Bacillary Angiomatosis
Roberto N. Miranda, MD
Key Facts
Terminology
Nodules of small blood vessels resulting from infection by bacterium Bartonella henselae
Etiology/Pathogenesis
B. henselae and B. quintana are most common agents isolated from BA
Domestic cats are major reservoir for B. henselae; transmitted by fleas from cat to cat
Clinical Issues
Most affected patients are immunosuppressed (e.g., AIDS)
Cutaneous lesions can be 1 or many (up to hundreds)
Red to violaceous, dome-shaped papules and nodules
Lymphadenopathy may be regional or localized to area of trauma
Bacteria can be cultured from clinical specimens such as blood, tissues, or cytologic specimens
Microscopic Pathology
Blood vessels can show spectrum of differentiation
Interstitium shows edema, scattered spindle cells, neutrophils, or foamy histiocytes
Ancillary Tests
Warthin-Starry or Giemsa stain can highlight organisms
Monoclonal antibodies specific for B. henselae can identify bacterial organisms
PCR is helpful to identify organism
TERMINOLOGY
Abbreviations
Bacillary angiomatosis (BA)
Synonyms
Epithelioid angiomatosis
Definitions
Nodules of small blood vessels resulting from infection by bacterium Bartonella henselae
ETIOLOGY/PATHOGENESIS
Infectious Agents
Bartonella henselae is most common agent isolated from BA
Small, curved, motile, Gram-negative bacilli, oxidase-negative
Culture is difficult, and bacteria may take 2-6 weeks to grow
Growth requires CO2 rich environment and enriched media
Better yield in patients with systemic disease; poor yield from tissues
Isolates may be obtained in 40% of cases of BA and 6% of cases with cat scratch disease
Bartonella quintana, the agent of trench fever, also can cause BA
Bartonella enters endothelial cells by endocytosis
Gives rise to Bartonella-containing vacuoles or by invasome-mediated internalization
Invasome involves formation of cell surfaceassociated bacterial aggregates, which are engulfed
Bartonella effector protein A BepA and VirB/VirD4 type IV secretion system are associated with vascular sprout formation
Bartonella henselae is name adopted since 1993
Earlier name: Rochalimaea henselae
Susceptibility
B. henselae infections in patients with HIV infection can manifest as BA
HIV(+) homosexual patients, intravenous drug users, and transfusion recipients are at risk
Rarely, patients with other types of immunosuppression can develop BA
B. henselae infections in immunocompetent patients can result in cat scratch disease
Pathogenesis
Domestic cats are major reservoir for B. henselae
Transmitted by cat fleas from cat to cat
Up to 1/2 of domestic cats carry anti-Bartonella henselae antibodies
B. henselae causes bacteremia in cats; organism colonizes erythrocytes
Bacilli are transmitted to humans through bite or scratch of infested cat
B. quintana is unusual cause of BA
B. quintana is more frequently associated with “urban trench fever”
Trench fever is characterized by recurrent and cycling fevers, malaise, bone pain, and splenomegaly
Homeless persons exposed to human louse (Pediculus humanus corporis) are more susceptible to B. quintana
CLINICAL ISSUES
Epidemiology
Incidence
Most affected patients are immunosuppressed as result of HIV infection
BA is uncommon but can occur in patients with other types of immunosuppression
Very rare cases of BA occur in immunocompetent persons
Many patients are men; 31-56 years of age
In large part, this correlates with high percentage of HIV(+) men
Presentation
Although cats are major reservoir, history of cat exposure is a variable
It is common for affected patients to not have history of contact with cats
Cutaneous BA may show concomitant involvement of other sites
Mucous membranes, lymph nodes, soft tissues, spleen, liver, and bones
Cutaneous lesions: Single up to many (hundreds), red to violaceous, dome-shaped papules and nodules
Trunk and extremities are preferentially affected
Lymph node involvement is more frequently associated with B. henselae than with B. quintana
Lymphadenopathy may be regional or localized to area of trauma
Extracutaneous involvement can occur in absence of concurrent skin lesions
Laboratory Tests
No specific hematologic changes
Bacteria can be cultured from clinical specimens such as blood, tissues, or cytologic specimens
Treatment
Patients with BA can benefit from erythromycin or doxycycline
Hepatosplenic disease may benefit from trimethoprimsulfamethoxazole, gentamicin, ciprofloxacin, and rifampin
Prognosis
Most skin lesions resolve spontaneously
Early diagnosis of various affected organs leads to cure
Unrecognized progressive disease can be fatal
MICROSCOPIC PATHOLOGY
Histologic Features
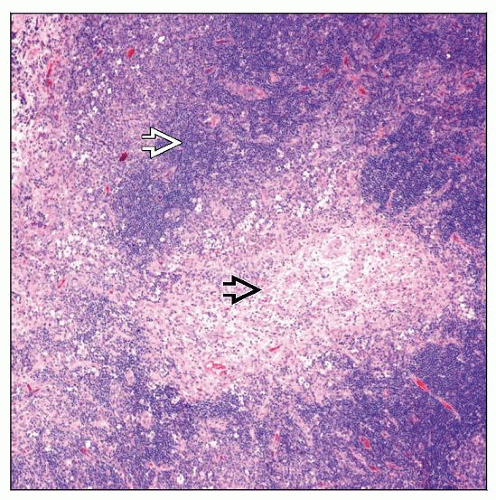
Lymph nodes involved by BA typically drain skin lesions
Nodules composed of blood vessels of variable size and shape
Vascular nodules can become confluent and form large masses
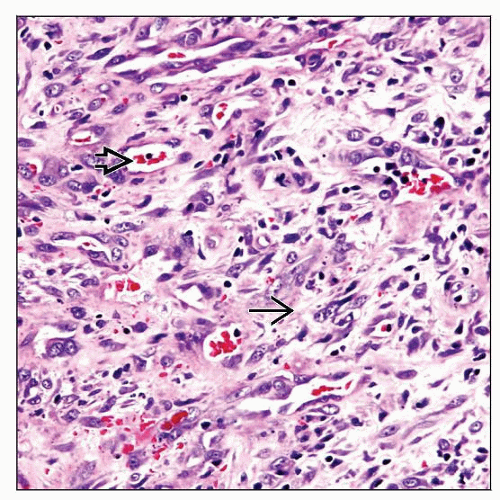
Blood vessels show a spectrum of differentiation
Round, large, irregular, or ectatic to small solid clusters with barely visible lumina
Endothelial nuclei are prominent, with single or multiple small nucleoli
Usually no multilayering of endothelial cells lining vessels
Mitotic figures are present; up to 3-5 per high-power field
Blood vessels can be surrounded by deeply eosinophilic interstitial material
Corresponds to bacterial aggregates
Interstitium may show loculated edema, scattered spindle cells, and inflammatory cells
Skin
Skin lesions can affect upper or deep dermis and subcutis
Lobules of newly formed blood vessels
Cytologically similar to those in lymph node
Overlying epidermis may be thin
Peliosis hepatis &/or peliosis splenis can occur
Cystic, blood-filled spaces in liver and spleen; can occur in immunocompromised patients
ANCILLARY TESTS
Histochemistry
Warthin-Starry (WS) stain highlights bacteria that appear as clumps of rods or as individual small rods
Bacteria can be found within endothelial cells or in macrophages
WS stain is technically difficult; skill is required to avoid precipitate that mimics bacterial organisms
Interpretation of good quality stain can be time consuming
Clusters of bacteria appear around blood vessels
Correspond to perivascular eosinophilic deposition seen on H&E stain
Giemsa stain may also highlight bacteria; appear violaceous
Immunohistochemistry
FVIIIRAg(+), ULEX-1(+)
Highlight endothelial cells
Reactivity correlates with degree of differentiation
CD31(+), CD34(+) in most cases
Monoclonal anti-B. henselae antibody reacts in fixed paraffin-embedded tissue; can confirm presence of bacteria
PCR
Primer sets specific for organism are available
Useful for identifying disease
Amplification of B. henselae 16S rRNA gene, citrate synthase gltA or htrA genes have been used
Sensitivity 45-75%; specificity near 100%
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree