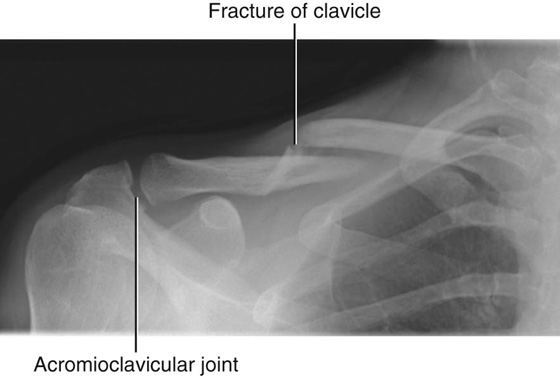
Fractures of the clavicle and dislocations of the acromioclavicular and sternoclavicular joints
The clavicle is often fractured because of its small size and the large forces that it often transmits from the upper limb to the trunk. The typical site of fracture is the middle third (Fig. 7.20), proximal to the attachment of the coracoclavicular ligament.
Fig. 7.20 Radiograph showing an oblique fracture of the middle third of the right clavicle.
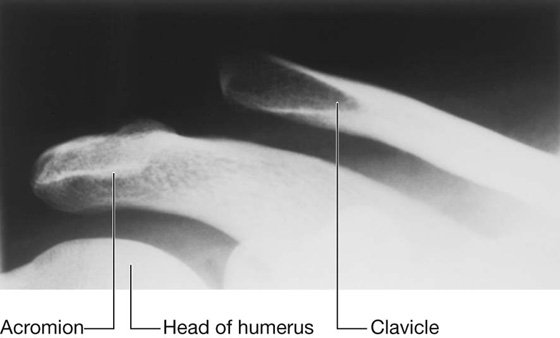
The acromial end of the clavicle tends to dislocate at the acromioclavicular joint with trauma (Fig. 7.21). A minor injury tends to tear the fibrous joint capsule and ligaments of the acromioclavicular joint, resulting in acromioclavicular separation on a plain radiograph. More severe trauma will disrupt the conoid and trapezoid ligaments of the coracoclavicular ligament, which results in elevation and upward subluxation of the clavicle.
Fig. 7.21 Radiograph of dislocated right acromioclavicular joint.
The typical injury at the medial end of the clavicle is an anterior or posterior dislocation of the sternoclavicular joint. Importantly, a posterior dislocation of the clavicle may impinge on the great vessels and compress or disrupt them.
Clinical app
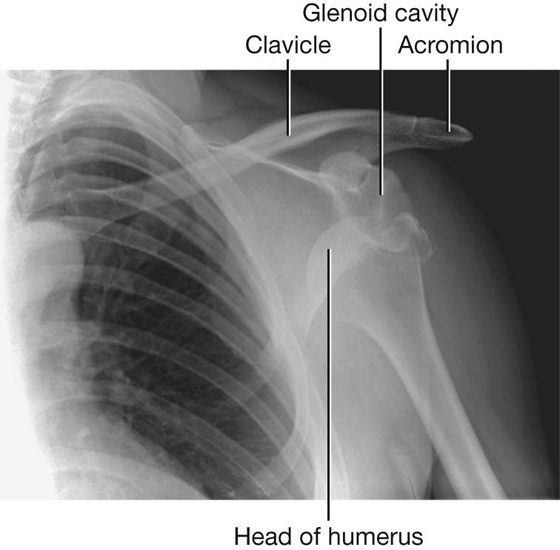
Dislocations of the glenohumeral joint
The glenohumeral joint is extremely mobile, providing a wide range of movement at the expense of stability. The relatively small bony glenoid cavity, supplemented by the less robust fibrocartilaginous glenoid labrum and the ligamentous support, make it susceptible to dislocation.
Anteroinferior dislocation (Fig. 7.22) occurs most frequently and is usually associated with an isolated traumatic incident (clinically, all anterior dislocations are anteroinferior). In some cases, the anteroinferior glenoid labrum is torn with or without a small bony fragment. Once the joint capsule and cartilage are disrupted, the joint is susceptible to further (recurrent) dislocations. When an anteroinferior dislocation occurs, the axillary nerve may be injured by direct compression of the humeral head on the nerve inferiorly as it passes through the quadrangular space. Furthermore, the “lengthening” effect of the humerus may stretch the radial nerve, which is tightly bound within the radial groove, and produce a radial nerve paralysis. Occasionally, an anteroinferior dislocation is associated with a fracture. Posterior dislocation is extremely rare.
Fig. 7.22 Radiograph showing an anteroinferior dislocation of the shoulder joint.
Clinical app
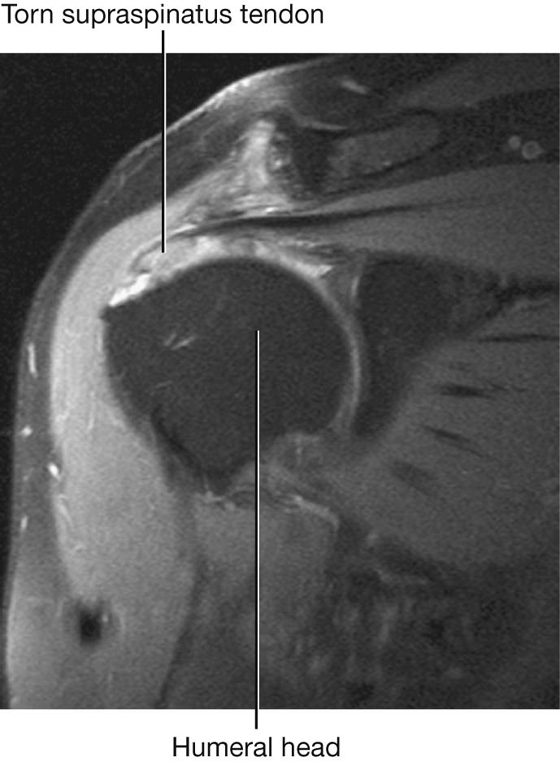
Rotator cuff disorders
The two main disorders of the rotator cuff are impingement and tendinopathy. The muscle most commonly involved is supraspinatus as it passes beneath the acromion and the acromioclavicular ligament. This space, beneath which the supraspinatus tendon passes, is of fixed dimensions. Swelling of the supraspinatus muscle, excessive fluid within the subacromial/subdeltoid bursa, or subacromial bony spurs may produce significant impingement when the arm is abducted.
The blood supply to the supraspinatus tendon is relatively poor. Repeated trauma, in certain circumstances, makes the tendon susceptible to degenerative change, which may result in calcium deposition, producing extreme pain.
When the supraspinatus tendon has undergone significant degenerative change, it is further susceptible to trauma and partial- or full-thickness tears may develop (Fig. 7.23). These tears are most common in older patients and may result in considerable difficulty in carrying out normal activities of daily living such as combing hair. However, complete tears may be entirely asymptomatic.
Muscles
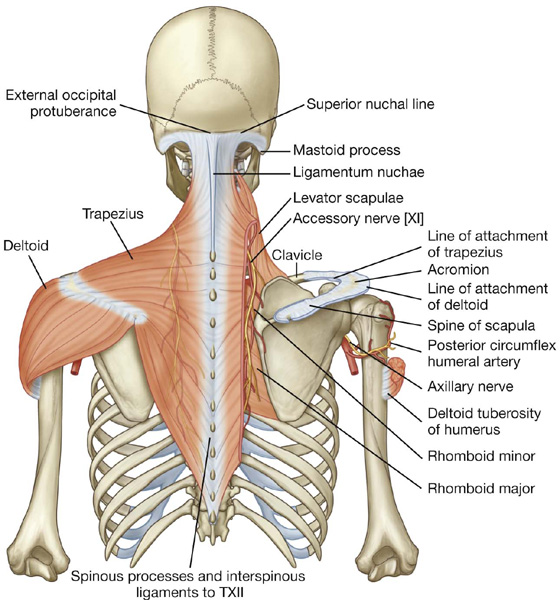
The two most superficial muscles of the shoulder are the trapezius and deltoid muscles (Table 7.1, Fig. 7.24). Together, they provide the characteristic contour of the shoulder:
 The trapezius attaches the scapula and clavicle to the trunk.
The trapezius attaches the scapula and clavicle to the trunk.
 The deltoid attaches the scapula and clavicle to the humerus.
The deltoid attaches the scapula and clavicle to the humerus.
Table 7.1 Muscles of the shoulder (spinal segments indicated in bold are the major segments innervating the muscle)
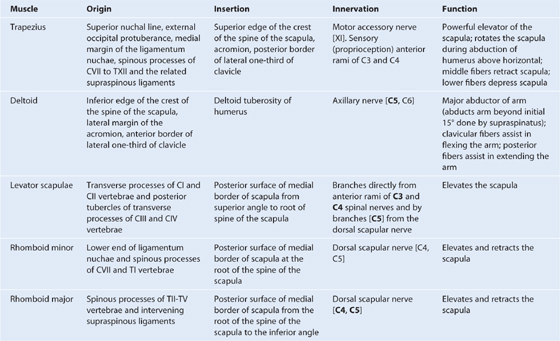
Fig. 7.24 Attachment and neurovascular supply of the trapezius and deltoid muscles.
Both the trapezius and deltoid are attached to opposing surfaces and margins of the spine of the scapula, the acromion, and the clavicle and these structures can be palpated between the attachments of trapezius and deltoid.
Deep to the trapezius the scapula is attached to the vertebral column by three muscles—the levator scapulae, rhomboid minor, and rhomboid major (Table 7.1, Fig. 7.24). These three muscles work with the trapezius (and with muscles found anteriorly) to position the scapula on the trunk.
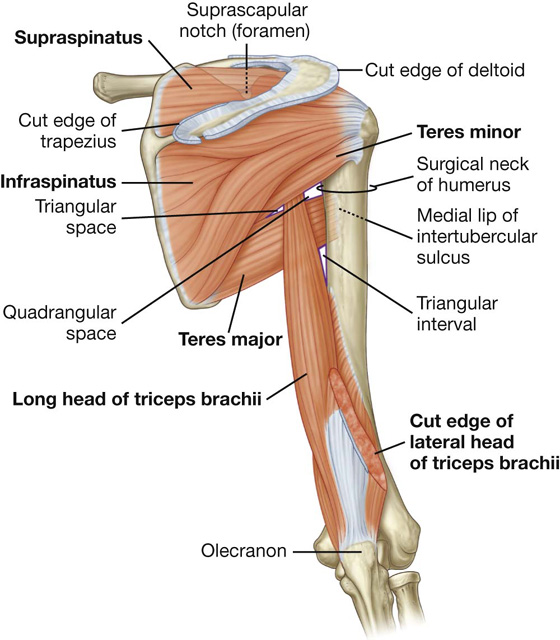
POSTERIOR SCAPULAR REGION
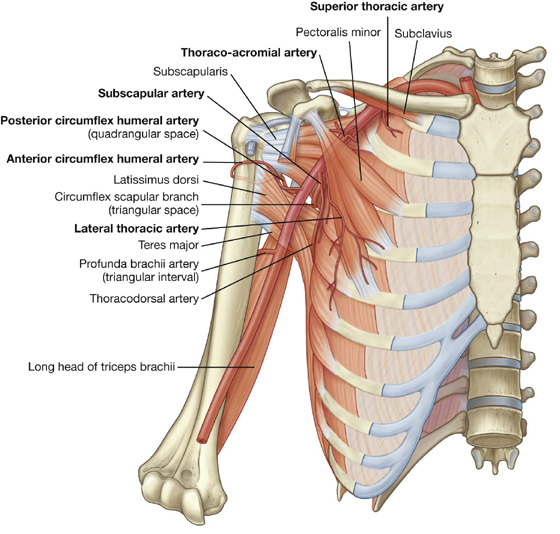
The posterior scapular region occupies the posterior aspect of the scapula and is located deep to the trapezius and deltoid muscles. It contains four muscles, which pass between the scapula and proximal end of the humerus: the supraspinatus, infraspinatus, teres minor, and teres major muscles (Table 7.2, Fig. 7.25).
Table 7.2 Muscles of the posterior scapular region (spinal segments indicated in bold are the major segments innervating the muscle)
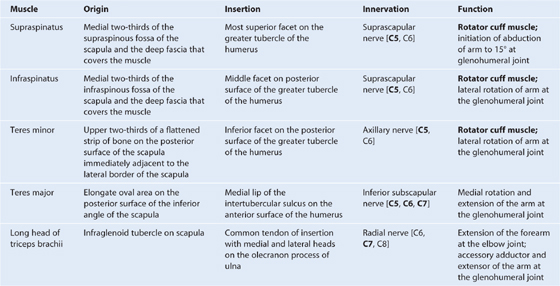
Fig. 7.25 Right posterior scapular region.
The posterior scapular region also contains part of one additional muscle, the long head of the triceps brachii, which passes between the scapula and the proximal end of the arm (Fig. 7.25). The importance of the triceps brachii in the posterior scapular region is that its vertical course between the teres minor and teres major, together with these muscles and the humerus, forms spaces through which nerves and vessels pass between regions.
The supraspinatus, infraspinatus, and teres minor muscles are three of the four components of the rotator cuff, which stabilizes the glenohumeral joint. The other component is subscapularis that is on the anterior aspect of the scapula.
Gateways to the posterior scapular region
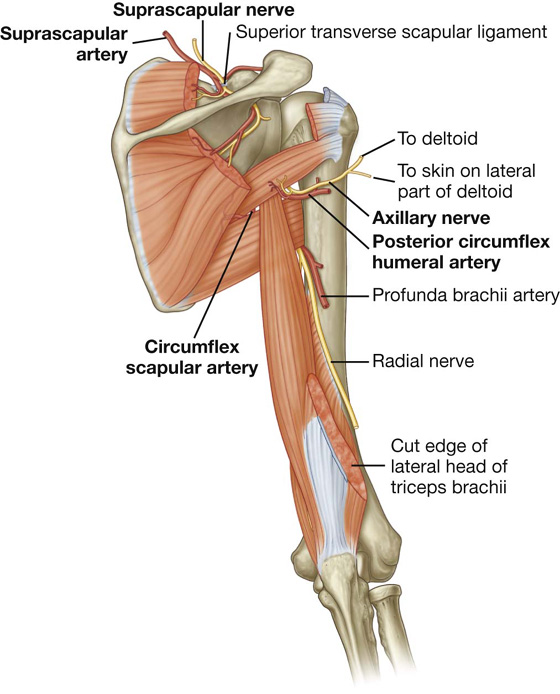
Suprascapular foramen
The suprascapular foramen is the route through which structures pass between the base of the neck and the posterior scapular region. It is formed by the suprascapular notch of the scapula and the superior transverse scapular (suprascapular) ligament, which converts the notch into a foramen (Fig. 7.26).
Fig. 7.26 Arteries and nerves associated with gateways in the posterior scapular region.
The suprascapular nerve passes through the suprascapular foramen; the suprascapular artery and the suprascapular vein follow the same course as the nerve, but normally pass immediately superior to the superior transverse scapular ligament and not through the foramen (Fig. 7.26).
Quadrangular space (from posterior)
The quadrangular space provides a passageway for nerves and vessels passing between more anterior regions (the axilla) and the posterior scapular region (Figs. 7.25, 7.26). In the posterior scapular region, its boundaries are formed by:
 the inferior margin of the teres minor,
the inferior margin of the teres minor,
 the surgical neck of the humerus,
the surgical neck of the humerus,
 the superior margin of the teres major, and
the superior margin of the teres major, and
 the lateral margin of the long head of triceps brachii.
the lateral margin of the long head of triceps brachii.
The axillary nerve and the posterior circumflex humeral artery and vein pass through this space (Fig. 7.26).
Clinical app
Quadrangular space syndrome
Hypertrophy of the muscles around the quadrangular space or fibrosis of the muscle edges may impinge on the axillary nerve. This may produce weakness of the deltoid muscle. It may also produce atrophy of the teres minor muscle, which may affect the control that the rotator cuff muscles exert on shoulder movement.
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (see Fig. 7.25). When viewed from the posterior scapular region, the triangular space is formed by:
 the medial margin of the long head of triceps brachii,
the medial margin of the long head of triceps brachii,
 the superior margin of the teres major, and
the superior margin of the teres major, and
 the inferior margin of the teres minor.
the inferior margin of the teres minor.
The circumflex scapular artery and vein pass through this gap (see Fig. 7.26).
Triangular interval
The triangular interval is formed by (see Fig. 7.25):
 the lateral margin of the long head of triceps brachii,
the lateral margin of the long head of triceps brachii,
 the inferior margin of the teres major.
the inferior margin of the teres major.
Because this space is below the inferior margin of the teres major, which defines the inferior boundary of the axilla, the triangular interval serves as a passageway between the anterior and posterior compartments of the arm and between the posterior compartment of the arm and the axilla. The radial nerve, the profunda brachii artery (deep artery of arm), and associated veins pass through it (see Fig. 7.26).
Nerves
The two major nerves of the posterior scapular region are the suprascapular and axillary nerves (see Fig. 7.25), both of which originate from the brachial plexus in the axilla.
Suprascapular nerve
The suprascapular nerve originates in the base of the neck from the superior trunk of the brachial plexus. It passes posterolaterally from its origin, through the suprascapular foramen to reach the posterior scapular region, where it lies in the plane between bone and muscle (see Fig. 7.26).
It innervates the supraspinatus muscle, then passes through the greater scapular (spinoglenoid) notch, between the root of the spine of the scapula and the glenoid cavity, to terminate in and innervate the infraspinatus muscle.
Generally, the suprascapular nerve has no cutaneous branches.
Axillary nerve
The axillary nerve originates from the posterior cord of the brachial plexus. It exits the axilla by passing through the quadrangular space in the posterior wall of the axilla, and enters the posterior scapular region (see Fig. 7.26). Together with the posterior circumflex humeral artery and vein, it is directly related to the posterior surface of the surgical neck of the humerus.
The axillary nerve innervates the deltoid and teres minor muscles. In addition, it has a cutaneous branch, the superior lateral cutaneous nerve of the arm, which carries general sensation from the skin over the inferior part of the deltoid muscle.
Arteries and veins
Three major arteries are found in the posterior scapular region: the suprascapular, posterior circumflex humeral, and circumflex scapular arteries. These arteries contribute to an interconnected vascular network around the scapula (Fig. 7.27).
Fig. 7.27 Arterial anastomoses around the shoulder.
Suprascapular artery
The suprascapular artery originates in the base of the neck as a branch of the thyrocervical trunk, which in turn, is a major branch of the subclavian artery (Fig. 7.27). The vessel may also originate directly from the third part of the subclavian artery.
The suprascapular artery normally enters the posterior scapular region superior to the suprascapular foramen, whereas the nerve passes through the foramen. In the posterior scapular region, the vessel runs with the suprascapular nerve (see Fig. 7.26).
In addition to supplying the supraspinatus and infraspinatus muscles, the suprascapular artery contributes branches to numerous structures along its course.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the third part of the axillary artery in the axilla (Figs. 7.26, 7.27).
The posterior circumflex humeral artery and axillary nerve leave the axilla through the quadrangular space in the posterior wall and enter the posterior scapular region. The vessel supplies the related muscles and the glenohumeral joint.
Circumflex scapular artery
The circumflex scapular artery is a branch of the subscapular artery that also originates from the third part of the axillary artery in the axilla (Fig. 7.27; also see Fig. 7.26). The circumflex scapular artery leaves the axilla through the triangular space and enters the posterior scapular region, passes through the origin of the teres minor muscle, and forms anastomotic connections with other arteries in the region.
Veins
Veins in the posterior scapular region generally follow the arteries and connect with vessels in the neck, back, arm, and axilla.
AXILLA
The axilla is the gateway to the upper limb, providing an area of transition between the neck and the arm (Fig. 7.28A). Formed by the clavicle, the scapula, the upper thoracic wall, the humerus, and related muscles, the axilla is an irregularly shaped pyramidal space with (Fig. 7.28A,B):
Fig. 7.28 Axilla. A. Walls and transition between neck and arm. B. Boundaries. C. Continuity with the arm.
The axillary inlet is continuous superiorly with the neck, and the lateral part of the floor opens into the arm.
All major structures passing into and out of the upper limb pass through the axilla (Fig. 7.28C). Apertures formed between muscles in the anterior and posterior walls enable structures to pass between the axilla and immediately adjacent regions (the posterior scapular, pectoral, and deltoid regions).
Axillary inlet
The axillary inlet is oriented in the horizontal plane and is somewhat triangular in shape, with its apex directed laterally (Fig. 7.28). The margins of the inlet are completely formed by bone:
 The medial margin is the lateral border of rib I.
The medial margin is the lateral border of rib I.
 The anterior margin is the posterior surface of the clavicle.
The anterior margin is the posterior surface of the clavicle.
 The posterior margin is the superior border of the scapula up to the coracoid process.
The posterior margin is the superior border of the scapula up to the coracoid process.
Major vessels and nerves pass between the neck and the axilla by crossing over the lateral border of rib I and through the axillary inlet (Fig. 7.28,A).
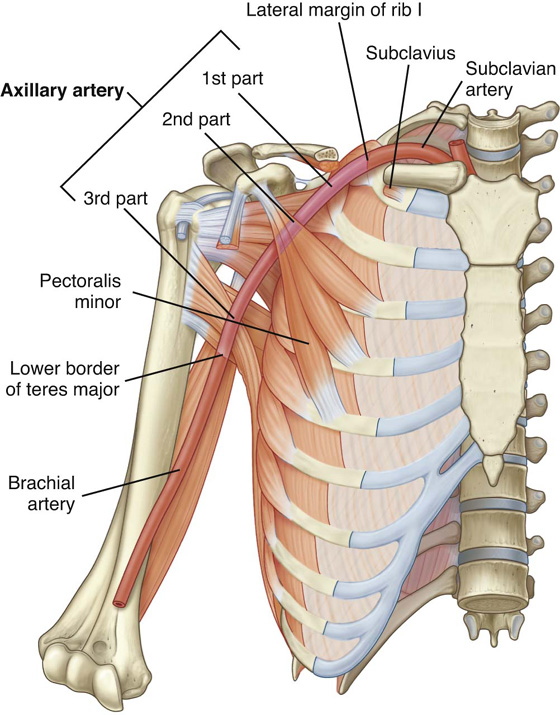
The subclavian artery, the major blood vessel supplying the upper limb, becomes the axillary artery as it crosses the lateral margin of rib I and enters the axilla. Similarly, the axillary vein becomes the subclavian vein as it passes over the lateral margin of rib I and leaves the axilla to enter the neck.
At the axillary inlet, the axillary vein is anterior to the axillary artery, which, in turn, is anterior to the trunks of the brachial plexus (Fig. 7.28,A)
The inferior trunk (lower trunk) of the brachial plexus lies directly on rib I in the neck, as does the subclavian artery and vein. As they pass over rib I, the vein and artery are separated by the insertion of the anterior scalene muscle (Fig. 7.28,A).
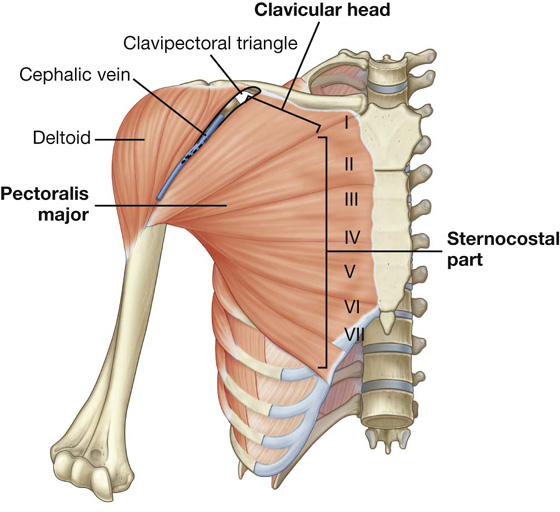
Anterior wall
The anterior wall of the axilla is formed by the lateral part of the pectoralis major muscle, the underlying pectoralis minor and subclavius muscles, and the clavipectoral fascia (Table 7.3, Figs. 7.28B, 7.29).
Table 7.3 Muscles of the anterior wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
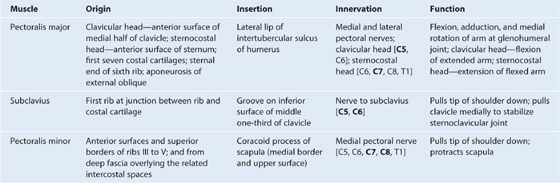
Fig. 7.29 Pectoralis major muscle.
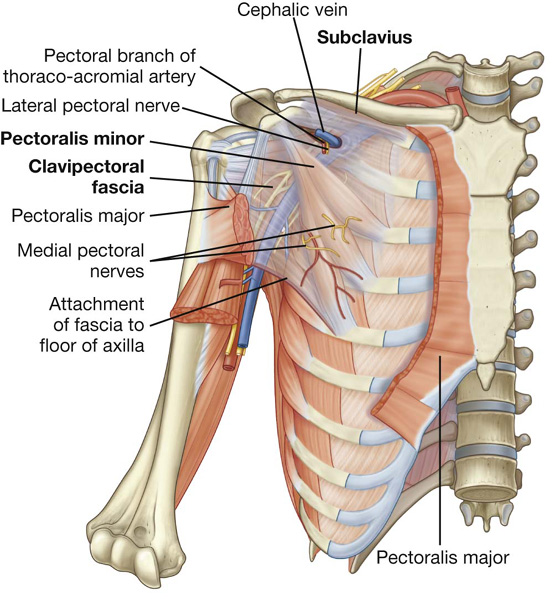
Clavipectoral fascia
The clavipectoral fascia is a thick sheet of connective tissue that connects the clavicle to the floor of the axilla (Fig. 7.30). It encloses the subclavius and pectoralis minor muscles and spans the gap between them.
Fig. 7.30 Pectoralis minor and subclavius muscles and clavipectoral fascia.
Structures travel between the axilla and the anterior wall of the axilla by passing through the clavipectoral fascia either between the pectoralis minor and subclavius muscles or inferior to the pectoralis minor muscle.
Important structures that pass between the subclavius and pectoralis minor muscles include the cephalic vein, the thoraco-acromial artery, and the lateral pectoral nerve.
The lateral thoracic artery leaves the axilla by passing through the fascia inferior to the pectoralis minor muscle.
The medial pectoral nerve leaves the axilla by penetrating directly through the pectoralis minor muscle to supply this muscle and to reach the pectoralis major muscle. Occasionally, branches of the medial pectoral nerve pass around the lower margin of the pectoralis minor to reach and innervate the overlying pectoralis major muscle.
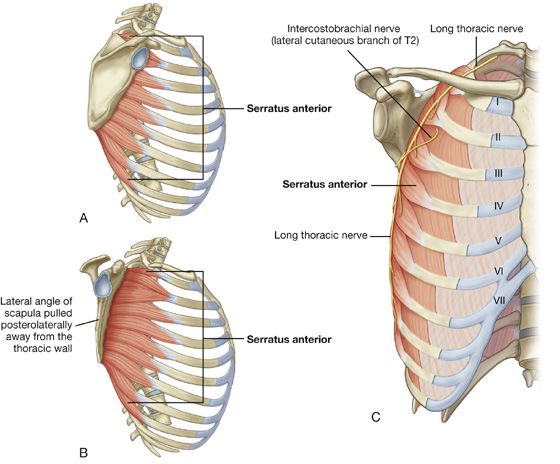
Medial wall
The medial wall of the axilla consists of the upper thoracic wall (the ribs and related intercostal tissues) and the serratus anterior muscle (Table 7.4, Fig. 7.31; see Fig. 7.28B).
Table 7.4 Muscles of the medial wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
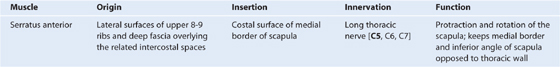
The only major structure that passes directly through the medial wall and into the axilla is the intercostobrachial nerve (Fig. 7.31C). This nerve is the lateral cutaneous branch of the second intercostal nerve (anterior ramus of T2). It communicates with a branch of the brachial plexus (the medial cutaneous nerve of the arm) in the axilla and supplies skin on the upper posteromedial side of the arm, which is part of the T2 dermatome.
Clinical app
“Winging” of the scapula
Because the long thoracic nerve passes down the lateral thoracic wall on the external surface of the serratus anterior muscle, just deep to skin and subcutaneous fascia, it is vulnerable to damage (see Fig. 7.31C). Loss of function of this muscle causes the medial border, and particularly the inferior angle, of the scapula to elevate away from the thoracic wall, resulting in characteristic “winging” of the scapula, on pushing forward with the arm. Furthermore, normal elevation of the arm is no longer possible.
Lateral wall
The lateral wall of the axilla is narrow and formed entirely by the intertubercular sulcus of the humerus (Fig. 7.32). The pectoralis major muscle of the anterior wall attaches to the lateral lip of the intertubercular sulcus. The latissimus dorsi and teres major muscles of the posterior wall attach to the floor and medial lip of the intertubercular sulcus, respectively (Table 7.5, Fig. 7.32).
Fig. 7.32 Lateral wall of the axilla.
Table 7.5 Muscles of the lateral and posterior wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle; spinal segments enclosed in parentheses do not consistently innervate the muscle)
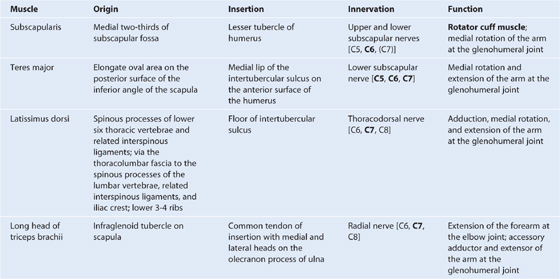
Posterior wall
The posterior wall of the axilla is complex (Table 7.5, Figs. 7.28B, 7.33). Its bone framework is formed by the costal surface of the scapula. Muscles of the wall are:
 the subscapularis muscle (associated with the costal surface of the scapula),
the subscapularis muscle (associated with the costal surface of the scapula),
 the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).
the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).
Fig. 7.33 Posterior wall of the axilla.
Gaps between the muscles of the posterior wall form apertures through which structures pass between the axilla, posterior scapular region, and posterior compartment of the arm (Fig. 7.33).
Together with three muscles of the posterior scapular region (the supraspinatus, infraspinatus, and teres minor muscles), the subscapularis is a member of the rotator cuff muscles, which stabilize the glenohumeral joint.
The long head of the triceps brachii muscle passes vertically through the posterior wall of the axilla, and, together with surrounding muscles and adjacent bones, results in the formation of three apertures through which major structures pass through the posterior wall (Fig. 7.33):
Gateways in the posterior wall
(See also “Gateways to the posterior scapular region,” p. 351, and Fig. 7.25.)
Quadrangular space
The quadrangular space provides a passageway for nerves and vessels passing between the axilla and the more posterior scapular and deltoid regions (Fig. 7.33). When viewed from anteriorly, its boundaries are formed by:
 the inferior margin of the subscapularis muscle;
the inferior margin of the subscapularis muscle;
 the surgical neck of the humerus;
the surgical neck of the humerus;
 the superior margin of the teres major muscle; and
the superior margin of the teres major muscle; and
 the lateral margin of the long head of the triceps brachii muscle.
the lateral margin of the long head of the triceps brachii muscle.
Passing through the quadrangular space are the axillary nerve and the posterior circumflex humeral artery and vein (see Fig. 7.26).
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (Fig. 7.33). When viewed from anteriorly, it is formed by:
 the medial margin of the long head of the triceps brachii muscle,
the medial margin of the long head of the triceps brachii muscle,
 the superior margin of the teres major muscle; and
the superior margin of the teres major muscle; and
 the inferior margin of the subscapularis muscle.
the inferior margin of the subscapularis muscle.
The circumflex scapular artery and vein pass into this space (see Fig. 7.26).
Triangular interval
This triangular interval is formed by (Fig. 7.33):
 the lateral margin of the long head of the triceps brachii muscle,
the lateral margin of the long head of the triceps brachii muscle,
 the inferior margin of the teres major muscle.
the inferior margin of the teres major muscle.
The radial nerve passes out of the axilla traveling through this interval to reach the posterior compartment of the arm (see Fig. 7.26).
Floor
The floor of the axilla (Fig. 7.34; also see Fig 7.28B) is formed by fascia and a dome of skin that spans the distance between the inferior margins of the walls. It is supported by the clavipectoral fascia.
Fig. 7.34 Floor of the axilla.
Inferiorly, structures pass into and out of the axilla immediately lateral to the floor where the anterior and posterior walls of the axilla converge and where the axilla is continuous with the anterior compartment of the arm.
Contents of the axilla
Passing through the axilla are the major vessels, nerves, and lymphatics of the upper limb. The space also contains the proximal parts of two muscles (biceps brachii and coracobrachialis muscles; Table 7.6) of the arm, the axillary process of the breast, and collections of lymph nodes, which drain the upper limb and chest wall.
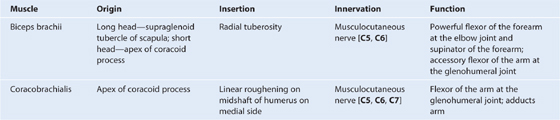
Table 7.6 Muscles having parts that pass through the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
Axillary artery
The axillary artery supplies the walls of the axilla and related regions, and continues as the major blood supply to the more distal parts of the upper limb (Fig. 7.35).
Fig. 7.35 Contents of the axilla: the axillary artery.
The subclavian artery in the neck becomes the axillary artery at the lateral margin of rib I and passes through the axilla, becoming the brachial artery at the inferior margin of the teres major muscle.
The axillary artery is separated into three parts by the pectoralis minor muscle, which crosses anteriorly to the vessel (Fig. 7.35):
 The first part is proximal to pectoralis minor.
The first part is proximal to pectoralis minor.
 The second part is posterior to pectoralis minor.
The second part is posterior to pectoralis minor.
 The third part is distal to pectoralis minor.
The third part is distal to pectoralis minor.
Generally, six branches arise from the axillary artery (Fig. 7.36):
 One branch, the superior thoracic artery, originates from the first part.
One branch, the superior thoracic artery, originates from the first part.
Fig. 7.36 Branches of the axillary artery.
Superior thoracic artery
The superior thoracic artery is small and originates from the anterior surface of the first part of the axillary artery (Fig. 7.36). It supplies upper regions of the medial and anterior axillary walls.
Thoracoacromial artery
The thoracoacromial artery is short and originates from the anterior surface of the second part of the axillary artery just posterior to the medial (superior) margin of the pectoralis minor muscle (Fig. 7.36). It curves around the superior margin of the muscle, penetrates the clavipectoral fascia, and immediately divides into four branches—the pectoral, deltoid, clavicular, and acromial branches, which supply the anterior axillary wall and related regions.
Additionally, the pectoral branch contributes vascular supply to the breast, and the deltoid branch passes into the clavipectoral triangle where it accompanies the cephalic vein and supplies adjacent structures (see Fig. 7.30).
Lateral thoracic artery
The lateral thoracic artery arises from the anterior surface of the second part of the axillary artery posterior to the lateral (inferior) margin of pectoralis minor (Fig. 7.36). It follows the margin of the muscle to the thoracic wall and supplies the medial and anterior walls of the axilla. In women, branches emerge from around the inferior margin of the pectoralis major muscle and contribute to the vascular supply of the breast.
Subscapular artery
The subscapular artery is the largest branch of the axillary artery and is the major blood supply to the posterior wall of the axilla (Fig. 7.36). It also contributes to the blood supply of the posterior scapular region.
The subscapular artery originates from the posterior surface of the third part of the axillary artery, follows the inferior margin of the subscapularis muscle for a short distance, then divides into its two terminal branches, the circumflex scapular artery and the thoracodorsal artery (Fig. 7.36).
The circumflex scapular artery passes through the triangular space between the subscapularis, teres major, and long head of the triceps muscles. Posteriorly, it passes inferior to, or pierces, the origin of the teres minor muscle to enter the infraspinous fossa. It anastomoses with the suprascapular artery and the deep branch (dorsal scapular artery) of the transverse cervical artery, thereby contributing to an anastomotic network of vessels around the scapula.
The thoracodorsal artery approximately follows the lateral border of the scapula to the inferior angle. It contributes to the vascular supply of the posterior and medial walls of the axilla.
Anterior circumflex humeral artery
The anterior circumflex humeral artery is small compared to the posterior circumflex humeral artery, and originates from the lateral side of the third part of the axillary artery (Fig. 7.36). It passes anterior to the surgical neck of the humerus and anastomoses with the posterior circumflex humeral artery.
This anterior circumflex humeral artery supplies branches to surrounding tissues, which include the glenohumeral joint and the head of the humerus.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the lateral surface of the third part of the axillary artery immediately posterior to the origin of the anterior circumflex humeral artery (Fig. 7.36). With the axillary nerve, it leaves the axilla by passing through the quadrangular space between the teres major, teres minor, and the long head of the triceps brachii muscle and the surgical neck of the humerus (see Fig. 7.26).
The posterior circumflex humeral artery curves around the surgical neck of the humerus and supplies the surrounding muscles and the glenohumeral joint. It anastomoses with the anterior circumflex humeral artery, and with branches from the profunda brachii, suprascapular, and thoracoacromial arteries.
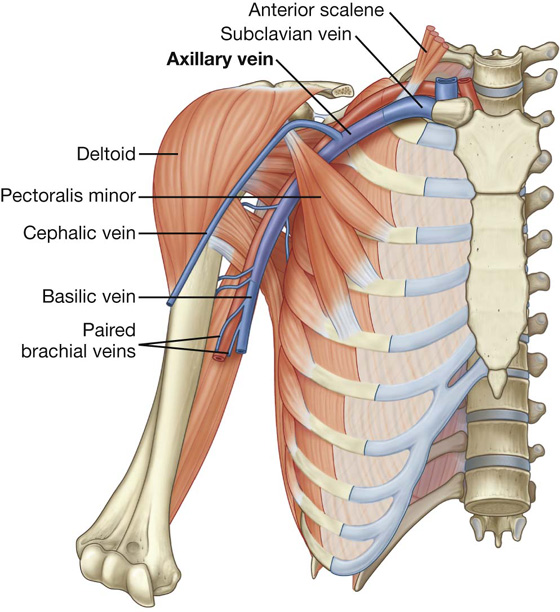
Axillary vein
The axillary vein begins at the lower margin of the teres major muscle and is the continuation of the basilic vein (Fig. 7.37), which is a superficial vein that drains the posteromedial surface of the hand and forearm and penetrates the deep fascia in the middle of the arm.
Fig. 7.37 Axillary vein.
The axillary vein passes through the axilla medial and anterior to the axillary artery and becomes the subclavian vein as the vessel crosses the lateral border of rib I at the axillary inlet. Tributaries of the axillary vein generally follow the branches of the axillary artery. Other tributaries include brachial veins that follow the brachial artery, and the cephalic vein (Fig. 7.37).
The cephalic vein is a superficial vein that drains the lateral and posterior parts of the hand, the forearm, and the arm. In the area of the shoulder, it passes into an inverted triangular cleft (the clavipectoral triangle) between the deltoid muscle, pectoralis major muscle, and the clavicle. In the superior part of the clavipectoral triangle, the cephalic vein passes deep to the clavicular head of the pectoralis major muscle and pierces the clavipectoral fascia to join the axillary vein.
Clinical app
Trauma to the arteries in and around the axilla
As the subclavian artery passes out of the neck and into the axilla, it is fixed in position by the surrounding muscles to the superior surface of rib I. A rapid deceleration injury involving upper thoracic trauma may cause a first rib fracture, which may significantly compromise the distal part of the subclavian artery or the first part of the axillary artery. Fortunately, there are anastomotic connections between branches of the subclavian artery and the axillary artery, which form a network around the scapula and proximal end of the humerus; therefore, even with complete vessel transection, the arm is rarely rendered completely ischemic (ischemia is poor blood supply to an organ or a limb).
Anterior dislocation of the humeral head
Anterior dislocation of the humeral head may compress the axillary artery resulting in vessel occlusion. This is unlikely to render the upper limb completely ischemic, but it may be necessary to surgically reconstruct the axillary artery to obtain pain-free function. Importantly, the axillary artery is intimately related to the brachial plexus, which also may be damaged at the time of anterior dislocation.
Clinical app
Central venous access via the subclavian/axillary vein
There are a number of routes through which central venous access may be obtained. The “subclavian route” and the “jugular route” are commonly used by clinicians. The subclavian route is a misnomer that remains the preferred term in clinical practice. In fact, most clinicians enter the first part of the axillary vein.
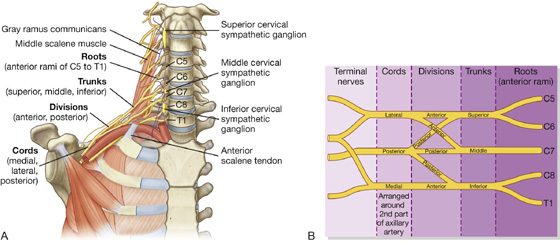
Brachial plexus
The brachial plexus is a somatic plexus formed by the anterior rami of C5 to C8, and most of the anterior ramus of T1 (Fig. 7.38). It originates in the neck, passes laterally and inferiorly over rib I, and enters the axilla.
The parts of the brachial plexus, from medial to lateral, are roots, trunks, divisions, and cords. All major nerves that innervate the upper limb originate from the brachial plexus, mostly from the cords. Proximal parts of the brachial plexus are posterior to the subclavian artery in the neck, while more distal regions of the plexus surround the axillary artery.
Roots
The roots of the brachial plexus are the anterior rami of C5 to C8, and most of T1. Close to their origin, the roots receive gray rami communicantes from the sympathetic trunk (Fig. 7.38). These carry postganglionic sympathetic fibers onto the roots for distribution to the periphery. The roots and trunks enter the posterior triangle of the neck by passing between the anterior scalene and middle scalene muscles and lie superior and posterior to the subclavian artery.
Trunks
The three trunks of the brachial plexus originate from the roots, pass laterally over rib I, and enter the axilla (Fig. 7.38):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 PT Case Studies
PT Case Studies Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases The shoulder is the area of upper limb attachment to the trunk. The bones of the shoulder include the scapula, clavicle, and proximal end of the humerus.
The shoulder is the area of upper limb attachment to the trunk. The bones of the shoulder include the scapula, clavicle, and proximal end of the humerus. The forearm is between the elbow joint and the wrist joint. The bones of the forearm are the ulna and radius.
The forearm is between the elbow joint and the wrist joint. The bones of the forearm are the ulna and radius. The hand is distal to the wrist joint. Bones of the hand are the carpals, metacarpals, and phalanges.
The hand is distal to the wrist joint. Bones of the hand are the carpals, metacarpals, and phalanges.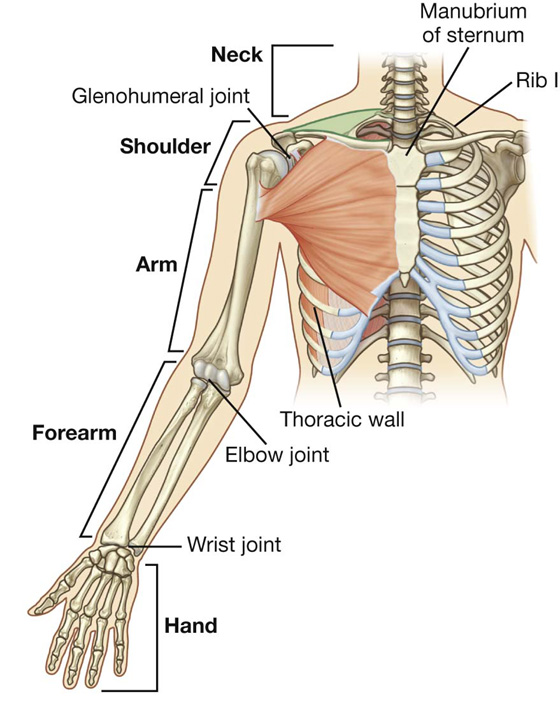
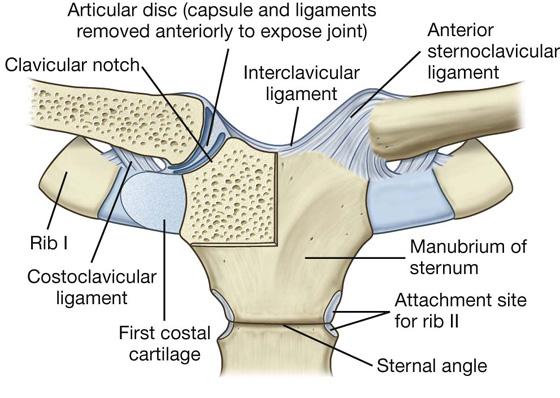
 The anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint.
The anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint. An interclavicular ligament links the ends of the two clavicles to each other and to the superior surface of the manubrium of sternum.
An interclavicular ligament links the ends of the two clavicles to each other and to the superior surface of the manubrium of sternum. The costoclavicular ligament is positioned laterally to the joint and links the proximal end of the clavicle to the first rib and related costal cartilage.
The costoclavicular ligament is positioned laterally to the joint and links the proximal end of the clavicle to the first rib and related costal cartilage.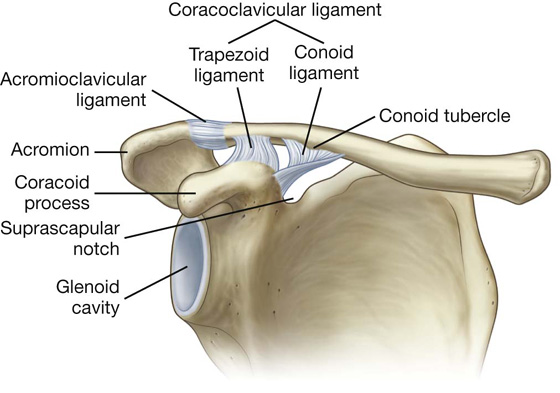
 a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and
a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weight-bearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion. It spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).
a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weight-bearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion. It spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).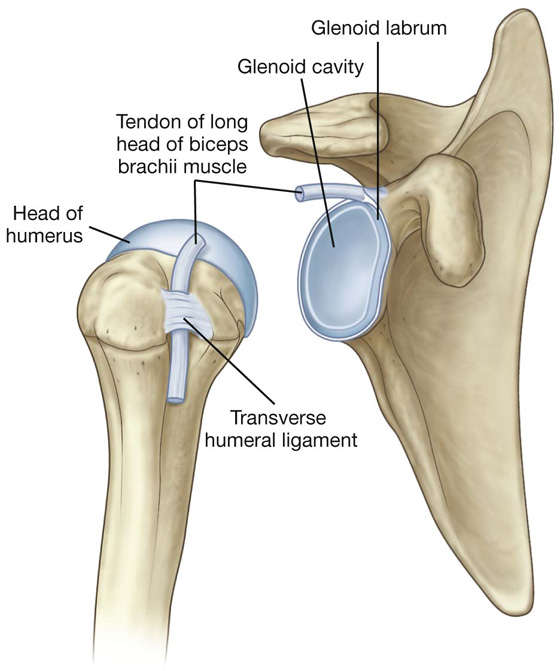
 in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles).
in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles). anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus;
anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus; superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament;
superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament; between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.
between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.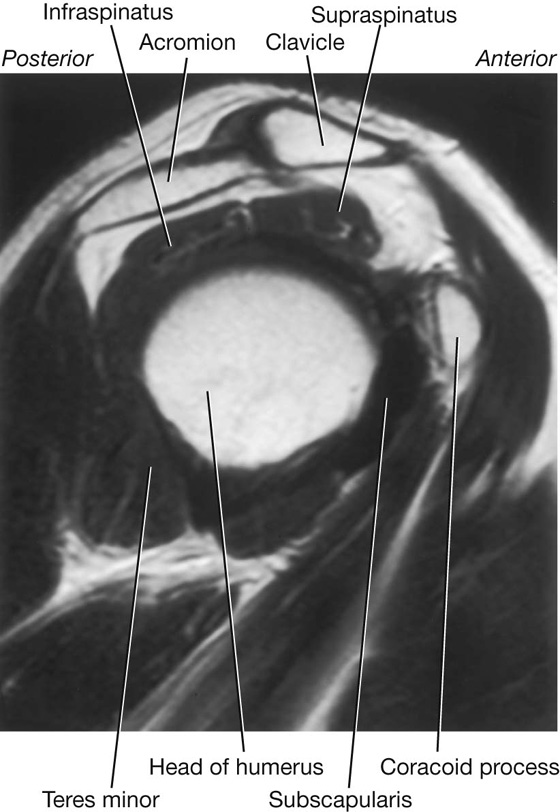
 the shaft of the humerus, and
the shaft of the humerus, and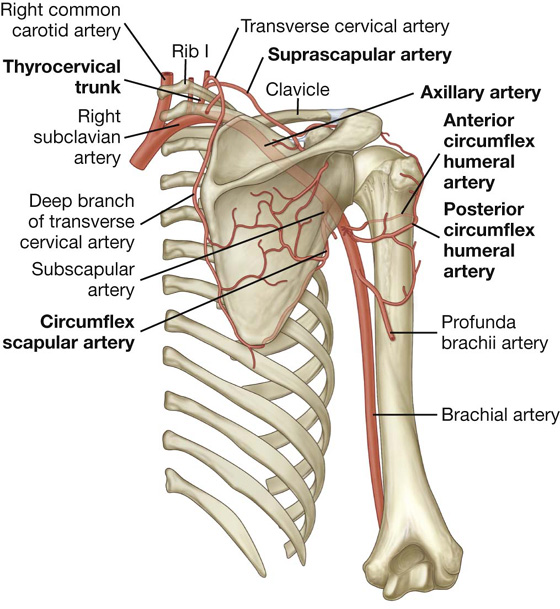
 four sides,
four sides, an inlet, and
an inlet, and a floor (base).
a floor (base).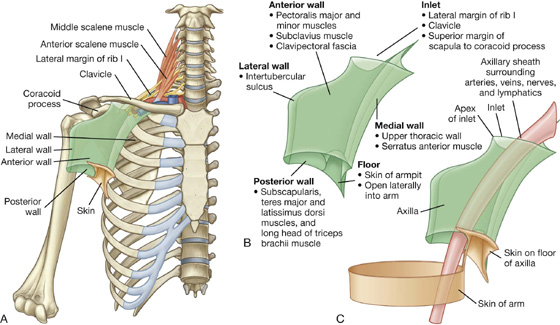
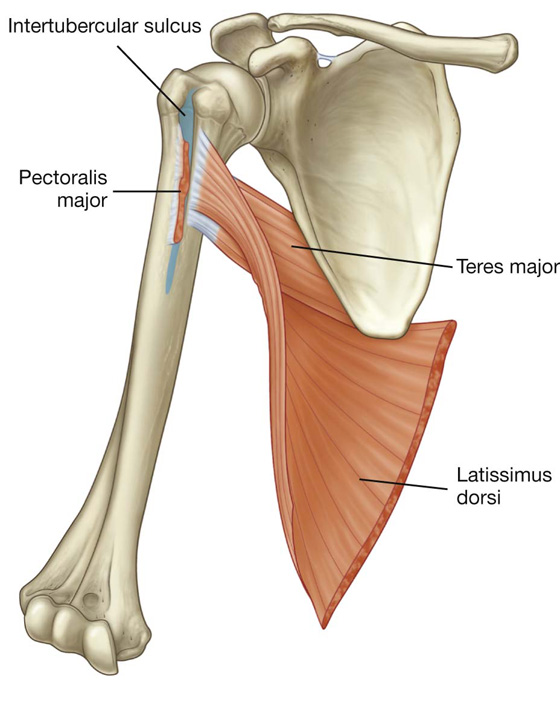
 the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region), and
the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region), and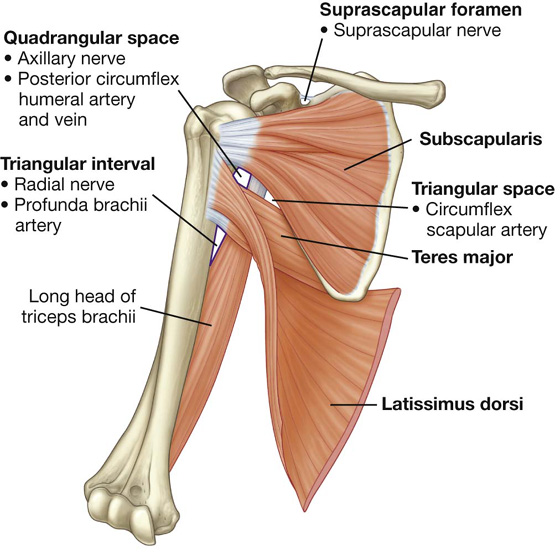
 the quadrangular space,
the quadrangular space, the triangular space, and
the triangular space, and the triangular interval.
the triangular interval. the shaft of the humerus, and
the shaft of the humerus, and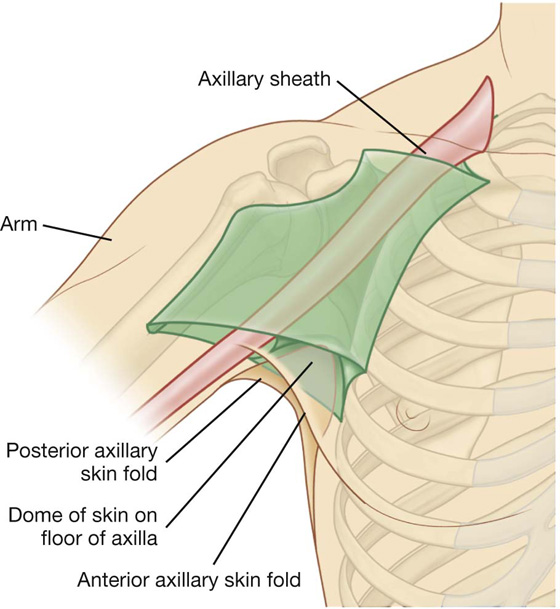
 Two branches, the thoracoacromial artery and the lateral thoracic artery, originate from the second part.
Two branches, the thoracoacromial artery and the lateral thoracic artery, originate from the second part. Three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part.
Three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part.