DRUG CLASSES
Beta (β)-adrenergic blocking drugs
Alpha (α)/β and antiadrenergic drugs (centrally and peripherally acting)
Calcium channel blocking drugs
Angiotensin-converting enzyme inhibitors (ACEIs)
Angiotensin II receptor antagonists
PHARMACOLOGY IN PRACTICE

Mr. Alfredo Garcia was in a month ago for a respiratory infection. At that time his blood pressure was 210/120 mm Hg. He was prescribed a beta (β) blocking drug. When he returns today, his weight is down 15 lb and his blood pressure is 170/95 mm Hg. Read about the different drugs in this chapter to see if any changes should be made.
In the United States, about 72 million people have high blood pressure; this is about 1 in 3 adults. African Americans are twice as likely as whites to experience hypertension. After age 65, African American women have the highest incidence of hypertension. Hypertension as defined as a blood pressure of 140/90 mm Hg or higher.
What is meant by blood pressure? It is simply the force of the blood against the walls of the arteries. Blood pressure increases and decreases throughout the day. The condition in which blood pressure stays elevated over time is known as hypertension. A systolic blood pressure less than 120 mm Hg and a diastolic blood pressure less than 80 mm Hg (120/80) are considered normal. Prehypertension is defined as a systolic pressure between 120 and 139 mm Hg or a diastolic pressure between 80 and 89 mm Hg. Individuals with prehypertensive blood pressures are at risk for developing hypertension and should begin health-promoting lifestyle modifications.
Risks Factors for Hypertension
Hypertension is serious, because it causes the heart to work too hard and contributes to atherosclerosis. It also increases the risk of heart disease, heart failure (HF), kidney disease, blindness, and stroke. Yet, most cases of hypertension have no known cause and this is called primary hypertension. Although the cause may be unknown, certain risk factors, such as diet and lifestyle, can influence primary hypertension. Display 35.1 identifies the risk factors associated with hypertension.
Primary hypertension cannot be cured but it can be controlled. Although hypertension is not a part of healthy aging, many individuals experience hypertension as they grow older. For many older individuals, the systolic pressure gives the most accurate diagnosis of hypertension. Display 35.2 discusses the importance of the systolic pressure.
Nonpharmacologic Management for Hypertension
Once primary hypertension develops, management of the disorder becomes a lifetime task. When a direct cause of the hypertension can be identified, the condition is described as secondary hypertension. Among the known causes of secondary hypertension kidney disease ranks first, with tumors or other abnormalities of the adrenal glands following. Most primary health care providers prescribe lifestyle changes to reduce risk factors before prescribing drugs. The primary health care provider may recommend measures such as:
Display 35.1 Risk Factors for Hypertension
- Age and sex (women older than 55 years and men older than 45 years of age)
- African American race (higher rates than Asian, Caucasian, or Hispanic individuals)
- Obesity
- Excessive dietary intake of salt and too little intake of potassium
- Chronic alcohol consumption
- Lack of physical activity
- Cigarette smoking
- Family history of high blood pressure and/or cardiovascular disease, diabetes, persistent stress
- Overweight in youth younger than 18 years has become a risk factor for prehypertension in teens
Display 35.2 Importance of the Systolic Blood Pressure
Individuals with only an elevated systolic pressure have a condition known as isolated systolic hypertension (ISH). In ISH, systolic blood pressure is 140 mm Hg or greater with diastolic blood pressure less than 90 mm Hg. When the systolic pressure is high, blood vessels become less flexible and stiffen, leading to cardiovascular disease and kidney damage. Research indicates that treating ISH saves lives and reduces illness. The treatment is the same for ISH as for other forms of hypertension. Diastolic pressure should not be reduced lower than 70 mm Hg. Therefore, caution is advised in treating those with ISH and existing heart disease (JNC 7, 2009).
• Weight loss (if the patient is overweight)
• Stress reduction (e.g., relaxation techniques, meditation, and yoga)
• Regular aerobic exercise
• Smoking cessation (if applicable)
• Moderation of alcohol consumption
• Dietary changes, such as a decrease in sodium (salt) intake
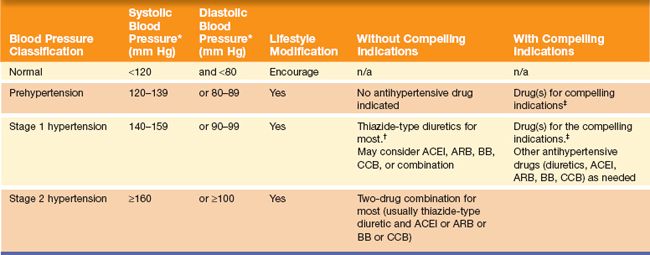
Many people with hypertension are “salt sensitive,” in that any salt or sodium more than the minimum need is too much for them and leads to an increase in blood pressure. Dietitians usually recommend the Dietary Approaches to Stop Hypertension (DASH) diet. Studies indicate that blood pressure can be reduced by eating a diet low in saturated fat, total fat, and cholesterol and rich in fruits, vegetables, and low-fat dairy foods. The DASH diet includes whole grains, poultry, fish, and nuts and has reduced amounts of fats, red meats, sweets, and sugared beverages. Table 35.1 identifies current blood pressure classifications and management strategies for adults.
Drug Therapy for Hypertension
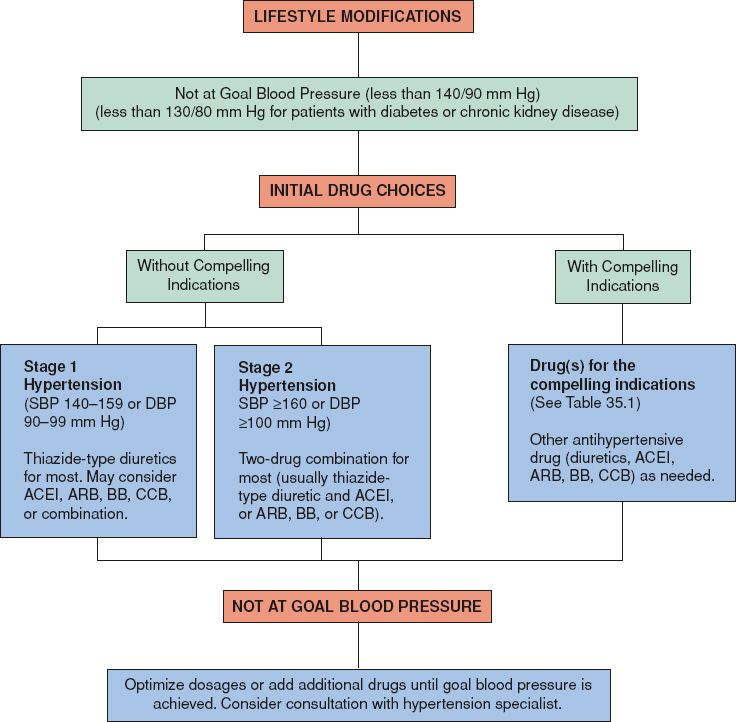
When nonpharmacologic measures do not control high blood pressure, drug therapy usually begins, and the primary health care provider may first prescribe a diuretic (see Chapter 33) or beta (β)-adrenergic blocker (see Chapter 25), because these drugs typically are highly effective. However, as in many other diseases and conditions, there is no “best” single drug, drug combination, or medical regimen for treatment of hypertension. After examination and evaluation of the patient, the primary health care provider selects the antihypertensive drug and therapeutic regimen that will probably be most effective. Figure 35.1 illustrates the recommendations of the National Heart, Lung and Blood Institute’s seventh report on hypertension displayed as an algorithm for the treatment of hypertension.
Drug abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β blocker; CCB, calcium channel blocker.
* Treatment determined by highest BP category.
† Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension.
‡ Treat patients with chronic kidney disease or diabetes to BP goal of <130/80 mm Hg.
Adapted from National Heart, Lung and Blood Institute. (2003). The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Institutes of Health. Retrieved May 7, 2009, from http://www.nhlbi.nih.gov/guidelines/hypertension/.
When the patient does not experience a response to therapy, it may be necessary to change to another antihypertensive drug or add a second antihypertensive drug. The primary health care provider also recommends that the patient continue with stress reduction, dietary modifications, and other lifestyle modifications needed for controlling hypertension. The types of drugs used for the treatment of hypertension include the following:
• Diuretics—for example, furosemide and hydrochlorothiazide
• β-Adrenergic blocking drugs—for example, atenolol and propranolol
• Antiadrenergic drugs (centrally acting)—for example, clonidine and methyldopa
• Antiadrenergic drugs (peripherally acting)—for example, doxazosin and prazosin
• Calcium channel blocking drugs—for example, amlodipine and diltiazem
• Angiotensin-converting enzyme inhibitors—for example, captopril and enalapril
• Angiotensin II receptor antagonists—for example, irbesartan and losartan
• Vasodilating drugs—for example, hydralazine and minoxidil
Two drug types are relatively new—direct renin inhibitors (aliskiren) and selective aldosterone receptor antagonists (SARAs; eplerenone). Aliskiren inhibits renin and subsequently prevents the angiotensin conversion process. Eplerenone also blocks the angiotensin process by binding with aldosterone.
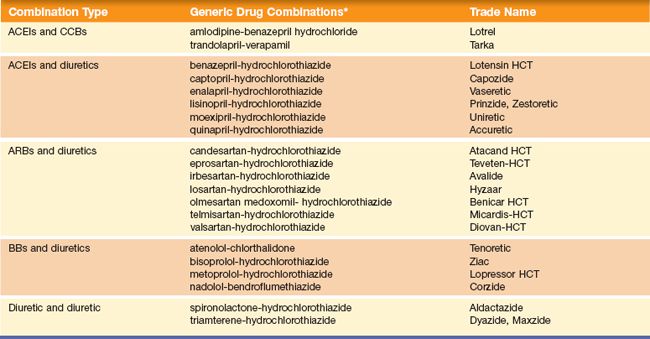
For additional information concerning the antiadrenergic drugs (both centrally and peripherally acting), and the alpha (α)- and β-adrenergic blocking drugs, see Chapter 25. Information on the vasodilating drugs and the diuretics can be found in Chapters 36 and 33, respectively. In addition to these antihypertensive drugs, many antihypertensive combinations are available, such as Capozide, Timolide, Aldoril, and Lopressor HCT (Table 35.2). Most combination antihypertensive drugs combine antihypertensive and diuretic agents.
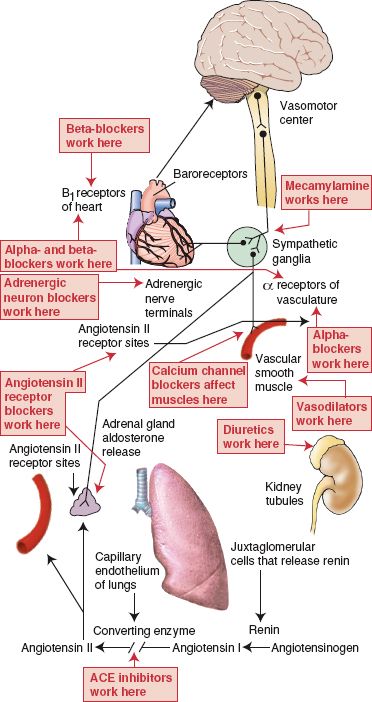
Actions
Many antihypertensive drugs lower the blood pressure by dilating or increasing the size of the arterial blood vessels (vasodilation). Vasodilation creates an increase in the lumen (the space or opening within a blood vessel) of the arterial blood vessels, which in turn increases the amount of space available for the blood to circulate. Because blood volume (the amount of blood) remains relatively constant, an increase in the space in which the blood circulates (i.e., the blood vessels) lowers the pressure of the fluid (measured as blood pressure) in the blood vessels. Although the method by which antihypertensive drugs dilate blood vessels varies, the result remains basically the same. Figure 35.2 shows the organs affected by the different classes of antihypertensive drugs.
Antihypertensive drugs with vasodilating activity include the adrenergic blocking and calcium channel blocking drugs. Diuretics (Chapter 33) are also considered antihypertensive drugs. The mechanism by which the diuretics reduce elevated blood pressure is not completely understood, but it is thought to be based, in part, on their ability to increase the excretion of sodium from the body.
