http://evolve.elsevier.com/McCuistion/pharmacology/
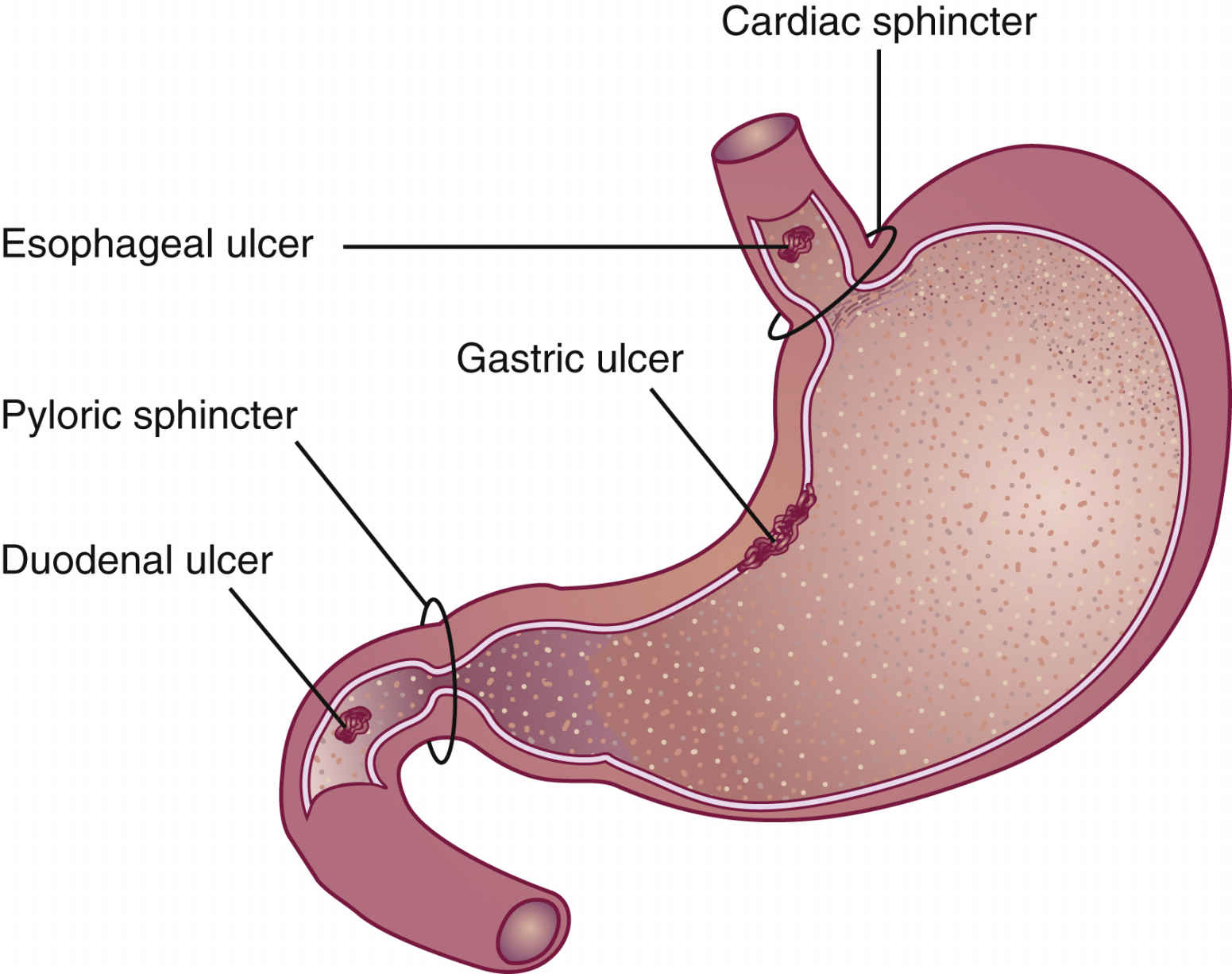
Peptic ulcer is a broad term for an ulcer that occurs in the esophagus, stomach, or duodenum within the upper gastrointestinal (GI) tract. Ulcers are more specifically named according to the site of involvement: esophageal, gastric, or duodenal. Duodenal ulcers occur 10 times more frequently than gastric and esophageal ulcers. The release of hydrochloric acid (HCl) from the parietal cells of the stomach is influenced by histamine, gastrin, and acetylcholine. Peptic ulcers occur when there is a hypersecretion of hydrochloric acid and pepsin, which erode the GI mucosal lining.
The gastric secretions in the stomach strive to maintain a pH of 2 to 5. Pepsin, a digestive enzyme, is activated at a pH of 2, and the acid-pepsin complex of gastric secretions can cause mucosal damage. If the pH of gastric secretions increases to 5, the activity of pepsin declines. The gastric mucosal barrier (GMB) is a thick, viscous, mucous material that provides a barrier between the mucosal lining and acidic gastric secretions. The GMB maintains the integrity of the gastric mucosal lining and is a defense against corrosive substances. The two sphincter muscles—the cardiac, located at the upper portion of the stomach, and the pyloric, located at the lower portion of the stomach—act as barriers to prevent reflux of acid into the esophagus and duodenum. Fig. 43.1 shows common sites of peptic ulcers.
An esophageal ulcer results from reflux of acidic gastric secretions into the esophagus as a result of a defective or incompetent cardiac sphincter. A gastric ulcer frequently occurs because of a breakdown of the GMB. A duodenal ulcer is caused by hypersecretion of acid from the stomach passing into the duodenum because of (1) insufficient buffers to neutralize gastric acid in the stomach, (2) a defective or incompetent pyloric sphincter, or (3) hypermotility of the stomach. Gastroesophageal reflux disease (GERD) is inflammation or erosion of the esophageal mucosa caused by a reflux of gastric acid content from the stomach into the esophagus.
Predisposing Factors in Peptic Ulcer Disease
The nurse needs to assist the patient in identifying possible causes of the ulcer and to teach ways to alleviate it. Predisposing factors include mechanical disturbances, genetic influences, bacterial organisms, environmental factors, and certain drugs. Healing of an ulcer takes 4 to 8 weeks. Complications can occur as the result of scar tissue. Table 43.1 lists the predisposing factors for peptic ulcers and their effects.
The classic symptom of peptic ulcers is gnawing, aching pain. With a gastric ulcer, pain occurs 30 minutes to 1.5 hours after eating, and with a duodenal ulcer, pain occurs 2 to 3 hours after eating. Small, frequent meals of nonirritating foods decrease the pain. With treatment, pain usually subsides in 10 days; however, the healing process may take 1 to 2 months.
A stress ulcer usually follows a critical situation such as extensive trauma, such as burns, or major surgery (e.g., cardiac surgery). Prophylactic use of antiulcer drugs decreases the incidence of stress ulcers.
Helicobacter pylori
Helicobacter pylori, a gram-negative bacillus, is linked with the development of peptic ulcer and is known to cause gastritis, gastric ulcer, and duodenal ulcer. When a peptic ulcer recurs after antiulcer therapy, and the ulcer is not caused by nonsteroidal antiinflammatory drugs (NSAIDs) such as aspirin or ibuprofen, the patient should be tested for the presence of H. pylori, which may have infected the gastric mucosa. In the past, endoscopy and a biopsy of the gastric antrum were needed to check for H. pylori. Currently, a noninvasive breath test—the Meretek UBT (urea breath test)—can detect H. pylori. This test consists of drinking a liquid containing 13C urea and breathing into a container. If H. pylori is present, the bacterial urease hydrolyzes the urea, releasing 13CO2, which is detected by a spectrometer. This test is 90% to 95% effective for detecting H. pylori and also notes progress in treatment. In addition, a blood test may be performed to check for antibodies to H. pylori, and a stool test may be done to check for antigens to determine whether the immune system has been triggered to fight H. pylori.
TABLE 43.1
Predisposing Factors for Peptic Ulcer Disease
| Predisposing Factors | Effects |
| Mechanical disturbances | Hypersecretion of acid and pepsin; inadequate GMB mucous secretion; impaired GMB resistance; hypermotility of the stomach; incompetent (defective) cardiac or pyloric sphincter |
| Genetic influences | Increased number of parietal cells in the stomach; susceptibility of mucosal lining to acid penetration; susceptibility to excess acetylcholine and histamine; excess hydrochloric acid caused by external stimuli |
| Environmental influences | Foods and liquids containing caffeine; fatty, fried, and highly spiced foods; alcohol; nicotine, especially from cigarette smoking; stressful situations; pregnancy; massive trauma; major surgery |
| Helicobacter pylori | A gram-negative bacterium, H. pylori, infects gastric mucosa and can cause gastritis, gastric ulcer, and duodenal ulcer. If not eradicated, peptic ulcer may return as frequently as every year. H. pylori can lead to atrophic gastritis in some patients. Serology and special breath tests can detect the presence of H. pylori. |
| Drugs | NSAIDs, including aspirin and aspirin compounds, ibuprofen, and indomethacin; corticosteroids; potassium salts; antineoplastic drugs |
There are various protocols for treating H. pylori infection, but antibacterial agents are the treatment of choice. The use of only one antibacterial agent is not effective for eradicating H. pylori because the bacterium can readily become resistant to that drug. Treatment to eradicate this bacterial infection includes using a dual-, triple-, or quadruple-drug therapy program in a variety of drug combinations—such as with amoxicillin, tetracycline, clarithromycin, omeprazole, lansoprazole, metronidazole, bismuth subsalicylate, or ranitidine bismuth citrate—on a 7- to 14-day treatment plan. The combination of drugs differs for each patient according to the patient’s drug tolerance. A common treatment protocol is the triple therapy of metronidazole (or amoxicillin), omeprazole (or lansoprazole), and clarithromycin (MOC). The drug regimen eradicates more than 90% of peptic ulcers caused by H. pylori (Complementary and Alternative Therapies 43.1).
One of the proton pump inhibitors (PPIs), such as omeprazole or lansoprazole, is frequently used as a component of combination drug therapy because each suppresses acid secretion by inhibiting the enzyme hydrogen or potassium adenosine triphosphatase (ATPase), which makes gastric acid. These agents block the final steps of acid production. If triple therapy fails to eradicate H. pylori, quadruple therapy using two antibiotics, a PPI, and a bismuth or histamine2 (H2) blocker is recommended. After completion of the treatment regimen, 6 weeks of standard acid suppression—such as H2 blocker therapy—is recommended. Table 43.2 lists agents used to treat H. pylori with their dosages, uses, and considerations.
Gastroesophageal Reflux Disease
Gastroesophageal reflux disease (GERD), also called reflux esophagitis, is an inflammation of the esophageal mucosa caused by reflux of gastric acid content into the esophagus. Its main cause is an incompetent lower esophageal sphincter. Smoking tends to accelerate the disease process.
Medical treatment for GERD is similar to the treatment for peptic ulcers. This includes use of the common antiulcer drugs to neutralize gastric contents and reduce gastric acid secretion. Drugs used in treatment include H2 blockers such as ranitidine and PPIs such as omeprazole, lansoprazole, rabeprazole, pantoprazole, or esomeprazole. A PPI relieves symptoms faster and maintains healing better than an H2 blocker. Once the strictures are relieved by dilation, they are less likely to recur if the patient was taking PPIs rather than an H2 blocker.
Effective management of GERD keeps the esophageal mucosa healed and the patient free from symptoms, but GERD is a chronic disorder that requires continuous care.
Nonpharmacologic Measures for Managing Peptic Ulcer and Gastroesophageal Reflux Disease
Nonpharmacologic measures, along with drug therapy, are an important part of treatment for a GI disorder. Once the GI problem is resolved, the patient should continue to follow nonpharmacologic measures to avoid recurrence of the condition.
Avoiding tobacco and alcohol can decrease gastric secretions. With GERD, nicotine relaxes the lower esophageal sphincter, permitting gastric acid reflux. Obesity enhances GERD, so weight loss is helpful in decreasing symptoms. The patient should avoid hot, spicy, and greasy foods, which could aggravate the gastric problem. Certain drugs like NSAIDs, which include aspirin, should be taken with food or in a decreased dosage. Glucocorticoids can cause gastric ulceration and should be taken with food.
To relieve symptoms of GERD, the patient should raise the head of the bed, not eat before bedtime, and wear loose-fitting clothing.
Antiulcer Drugs
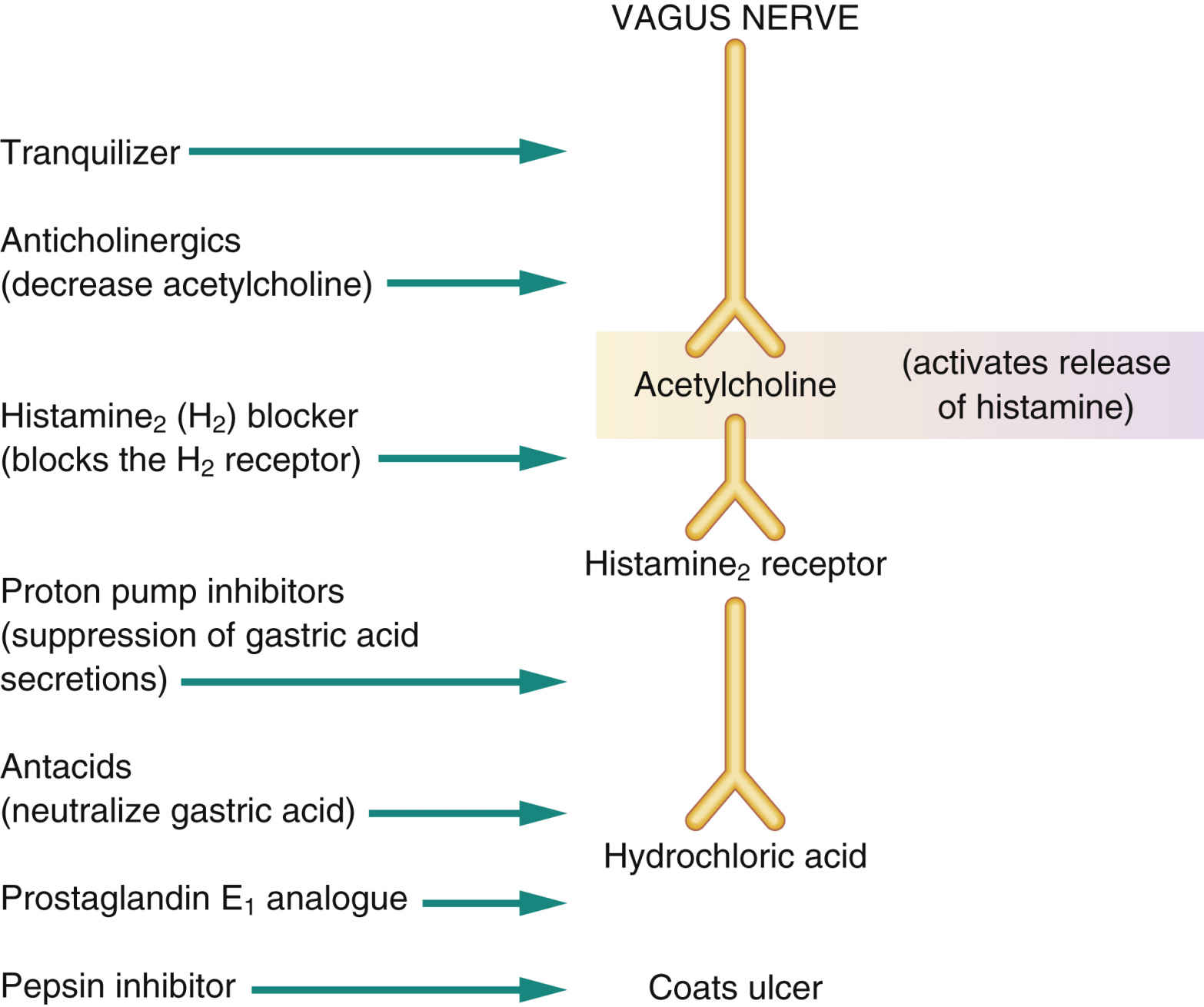
The seven groups of antiulcer agents are (1) tranquilizers, which decrease vagal activity; (2) anticholinergics, which decrease acetylcholine by blocking the cholinergic receptors; (3) antacids, which neutralize gastric acid; (4) H2 blockers, which block the H2 receptor; (5) PPIs, which inhibit gastric acid secretion, regardless of acetylcholine or histamine release; (6) the pepsin inhibitor sucralfate; and (7) the prostaglandin E1 analogue misoprostol, which inhibits gastric acid secretion and protects the mucosa. Currently, tranquilizers and anticholinergics are used infrequently due to potential adverse effects and much more effective drugs on the market. Fig. 43.2 shows the action of the antiulcer drug groups, each of which is discussed separately.
Tranquilizers
Tranquilizers have minimal effect in preventing and treating ulcers; however, they reduce vagal stimulation and decrease anxiety. A combination of the anxiolytic chlordiazepoxide and the anticholinergic clidinium bromide may be used in the treatment of ulcers. Adverse effects may include edema, ataxia, confusion, extrapyramidal syndrome (EPS), and agranulocytosis.
TABLE 43.3
Antiulcer Drugs: Anticholinergics
| Drug | Route and Dosage | Uses and Considerations |
| Clidinium bromide and chlordiazepoxide hydrochloride | Ulcer: A: PO: 1-2 cap (clidinium 2.5 mg, chlordiazepoxide 5 mg) tid/qid ac and at bedtime; max: clidinium 20 mg/d, chlordiazepoxide 40 mg/d Older A: PO: 1 cap bid; max: clidinium 20 mg/d, chlordiazepoxide 40 mg/d | For treatment of gastric ulcer, IBS, and enterocolitis. May cause drowsiness, confusion, dry mouth, blurred vision, nausea, constipation, edema, and ataxia. Pregnancy category: D∗; PB: 96%; t½: 2.4-20 h |
| Glycopyrrolate | Ulcer: A/adol/C >12 y: PO: 1-2 mg bid/tid; max: 6 mg/d A/adol >16 y: IM/IV: 100-200 mcg q4h as needed; max: 6 mg/d | For gastric and duodenal ulcers, bradycardia, and aspiration prophylaxis. May cause dry mouth, blurred vision, headache, flushing, anhidrosis, palpitations, seizures, erectile dysfunction, urinary retention, and constipation. Pregnancy category: B∗; PB: UK; t½: 0.5-3 h |
| Propantheline | A: PO: 15 mg tid 30 min ac and 30 mg at bedtime Older A: PO: 7.5 mg bid/tid ac | For duodenal ulcers. May cause headache, dizziness, blurred vision, confusion, palpitations, hypotension, anhidrosis, urinary retention, dysphagia, and constipation. Pregnancy category: C∗; PB: UK; t½: 1.6 h |
Anticholinergics
Anticholinergics (antimuscarinics, parasympatholytics) and antacids were the drugs of choice for peptic ulcers for many years. However, anticholinergic use declined with the introduction of H2 blockers in 1975. These drugs relieve pain by decreasing GI motility and secretion. They act by inhibiting acetylcholine and blocking histamine and hydrochloric acid. Anticholinergics delay gastric emptying time, so they are used more frequently for duodenal ulcers than for gastric ulcers. The anticholinergic propantheline bromide inhibits gastric secretions in the treatment of peptic ulcers.
Anticholinergics should be taken before meals to decrease the acid secretion that occurs with eating. Antacids can slow the absorption of anticholinergics and therefore should be taken 2 hours after anticholinergic administration.
Table 43.3 lists selected anticholinergic drugs used to treat peptic ulcer. Anticholinergics should be used as adjunctive therapy and not as the only antiulcer drug. Anticholinergics are discussed in more detail in Chapter 16.
Side Effects and Adverse Reactions
Anticholinergics have many side effects, including dry mouth, decreased secretions, headache, blurred vision, drowsiness, dizziness, lethargy, palpitations, bradycardia, tachycardia, urinary retention, and constipation. Because anticholinergics decrease GI motility, gastric emptying time is delayed, which can stimulate gastric secretions and aggravate the ulceration.
Antacids
Antacids promote ulcer healing by neutralizing hydrochloric acid and reducing pepsin activity; they do not coat the ulcer. There are two types of antacids: those that have a systemic effect and those that have a nonsystemic effect.
Sodium bicarbonate, a systemically absorbed antacid, was one of the first antiulcer drugs. Because it has many side effects (sodium excess, causing hypernatremia and water retention; metabolic alkalosis caused by excess bicarbonate; and acid rebound [excess acid secretion]), sodium bicarbonate is seldom used to treat peptic ulcers.
Calcium carbonate is most effective in neutralizing acid; however, one third to one half of the drug can be systemically absorbed and can cause acid rebound. Hypercalcemia and Burnett syndrome, formerly called milk-alkali syndrome, can result from excessive use of calcium carbonate. Burnett syndrome is intensified if milk products are ingested with calcium carbonate. It is identified by the presence of alkalosis, hypercalcemia, and in severe cases, by crystalluria and renal failure.
The nonsystemic antacids are composed of alkaline salts such as aluminum (aluminum hydroxide) and magnesium (magnesium hydroxide, magnesium trisilicate). A small degree of systemic absorption occurs with these drugs, mainly of aluminum. Magnesium hydroxide has greater neutralizing power than aluminum hydroxide. Magnesium compounds can cause diarrhea, and aluminum and calcium compounds can cause constipation with long-term use. A combination of magnesium and aluminum salts neutralizes gastric acid without causing severe diarrhea or constipation. Simethicone, an antigas agent, is found in many antacids. Prototype Drug Chart 43.1 lists the pharmacologic data for aluminum hydroxide antacids.
Pharmacokinetics
Aluminum hydroxide was one of the first antacids used to neutralize hydrochloric acid. Aluminum products are frequently used to lower high serum phosphate (hyperphosphatemia). Because aluminum hydroxide alone can cause constipation, and magnesium products alone can cause diarrhea, combination drugs such as aluminum hydroxide and magnesium hydroxide have become popular because they decrease these side effects.
Only a small amount of aluminum hydroxide is absorbed from the GI tract. It is primarily bound to phosphate and excreted in the feces. The small portion that is absorbed is excreted in the urine.
Pharmacodynamics
Aluminum hydroxide neutralizes gastric acid, including hydrochloric acid, and increases the pH of gastric secretions; an elevated pH inactivates pepsin. The onset of action is fairly rapid, but the duration of action varies, depending on whether the antacid is taken with or without food. If the antacid is taken after a meal, the duration of action may be up to 3 hours because food delays gastric emptying time. Frequent dosing may be necessary if the antacid is given during a fasting state or early in the course of treatment.
The ideal dosing interval for antacids is 1 and 3 hours after meals (maximum acid secretion occurs after eating) and at bedtime. Antacids taken on an empty stomach are effective for 30 to 60 minutes before passing into the duodenum. Chewable tablets should be followed by water. Liquid antacids should also be taken with water (2 to 4 oz) to ensure that the drug reaches the stomach; however, no more than 4 ounces of water should be taken because water quickens gastric emptying time.
Antacids that contain magnesium salts are contraindicated in patients with impaired renal function because of the risk for hypermagnesemia. Magnesium is primarily excreted by the kidneys; however, hypermagnesemia is usually not a problem unless a patient with renal insufficiency is ingesting magnesium. Prolonged use of aluminum hydroxides can cause hypophosphatemia (low serum phosphate), osteoporosis, nephrolithiasis, and osteomalacia. If hyperphosphatemia occurs because of poor renal function, aluminum hydroxide can be given to decrease the phosphate level. In patients with renal insufficiency, aluminum salt ingestion can cause encephalopathy from accumulation of aluminum in the brain. Table 43.4 lists the antacids and their dosages, uses, and considerations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree