DRUG CLASSES
Antifungals
Antihelmintics
Antiprotozoals
Fungal Infections
A fungus is a single-celled, colorless plant that lacks chlorophyll (Fig. 12.1). Fungi that cause disease in humans may be yeast-like or mold-like; the resulting infections are called fungal or mycotic infections.
Fungal infections range from superficial skin infections to life-threatening systemic infections. The superficial mycotic infections occur on the surface of, or just below, the skin or nails (see Chapter 52). Systemic fungal infections are serious infections that occur when fungi gain entrance into the interior of the body. These deep mycotic infections develop inside the body in sites such as in the lungs, brain, or gastrointestinal (GI) tract. Treatment for deep mycotic infections is often difficult and prolonged.
PHARMACOLOGY IN PRACTICE

Lillian Chase, age 36, is caring for her two grandchildren. She calls the clinic because she thinks they are unusually fussy this visit. In asking about the children, there does not seem to be any indication they are ill; what you do learn is that they typically play in a large sand lot at home. Think about questions to ask about the children as you read this chapter.
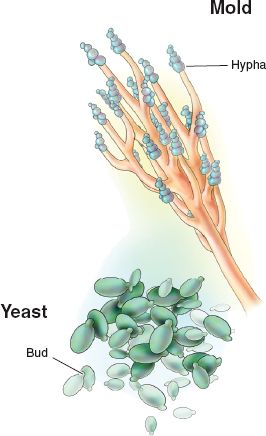
Figure 12.1 Examples of infection-causing fungi.
Yeast infections, such as those caused by Candida albicans, are known as candidiasis. Infection of the mouth by the microorganism C. albicans is commonly called thrush. Candidiasis also affects women in the vulvovaginal area and immunocompromised patients with chronic conditions in the perineum, the oral cavity, or systemically. Patients who are at increased risk for candidal infections are those who have diabetes, are pregnant, or are taking oral contraceptives, antibiotics, or corticosteroids such as posttransplant or surgical patients. The Summary Drug Table: Antifungal and Antiparasitic Drugs identifies drugs that are used to combat fungal infections.
ANTIFUNGAL DRUGS
Actions
Antifungal drugs may be fungicidal (able to destroy fungi) or fungistatic (able to slow or retard the multiplication of fungi). Amphotericin B (Fungizone IV), miconazole (Monistat), nystatin, voriconazole (Vfend), micafungin (Mycamine), and ketoconazole (Nizoral) are thought to have an effect on the cell membrane of the fungus. The fungicidal or fungistatic effect of these drugs appears to be related to their concentration in body tissues. Fluconazole (Diflucan) has fungistatic activity that appears to result from the depletion of sterols (a group of substances related to fats) in the fungus cells.
Griseofulvin (Grisactin) exerts its effect by being deposited in keratin precursor cells, which are then gradually lost (because of the constant shedding of top skin cells) and replaced by new, noninfected cells. The mode of action of flucytosine (Ancobon) is to inhibit DNA and RNA synthesis in the fungus. Clotrimazole (Lotrimin, Mycelex) binds with phospholipids in the fungal cell membrane, increasing permeability of the cell and resulting in loss of intracellular components.
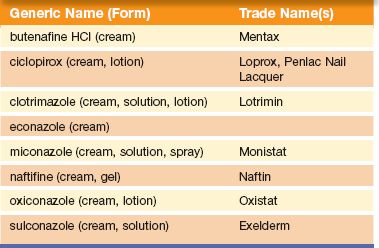
Table 12.1 Topical Antifungal Drugs
Uses
Antifungal drugs are used prophylactically to prevent or to treat fungal infection in immunocompromised patients. They are also used to treat the following:
• Superficial and deep fungal infections
• Systemic infections such as aspergillosis, candidiasis, and cryptococcal meningitis
• Superficial infections of nail beds and oral, anal, and vaginal areas
The specific uses of antifungal drugs appear in the Summary Drug Table: Antifungal and Antiparasitic Drugs. Miconazole is an antifungal drug used to treat vulvovaginal “yeast” infections and is representative of all the vaginal antifungal agents. Fungal infections of the skin or mucous membranes may be treated with topical or vaginal preparations. A listing of the topical antifungal drugs appears in Table 12.1, and the vulvovaginal antifungal agents are listed in Table 12.2.
Table 12.2 Vaginal Antifungal Drugs
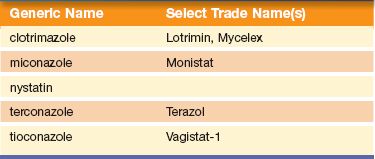
Table 12.3 Possible Interactions Between Antifungal and Other Drugs
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Researchers have identified several antifungal herbs that are effective against skin infections, such as tea tree oil (Melaleuca alternifolia) and garlic (Allium sativum). Tea tree oil comes from an evergreen tree native to Australia. The herb has been used as a nonirritating antimicrobial for cuts, stings, wounds, burns, and acne. It can be found in shampoos, soaps, and lotions. Tea tree oil should not be ingested orally but is effective when used topically for minor cuts and stings. Topical application is most effective when used in a cream with at least 10% tea tree oil. Several commercially prepared ointments are available. The cream is applied to affected areas twice daily for several weeks.
Garlic is also used as an antifungal. A cream of 0.4% ajoene (the antifungal component of garlic) was found to relieve symptoms of athlete’s foot and, like tea tree oil, is applied twice daily (DerMarderosian, 2003).
Adverse Reactions
Systemic Administration
• Headache
• Rash
• Anorexia and malaise
• Abdominal, joint, or muscle pain
• Nausea, vomiting, diarrhea
Contraindications
Antifungal drugs are contraindicated in patients with a history of allergy to the drug. Most of the systemic antifungal medications are contraindicated during pregnancy and lactation and are used only when the situation is life-threatening and outweighs the risk to the fetus.
Griseofulvin is not recommended for those with severe liver disease. Voriconazole is contraindicated when patients are taking the following medications: terfenadine, astemizole, sirolimus, rifampin, rifabutin, carbamazepine, ritonavir, ergot alkaloids, or long-acting barbiturates.
Both voriconazole and itraconazole are contraindicated in patients taking cisapride, pimozide, or quinidine. The systemic agent itraconazole should not be used to treat fungal nail infections in patients with a history of heart failure.
Precautions
Antifungals should be used cautiously in patients with renal dysfunction or hepatic impairment. Specific precautions include:
• Use amphotericin B cautiously in patients who have electrolyte imbalances or who currently use antineoplastic drugs (because severe bone marrow suppression can result).
• Administer griseofulvin cautiously with penicillin because of possible cross-sensitivity.
• Itraconazole should be used with caution in patients with human immunodeficiency virus (HIV) infection or hypochlorhydria (low levels of stomach acid).
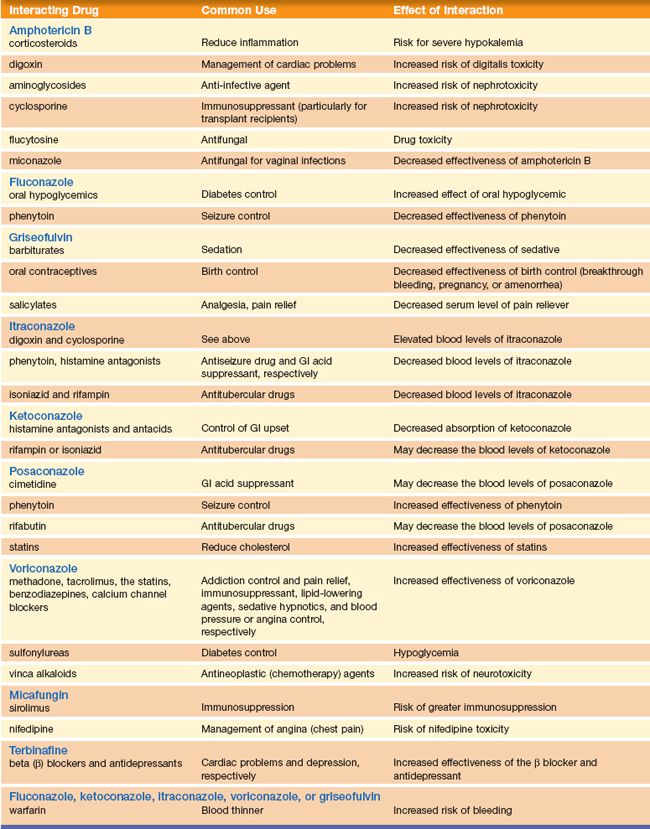
Interactions
Possible interactions depend on the individual drugs, and many interactions can occur. See Table 12.3 for more drug interaction information.
NURSING PROCESS
PATIENT RECEIVING AN ANTIFUNGAL DRUG
ASSESSMENT
Preadministration Assessment
Assess the patient for signs of infection before giving the first dose of an antifungal drug. It is important to ask about pain and to describe white plaques or sore areas on mucous membranes of the oral or perineal areas, as well as any vaginal discharge. Take and record vital signs. When the patient is scheduled to receive amphotericin or flucytosine for a systemic fungal infection, be sure to weigh the patient because the dosage of the drug is determined according to the patient’s weight.
Ongoing Assessment
The ongoing assessment involves careful observation of the patient every 2 to 4 hours for adverse drug reactions when the antifungal drug is given by the oral or parenteral route. When these drugs are administered topically or on an outpatient basis, instruct the patient in what to look for when gathering ongoing assessment data. This should include signs of improvement and adverse reactions, both minor and severe (requiring immediate notification of the primary health care provider).
NURSING DIAGNOSES
Drug-specific nursing diagnoses are the following:
 Impaired Comfort related to intravenous (IV) administration of amphotericin B
Impaired Comfort related to intravenous (IV) administration of amphotericin B
 Risk for Ineffective Tissue Perfusion: Renal related to adverse reactions of the antifungal drug
Risk for Ineffective Tissue Perfusion: Renal related to adverse reactions of the antifungal drug
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient depend on the reason for administering the antifungal drug but may include a therapeutic response to the antifungal drug, patient needs related to the management of adverse reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy: Administering Specific Antifungal Drugs
AMPHOTERICIN B. Amphotericin B is given only under close supervision in the hospital setting. Its use is reserved for serious and potentially life-threatening fungal infections. This drug is administered daily or every other day over several days or months.
The IV solution of amphotericin B is light sensitive and should be protected from exposure to light. If the solution is used within 8 hours, there is negligible loss of drug activity. Therefore, once the drug is reconstituted, administer the medication immediately, because the typical IV infusion is for a period of 6 hours or more. Consult the clinical pharmacist regarding whether to use a protective covering for the infusion container.
 NURSING ALERT
NURSING ALERT
Renal damage is the most serious adverse reaction to the use of amphotericin B. Renal impairment usually improves with a modification of the dosage regimen (reduced dosage or increased time between doses). Serum creatinine levels and blood urea nitrogen (BUN) levels are checked frequently during the course of therapy to monitor kidney function. If the BUN exceeds 40 mg/dL or the serum creatinine level exceeds 3 mg/dL, the primary health care provider may discontinue the drug or reduce the dosage until renal function improves.
NONSYSTEMIC ANTIFUNGAL INFECTION PREPARATIONS. When a vaginal fungal infection is treated with miconazole during pregnancy, a vaginal applicator may be contraindicated. Manual insertion of the vaginal tablets may be preferred. Because small amounts of these drugs may be absorbed from the vagina, they are used only when essential during the first trimester.
Oral thrush infections (candidiasis) may be treated with oral solutions. Instruct the patient to swish and hold the solution in the mouth for several seconds (or as long as possible), gargle, and swallow the solution. Oral infections also may be treated with medication lozenges. Sometimes the vaginal troche preparation of an antifungal medication is prescribed for oral use. The patient needs specific instructions on how to use the medication to prevent confusion and improper use.
Monitoring and Managing Patient Needs
IMPAIRED COMFORT: MEDICATION ADMINISTRATION. When administering amphotericin B by IV infusion, be aware that immediate adverse reactions can occur. Nausea, vomiting, hypotension, tachypnea, fever, and chills (sometimes called rigors) may occur within 15 to 20 minutes of beginning the IV infusion. To prevent these adverse reactions, patients may be premedicated with antipyretics, antihistamines, or antiemetics. It is important to monitor the patient’s temperature, pulse, respirations, and blood pressure carefully during the first 30 minutes to 1 hour of treatment. Monitor vital signs every 2 to 4 hours during therapy, depending on the patient’s condition. Also check the IV infusion rate and the infusion site frequently during administration of the drug. This is especially important if the patient is restless or confused.
Patients should be taught before the drug is given that the side effects can be uncomfortable. Warm blankets should be provided for patient comfort. Reassure the patient that the medications administered before the antifungal will help to ease the adverse reactions. Instruction should include that the reactions decrease with ongoing therapy.
RISK FOR INEFFECTIVE TISSUE PERFUSION: RENAL. When the patient is taking a drug that is potentially toxic to the kidneys, carefully monitor fluid intake and output. If the patient is known to have renal compromise, perform hourly measurements of urine output. Periodic laboratory tests are usually ordered to monitor the patient’s response to therapy and detect toxic reactions. Serum creatinine and BUN levels are checked frequently during the course of therapy to monitor kidney function. If the BUN exceeds 40 mg/dL or if the serum creatinine level exceeds 3 mg/dL, the primary health care provider may discontinue the drug therapy or reduce the dosage until renal function improves.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Before administering fluconazole to an older adult or a patient with renal impairment, the primary health care provider may order a creatinine clearance test. Watch for and report the laboratory results to the primary health care provider because the dosage may be adjusted based on the test results.
Educating the Patient and Family
If the patient is being treated in the ambulatory care setting, include the following points in the teaching plan:
 Clean the involved area and apply the ointment or cream to the skin as directed by the primary health care provider.
Clean the involved area and apply the ointment or cream to the skin as directed by the primary health care provider.
 Do not increase or decrease the amount used or the number of times the ointment or cream should be applied unless directed to do so by the primary health care provider.
Do not increase or decrease the amount used or the number of times the ointment or cream should be applied unless directed to do so by the primary health care provider.
Drug-specific teaching points include:
 Flucytosine—Nausea and vomiting may occur with this drug. Reduce or eliminate these effects by taking a few capsules at a time during a 15-minute period. If nausea, vomiting, or diarrhea persists, notify the primary health care provider as soon as possible.
Flucytosine—Nausea and vomiting may occur with this drug. Reduce or eliminate these effects by taking a few capsules at a time during a 15-minute period. If nausea, vomiting, or diarrhea persists, notify the primary health care provider as soon as possible.
 Griseofulvin—Beneficial effects may not be noticed for some time; therefore, take the drug for the full course of therapy. Avoid exposure to sunlight and sunlamps because an exaggerated skin reaction (which is similar to severe sunburn) may occur even after a brief exposure to ultraviolet light. Notify the primary health care provider if fever, sore throat, or skin rash occurs.
Griseofulvin—Beneficial effects may not be noticed for some time; therefore, take the drug for the full course of therapy. Avoid exposure to sunlight and sunlamps because an exaggerated skin reaction (which is similar to severe sunburn) may occur even after a brief exposure to ultraviolet light. Notify the primary health care provider if fever, sore throat, or skin rash occurs.
 Ketoconazole—Complete the full course of therapy as prescribed by the primary health care provider. Do not take this drug with an antacid. In addition, avoid the use of nonprescription drugs unless use of a specific drug is approved by the primary health care provider. This drug may produce headache, dizziness, and drowsiness. If drowsiness or dizziness occurs, use caution while driving or performing other hazardous tasks. Notify the primary health care provider if pronounced abdominal pain, fever, or diarrhea occurs.
Ketoconazole—Complete the full course of therapy as prescribed by the primary health care provider. Do not take this drug with an antacid. In addition, avoid the use of nonprescription drugs unless use of a specific drug is approved by the primary health care provider. This drug may produce headache, dizziness, and drowsiness. If drowsiness or dizziness occurs, use caution while driving or performing other hazardous tasks. Notify the primary health care provider if pronounced abdominal pain, fever, or diarrhea occurs.
 Itraconazole—The drug is taken with food. Therapy continues for at least 3 months until infection is controlled. Report unusual fatigue, yellow skin, darkened urine, anorexia, nausea, and vomiting.
Itraconazole—The drug is taken with food. Therapy continues for at least 3 months until infection is controlled. Report unusual fatigue, yellow skin, darkened urine, anorexia, nausea, and vomiting.
 Miconazole—If the drug (cream or tablet) is administered vaginally, insert the drug high in the vagina using the applicator provided with the product. Wear a pantiliner after insertion of the drug to prevent staining of the clothing and bed linen. Continue taking the drug during the menstrual period if the vaginal route is being used. Do not have intercourse while taking this drug, or advise the partner to use a condom to avoid reinfection. To prevent recurrent infections, avoid nylon, thong underwear, and tight-fitting garments. If there is no improvement in 5 to 7 days, stop using the drug and consult the primary care provider, because a more serious infection may be present. If abdominal pain, pelvic pain, rash, fever, or offensive-smelling vaginal discharge is present, do not use the drug, but notify the primary health care provider.
Miconazole—If the drug (cream or tablet) is administered vaginally, insert the drug high in the vagina using the applicator provided with the product. Wear a pantiliner after insertion of the drug to prevent staining of the clothing and bed linen. Continue taking the drug during the menstrual period if the vaginal route is being used. Do not have intercourse while taking this drug, or advise the partner to use a condom to avoid reinfection. To prevent recurrent infections, avoid nylon, thong underwear, and tight-fitting garments. If there is no improvement in 5 to 7 days, stop using the drug and consult the primary care provider, because a more serious infection may be present. If abdominal pain, pelvic pain, rash, fever, or offensive-smelling vaginal discharge is present, do not use the drug, but notify the primary health care provider.
EVALUATION
 Therapeutic response is achieved and there is no evidence of infection.
Therapeutic response is achieved and there is no evidence of infection.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
• Patient reports comfort, without fever or chills.
• Kidney perfusion is maintained.
 Patient and family express confidence and demonstrate understanding of the drug regimen.
Patient and family express confidence and demonstrate understanding of the drug regimen.
Parasitic Infections
A parasite is an organism that lives in or on another organism (the host) without contributing to the survival or well-being of the host. These infections are infrequent in most populations in the United States except the immunocompromised. Helminthiasis (invasion of the body by parasitic worms) and protozoal infections (invasion of the body by single-celled parasites or malaria) are worldwide health problems. What makes these diseases especially worthy of concern is the frequency of global air travel in modern society. Conditions once confined to specific parts of the world can now be spread in hours or days by air travel.
ANTHELMINTIC DRUGS
Roundworms, pinworms, whipworms, hookworms, and tapeworms are examples of helminths. The most common parasitic worm across the world is the roundworm. In the United States, the most common worm seen is the pinworm. Anthelmintic (against helminths) drugs are used to treat helminthiasis.
Actions and Uses
Although the actions of anthelmintic drugs vary, their primary purpose is to kill parasites.
Albendazole (Albenza) interferes with the synthesis of the parasite’s microtubules, resulting in death of susceptible larvae. This drug is used to treat larval forms of pork tapeworm and to treat liver, lung, and peritoneum disease caused by the dog tapeworm.
Mebendazole blocks the uptake of glucose by the helminth, resulting in depletion of the helminth’s own glycogen. This drug is used to treat whipworm, pinworm, roundworm, American hookworm, and the common hookworm.
The activity of pyrantel (Antiminth) is probably due to its ability to paralyze the helminth. Paralysis causes the helminth to release its grip on the intestinal wall, after which it can be excreted in the feces. Pyrantel is used to treat roundworm and pinworm.
Adverse Reactions
Generalized adverse reactions include the following:
• Drowsiness, dizziness
• Nausea, vomiting
• Abdominal pain and cramps, diarrhea
Adverse reactions associated with the anthelmintic drugs, if they do occur, are usually mild when the drug is used in the recommended dosage. Rash is a serious adverse reaction to pyrantel, which is sold over the counter (without a prescription). As such, patients may begin self-treatment before notifying their primary health provider. Therefore, it is important to instruct the patient to notify the primary health care provider if this skin reaction occurs. For more information, see the Summary Drug Table: Antifungal and Antiparasitic Drugs.
Contraindications and Precautions
The anthelmintic drugs are contraindicated in patients with known hypersensitivity to the drugs and during pregnancy (pregnancy category C). They should be used cautiously in lactating patients, patients with hepatic or renal impairment, and patients with malnutrition or anemia.
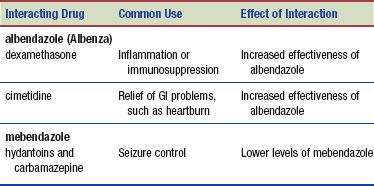
Interactions
The following interactions may occur when a specific anthelmintic drug is administered with another agent:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