Figure 35.1 Algorithm for treatment of hypertension. Compelling indicators include HF, high risk for cardiovascular disease, post–myocardial infarction (MI), diabetes, stroke prevention, and chronic kidney disease. Key: DBP, diastolic blood pressure; SBP, systolic blood pressure; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β blocker; CCB, calcium channel blocker; DBP, diastolic blood pressure; SBP, systolic blood pressure. (Adapted from National Heart, Lung and Blood Institute. [2003]. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Institutes of Health. Retrieved May 7, 2009, from http://www.nhlbi.nih.gov/guidelines/ hypertension/.)
Drug abbreviations: BB, β blocker; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
* Some drug combinations are available in multiple fixed doses. Each drug dose is reported in milligrams.
Adapted from National Heart Lung and Blood Institute. (2003). The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Institutes of Health. Retrieved May 7, 2009, from http://www.nhlbi.nih.gov/guidelines/hypertension/.
Action of Angiotensin-Converting Enzyme Inhibitors
The angiotensin-converting enzyme (ACE) inhibitors (ACEIs) appear to act primarily through suppression of the renin-angiotensin-aldosterone system. These drugs prevent (or inhibit) the activity of ACE, which converts angiotensin I to angiotensin II, a powerful vasoconstrictor. Both angiotensin I and ACE normally are manufactured by the body and are called endogenous substances. The vasoconstricting activity of angiotensin II stimulates the secretion of the endogenous hormone aldosterone by the adrenal cortex. Aldosterone promotes the retention of sodium and water, which may contribute to a rise in blood pressure. By preventing the conversion of angiotensin I to angiotensin II, this chain of events is interrupted, sodium and water are not retained, and blood pressure decreases.
Action of Calcium Channel Blockers
Systemic and coronary arteries are influenced by movement of calcium across cell membranes of vascular smooth muscle. The contractions of cardiac and vascular smooth muscle depend on movement of extracellular calcium ions into these walls through specific ion channels.
Calcium channel blockers act by inhibiting the movement of calcium ions across cell membranes of cardiac and arterial muscle cells. This results in less calcium available for the transmission of nerve impulses. As a result, these drugs relax blood vessels, increase the supply of oxygen to the heart, and reduce the heart’s workload.
Action of Angiotensin II Receptor Antagonists
These drugs act to block the binding of angiotensin II at various receptor sites in the vascular smooth muscle and adrenal gland, which blocks the vasoconstrictive effect of the renin-angiotensin system and the release of aldosterone, resulting in a lowering of the blood pressure.
Uses
Antihypertensive drugs are used in the treatment of hypertension. Although many antihypertensive drugs are available, not all drugs work equally well for a given patient. In some instances, the primary health care provider may find it necessary to prescribe a different antihypertensive drug when the patient does not experience a response to therapy. Some antihypertensive drugs are used only in severe cases of hypertension and when other, less potent drugs fail to lower the blood pressure. At times, two antihypertensive drugs may be given together to achieve a better response (see Fig. 35.1).
Nitroprusside (Nitropress) is an example of an intravenous (IV) drug that may be used to treat hypertensive emergencies. A hypertensive emergency is a case of extremely high blood pressure in which blood pressure must be lowered immediately to prevent damage to the target organs. Target organs of hypertension include the heart, kidney, and eyes (retinopathy). Additional uses of the antihypertensive drugs are given in the Summary Drug Table: Antihypertensive Drugs.
Adverse Reactions
When any antihypertensive drug is given, orthostatic (or postural) hypotension may result in some patients, especially early in therapy. Orthostatic hypotension occurs when the individual has a significant drop in blood pressure (usually 10 mm Hg systolic or more) when assuming an upright position. The patient can become dizzy and may fall, resulting in an injury. Butt (2012) reported that the risk of hip fracture is increased by almost 50% for those older than 66 when they are started on antihypertensives. This is thought to be from fainting and falling related to orthostatic hypotension.
Central Nervous System Reactions
• Fatigue, depression, dizziness, headache, and syncope
Respiratory System Reactions
• Upper respiratory infections and cough
Gastrointestinal System Reactions
• Abdominal pain, nausea, diarrhea, constipation, gastric irritation, and anorexia
Other Reactions
• Rash, pruritus, dry mouth, tachycardia, hypotension, proteinuria, and neutropenia
Additional adverse reactions that may occur when an antihypertensive drug is administered are listed in the Summary Drug Table: Antihypertensive Drugs. For the adverse reactions that may result when a diuretic is used as an antihypertensive drug, see the Summary Drug Table: Diuretics in Chapter 33.
Contraindications
Antihypertensive drugs are contraindicated in patients with known hypersensitivity to the individual drugs.
The ACEIs and angiotensin II receptor blockers are contraindicated if the patient has impaired renal function, HF, salt or volume depletion, bilateral stenosis, or angioedema. They are also contraindicated during pregnancy (pregnancy category C during first trimester and pregnancy category D in the second and third trimesters) or during lactation. Use of the ACEIs and the angiotensin II receptor blockers during the second and third trimesters of pregnancy is contraindicated, because use may cause fetal and neonatal injury or death.
Calcium channel blockers are contraindicated in patients who are hypersensitive to the drugs and those with sick sinus syndrome, second- or third-degree atrioventricular (AV) block (except with a functioning pacemaker), hypotension (systolic pressure less than 90 mm Hg), ventricular dysfunction, or cardiogenic shock.
Precautions
Antihypertensive drugs are used cautiously in patients with renal or hepatic impairment or electrolyte imbalances, during lactation and pregnancy, and in older patients. The calcium channel blockers are used cautiously in patients with HF or renal or hepatic impairment. The calcium channel blockers are used cautiously during pregnancy (pregnancy category C) and lactation. ACEIs are used cautiously in patients with sodium depletion, hypovolemia, or coronary or cerebrovascular insufficiency and in those receiving diuretic therapy or dialysis. The angiotensin II receptor agonists are used cautiously in patients with renal or hepatic dysfunction, hypovolemia, or volume or salt depletion, and in patients receiving high doses of diuretics.
Interactions
The hypotensive effects of most antihypertensive drugs are increased when administered with diuretics and other antihypertensives. Many drugs can interact with the antihypertensive drugs and decrease their effectiveness (e.g., monoamine oxidase inhibitor antidepressants, antihistamines, and sympathomimetic bronchodilators).
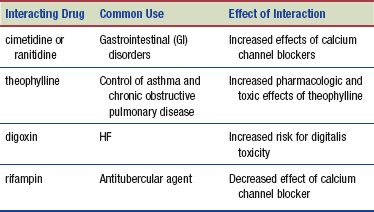
The following interactions may occur when the calcium channel blockers are used with another agent:
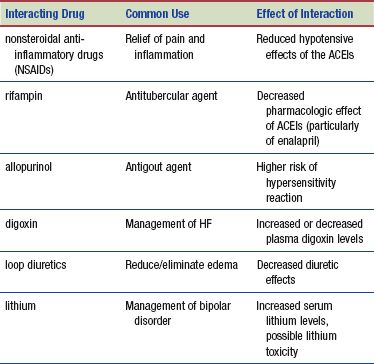
The following interactions may occur when ACEI drugs are administered with another agent:
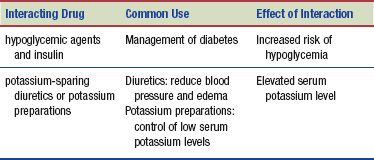
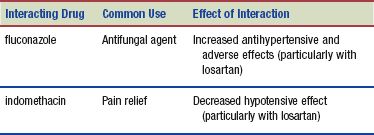
The following interactions may occur when angiotensin II receptor antagonists are administered with other agents:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Hawthorn, one of the most commonly used natural agents to treat various cardiovascular problems such as hypertension, angina, arrhythmias, and HF, is known for its masses of white, strong-smelling flowers. They are used, along with the fruit and leaves of the plant, in the form of capsules, fluid extract, tea, tinctures, and topical creams. Hawthorn should not be taken by individuals who are pregnant, breastfeeding, or allergic to the agent. Possible adverse reactions include hypotension, arrhythmias, sedation, nausea, and anorexia. Possible drug–hawthorn interactions include a risk of hypotension when hawthorn is used with other antihypertensive drugs, possible increased effects of inotropic drugs when inotropic drugs are administered with hawthorn, and increased risk of sedative effects when hawthorn is administered with other central nervous system (CNS) depressants. As with all substances, hawthorn should be used only under the supervision of the primary health care provider (DerMarderosian, 2003).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree