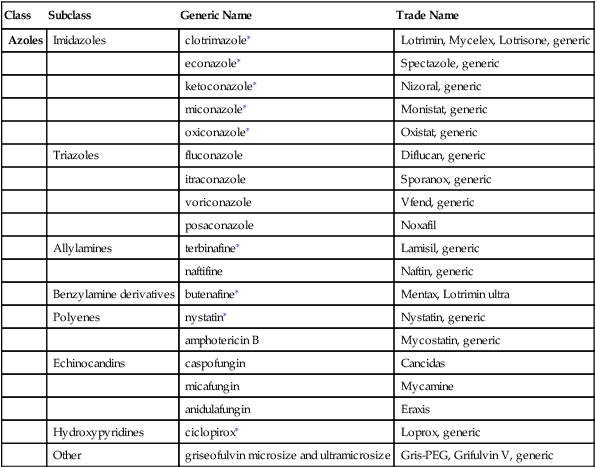
Chapter 67 ∗Covered in Chapter 13, Dermatologic Agents. A growing number of antifungals are now available for topical or oral use. This chapter discusses the oral antifungals most commonly used in the primary care treatment of two types of fungal infection: (1) endemic fungal infection, such as blastomycosis, histoplasmosis, and sporotrichosis, and (2) superficial fungal infection not responsive to topical therapy. Fluconazole is commonly used for vulvovaginal candidiasis. Chapter 13 discusses the treatment of superficial fungal infections with topical antifungal agents. Several of the newer antifungals are administered parenterally and are used in specialty practice; these are not discussed here. Ketoconazole and itraconazole have “black box” warnings—itraconazole for CHF and 3A4 drug interactions, and ketoconazole for hepatotoxicity and 3A4 drug interactions. Fungal infections of the nails remain prevalent, and the demand for treatment has increased as safer drugs have been developed. A factor that limits this treatment is the refusal of many health insurance companies to reimburse for these medications, which are expensive and must be used for an extended period. Infections of the nails are generally impervious to superficial treatment. Ciclopirox (Penlac) is a new topical medication that is effective for skin and nail infections; however, it is expensive (see Chapter 13). Candida albicans is part of the normal flora of the mouth, vagina, and feces of most people. Overgrowth of candida organisms causes mucosal candidiasis, which may affect the mouth, esophagus, and vulvovagina. It is also frequently found on the skin, especially in skin folds. Vulvovaginal candida is discussed in Chapter 58. Topical candida is discussed in Chapter 13. Risk factors for invasive candidiasis (i.e., fungemia and endocarditis) include neutropenia, recent surgery, broad-spectrum antibiotic therapy, indwelling catheters (IV or bladder), and immunodeficiency. HIV infection should be suspected if the patient has invasive candidiasis. Terbinafine blocks the biosynthesis of ergosterol, an essential component of fungal cell membranes. Griseofulvin is derived from a species of Penicillium. It is deposited in the keratin of diseased tissue, making it resistant to fungal infection. The diseased tissue is gradually exfoliated and is replaced by noninfected tissue. See Table 67-1 for a comparison of the mechanisms of action of commonly used antifungals. TABLE 67-1 Classification and Mechanism of Action of Selected Antifungal Antibiotics Modified from Zhang AY et al: Advances in topical and systemic antifungals, Dermatol Clin 25:165-183, 2007. The Infectious Diseases Society of America has put forth guidelines for the treatment of patients with aspergillus, blastomycosis, coccidioidomycosis or cryptococcal disease, candidiasis, histoplasmosis, and sporotrichosis (www.idsociety.org). • Topical fungi are often resistant to oral treatment; in order of effectiveness, treatment may consist of terbinafine, itraconazole, or fluconazole. • Endemic fungal infections: In order of effectiveness, itraconazole and fluconazole • Culture or microscopy should be performed whenever possible to confirm a diagnosis of fungal infection. A wide variety of tests are available, including the following: • Potassium hydroxide preparation (KOH), interpreted by both a dermatologist (KOH-CLINIC) and a laboratory technician (KOH-LAB) • KOH with dimethyl sulfoxide (KOH-DMSO); when combined with chlorazol black E (KOH-CBE), interpreted by a dermatologist • Culture with dermatophyte test medium or with mycobiotic and inhibitory mold agar (Cx) • Histopathologic analysis with the use of periodic acid–Schiff stain (PAS)
Antifungals
Class
Subclass
Generic Name
Trade Name
Azoles
Imidazoles
clotrimazole∗
Lotrimin, Mycelex, Lotrisone, generic
econazole∗
Spectazole, generic
ketoconazole∗
Nizoral, generic
miconazole∗
Monistat, generic
oxiconazole∗
Oxistat, generic
Triazoles
fluconazole
Diflucan, generic
itraconazole
Sporanox, generic
voriconazole
Vfend, generic
posaconazole
Noxafil
Allylamines
terbinafine∗
Lamisil, generic
naftifine
Naftin, generic
Benzylamine derivatives
butenafine∗
Mentax, Lotrimin ultra
Polyenes
nystatin∗
Nystatin, generic
amphotericin B
Mycostatin, generic
Echinocandins
caspofungin
Cancidas
micafungin
Mycamine
anidulafungin
Eraxis
Hydroxypyridines
ciclopirox∗
Loprox, generic
Other
griseofulvin microsize and ultramicrosize
Gris-PEG, Grifulvin V, generic
Therapeutic Overview
Anatomy and Physiology
Disease Process
Topical Fungi
Mechanism of Action
Class
Representative Drugs
Mechanism of Action and Antifungal Effects
Azoles
clotrimazole
Inhibition of fungal lanosterol 14-α demethylase, resulting in depletion of ergosterol and accumulation of toxic sterols in the fungal cell membrane; fungistatic
Triazoles
voriconazole
Candida: Time-dependent fungistatic
Aspergillus: Time-dependent slow fungicidal
Polyenes
nystatin
Interaction with ergosterol, formation of aqueous channels, increased membrane permeability, and subsequent leakage of intracellular components; fungistatic and fungicidal properties
amphotericin B
Fungicidal
Hydroxypyridine
ciclopirox
Inhibition of essential enzymes by creation of a large polyvalent cation through chelation, thus interfering with mitochondrial electron transport processes and energy production; fungicidal and fungistatic properties
Other antifungals
griseofulvin
Inhibition of fungal cell mitosis and nucleic acid synthesis and interference with the function of spindles and cytoplasmic microtubules by binding to α- and β-tubulin; fungistatic
Treatment Principles
Standardized Guidelines
Cardinal Points of Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antifungals
Only gold members can continue reading. Log In or Register to continue
