Atypical Vascular Proliferation
Thomas Mentzel, MD
Key Facts
Terminology
Vascular proliferation after radiotherapy excluding obvious post-irradiation angiosarcoma, arising predominantly in breast
Clinical Issues
Exact incidence is difficult to establish
Occurs most frequently after radiation therapy of breast cancer
Small papules, usually less than 5 mm
Papules are red to brown colored
Often multifocal
All lesions must be excised completely
Wide age range; median in late 50s
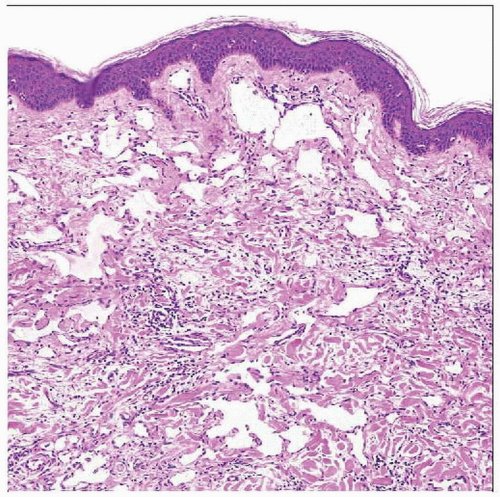
Microscopic Pathology
Rather well-circumscribed, superficially located, dermal lesions
Rather small, symmetrical, and wedge-shaped lesions
Dilated &/or narrow vascular structures
Sometimes anastomosing vessels are seen
Sometimes dissecting vascular structures are seen
Single layer of slightly enlarged endothelial cells
Expression of CD31 and podoplanin
No endothelial multilayering
No prominent cytologic atypia
No increased endothelial mitoses
No increased expression of Ki-67
No increased expression of p63
No amplification of c-myc
 Multiple red papules and nodules are seen in a patient with an atypical vascular proliferation after radiotherapy. |
TERMINOLOGY
Abbreviations
(Post-irradiation) atypical vascular proliferation (AVP)
Synonyms
Atypical vascular lesion (AVL)
Benign lymphangiomatous papulae (BLAP)
Definitions
Vascular proliferation after radiotherapy excluding obvious post-irradiation angiosarcoma, arising predominantly in breast
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Occurs after radiotherapy (40-60 Gy)
Develops after a median of 3 years after radiotherapy
CLINICAL ISSUES
Epidemiology
Incidence
Exact incidence difficult to establish
Relative risk is increased about 10x following radiation therapy
Incidence for post-irradiation AVP is equal after mastectomy or breast-conserving therapy
Age
Wide age range; median in late 50s
Usually 1 decade earlier than radiation-induced cutaneous angiosarcoma
Site
Occurs most frequently after radiation therapy for breast cancer
Seen in skin of breast &/or chest wall
Develops less frequently after radiation for gynecological or other malignancies
Presentation
Small, red to brown papules (usually less than 5 mm)
Often multifocal
Presents only rarely as large plaques
Treatment
Surgical approaches
All lesions must be excised completely
Prognosis
Very difficult to estimate exact prognosis
Presence of significant cytologic atypia worsens prognosis
Presence of increased proliferative activity (Ki-67) worsens prognosis
Presence of increased p53 expression worsens prognosis
MICROSCOPIC PATHOLOGY
Histologic Features
Rather well-circumscribed, superficially located, dermal lesions
Extension into subcutaneous tissue usually not seen
Rather small, symmetrical, and often wedge-shaped lesions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree