DRUG CLASSES
Insulins
Sulfonylureas
Nonsulfonylureas
Incretin mimetics
PHARMACOLOGY IN PRACTICE

When Mr. Phillip was seen for atrial fibrillation, it was discovered that he had not been seen by a health care provider in more than 5 years. The first priority was to stabilize his heart and coagulation status. He was then given an appointment to come to the clinic for a complete physical examination. During the clinic visit, Mr. Phillip was found to be in relatively good physical condition, yet his blood chemistries showed an elevation in his blood glucose level (153 mg/dL) and his HbA1c reading was 9%. When his wife was alive, he remembers she started fixing food in a different way because of the doctor’s concerns about eating too much sugar. When you finish this chapter, you should better understand the meaning of these laboratory values and know what patient interventions and instruction should follow.
Insulin is essential for cells to utilize glucose for energy and for the proper metabolism of protein and fat in our bodies. A hormone produced by the pancreas, insulin is required for the proper use of glucose (carbohydrate). This is accomplished by the release of small amounts of insulin into the bloodstream throughout the day in response to changes in blood glucose levels. Insulin lowers blood glucose levels by inhibiting glucose production by the liver. Insulin also controls the storage and utilization of amino acids and fatty acids.
Diabetes mellitus (often referred to as simply diabetes) is a complicated, chronic disorder characterized either by insufficient insulin production by the beta (β) cells of the pancreas or by cellular resistance to insulin. Insulin insufficiency results in elevated blood glucose levels, or hyperglycemia. As a result of the disease, individuals with diabetes are at greater risk for a number of disorders, including myocardial infarction, cerebrovascular accident (stroke), blindness, kidney disease, and lower limb amputations.
Insulin and antidiabetic drugs, along with diet and exercise, are the cornerstones of treatment for diabetes. They are used to prevent episodes of hypoglycemia and normalize carbohydrate metabolism.
There are two major types of diabetes mellitus:
• Type 1—formerly known as insulin-dependent diabetes mellitus or IDDM
• Type 2—formerly known as non–insulin-dependent diabetes mellitus or NIDDM
Those with type 1 diabetes produce insulin in insufficient amounts and therefore must have insulin supplementation to survive (Fig. 42.1). Type 1 diabetes usually has a rapid onset, occurs before age 20 years, produces more severe symptoms than type 2 diabetes, and is more difficult to control. Major symptoms of type 1 diabetes include hyperglycemia, polydipsia (increased thirst), polyphagia (increased appetite), polyuria (increased urination), and weight loss. Control of type 1 diabetes is particularly difficult because of the lack of insulin production by the pancreas. Treatment requires a strict regimen that typically includes a carefully calculated diet, planned physical activity, home glucose testing several times a day, and daily supplement of insulin by injections or pump.
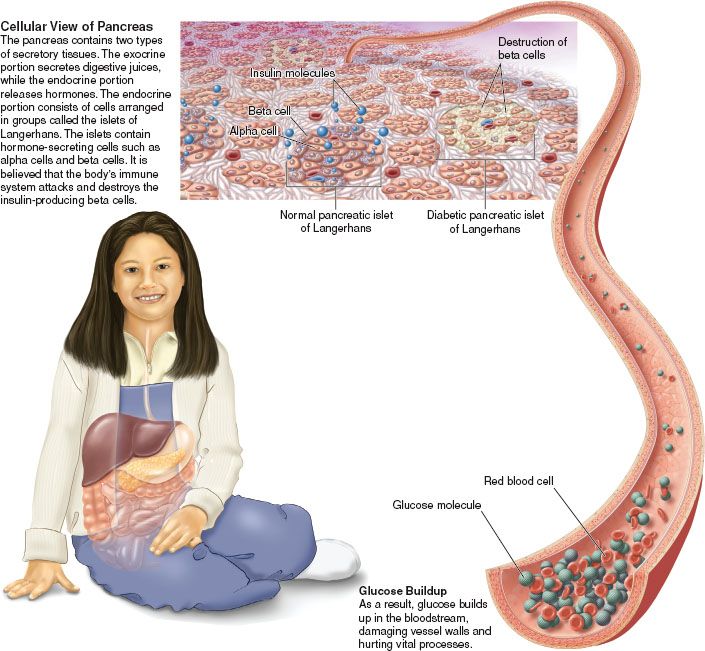
Figure 42.1 Cellular view of type 1 diabetes. (Courtesy of Anatomical Chart Co.)
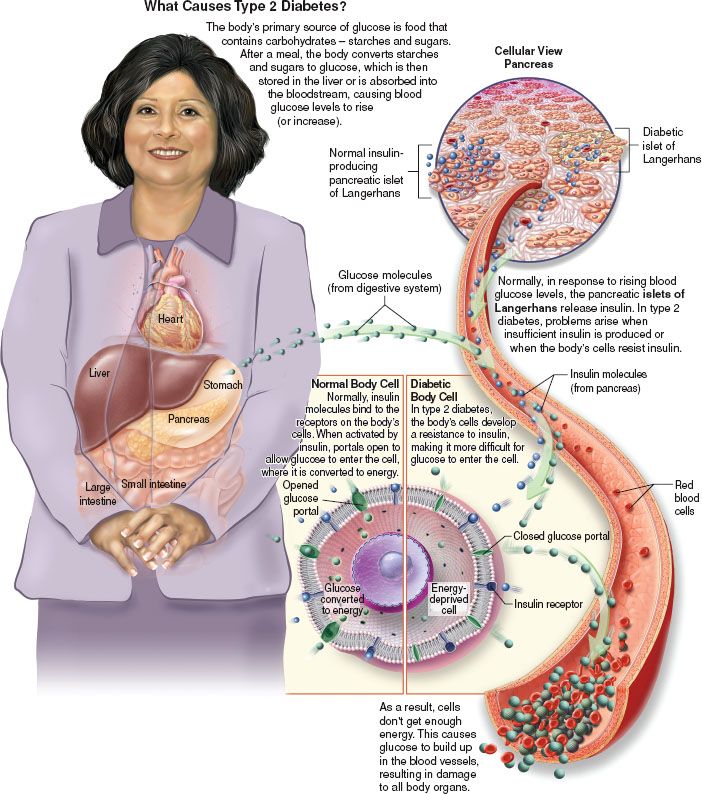
Figure 42.2 Cellular view of type 2 diabetes. (Courtesy of Anatomical Chart Co.)
Type 2 diabetes mellitus affects about 90% to 95% of individuals with diabetes. Those with type 2 diabetes are affected either by decreased production of insulin by the β cells of the pancreas or by decreased sensitivity of the body cells to insulin, making the cells insulin resistant (Fig. 42.2). Although type 2 diabetes may occur at any age, the disorder occurs most often after age 40 years. The onset of type 2 diabetes is usually insidious. Symptoms are less severe than in type 1 diabetes, and because it tends to be more stable, type 2 diabetes is easier to control than type 1. Risk factors for type 2 diabetes include:
- Obesity
- Older age
- Family history of diabetes
- History of gestational diabetes (diabetes that develops during pregnancy but disappears when pregnancy is over)
- Impaired glucose tolerance
- Minimal or no physical activity
- Race/ethnicity (African Americans, Hispanic/Latino Americans, Native Americans, and some Asian Americans)
In many individuals with type 2 diabetes, the disorder can be controlled with diet, exercise, and oral antidiabetic drugs. However, about 40% of those with type 2 diabetes respond poorly to the oral antidiabetic drugs and require insulin to control the disorder.
Insulin is a hormone manufactured by the β cells of the pancreas. Pharmaceutical human insulin is derived from a biosynthetic process (recombinant DNA or rDNA). Animal-source insulins are used less frequently today than in the past. They have been replaced by synthetic insulins, such as human insulin or insulin analogs. Insulin analogs, insulin lispro, and insulin aspart are newer forms of insulin made using recombinant DNA technology and are structurally similar to human insulin.
Actions
Insulin appears to activate a process that helps glucose molecules enter the cells of striated muscle and adipose tissue. Figure 42.2 depicts the difference between normal glucose metabolism and that of the cell affected by diabetes. Insulin also stimulates the synthesis of glycogen by the liver. In addition, insulin promotes protein synthesis and helps the body store fat by preventing its breakdown for energy.
Onset, Peak, and Duration of Action
Onset, peak, and duration are three clinically important properties of insulin:
• Onset—when insulin first begins to act in the body
• Peak—when the insulin is exerting maximum action
• Duration—the length of time the insulin remains in effect
To meet the needs of those with diabetes mellitus, various insulin preparations have been developed to delay the onset and prolong the duration of action of insulin. When insulin is combined with protamine (a protein), its absorption from the injection site is slowed and its duration of action is prolonged. The addition of zinc also modifies the onset and duration of action of insulin. Insulin preparations are classified as rapid acting, intermediate acting, or long acting. See the Summary Drug Table: Insulin Preparations for information concerning the onset, peak, and duration of various insulins.
Uses
Insulin is used to:
• Control type 1 diabetes
• Control type 2 diabetes when uncontrolled by diet, exercise, or weight reduction
• Treat severe diabetic ketoacidosis (DKA) or diabetic coma
• Treat hypokalemia in combination with glucose
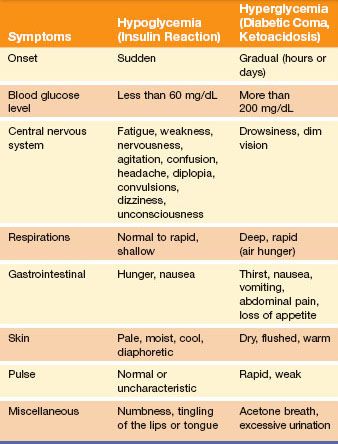
Adverse Reactions
The two major adverse reactions seen with insulin administration are hypoglycemia (low blood glucose, or sugar level) and hyperglycemia (elevated blood glucose, or sugar level). The symptoms of hypoglycemia and hyperglycemia are listed in Table 42.1.
Hypoglycemia may occur when there is too much insulin in the bloodstream in relation to the available glucose (hyperinsulinism). Hypoglycemia may occur when:
• The patient eats too little food.
• The insulin dose is incorrectly measured and is greater than that prescribed.
• The patient has drastically increased demands (activity or illness).
Table 42.1 Hypoglycemia Versus Hyperglycemia
Display 42.1 Drugs That Alter Insulin Effectiveness
Selected Drugs That Decrease the Effect (More Insulin May Be Required)
acetazolamide
albuterol
antipsychotics (atypical or second generation)
asparaginase
calcitonin
contraceptives, oral
corticosteroids
cyclophosphamide
danazol
diltiazem
diuretics
dobutamine
epinephrine
estrogens
glucagon
human immunodeficiency virus (HIV) antivirals
isoniazid
lithium
morphine sulfate
niacin
nicotine
phenothiazines
phenytoin
progestogens
protease inhibitors
somatropin
terbutaline
thiazide diuretics
thyroid hormones
Drugs That Increase the Effect (Less Insulin May Be Required)
angiotensin-converting enzyme (ACE) inhibitors
alcohol
anabolic steroids
antidiabetic drugs, oral
β-blocking drugs
calcium
clonidine
disopyramide
fluoxetine
fibrates
lithium
MAOIs
mebendazole
pentamidine
pentoxifylline
pyridoxine
salicylates
somatostatin analog
sulfonamides
tetracycline
Hyperglycemia may occur if there is too little insulin in the bloodstream in relation to the available glucose (hypoinsulinism). Hyperglycemia may occur when:
• The patient eats too much food.
• Too little or no insulin is given.
• The patient experiences emotional stress, infection, surgery, pregnancy, or an acute illness.
An individual can also become insulin resistant because antibodies develop against insulin. These patients have impaired receptor function and become so unresponsive to insulin that the dose requirement may be in excess of 500 units/day, rather than the usual 40 to 60 units/day. High-potency insulin in a concentrated form (U500) is used for patients requiring more than 200 units/day.
Contraindications and Precautions
Specific insulin products are contraindicated when the patient is hypoglycemic. Insulin is used cautiously in patients with renal or hepatic impairment and during pregnancy and lactation. The insulins are grouped in pregnancy category B, except for insulin glargine and insulin aspart, which are in pregnancy category C. Insulin appears to inhibit milk prowduction in lactating women and could interfere with breastfeeding. Lactating women may require adjustment in insulin dose and diet.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pregnancy
Pregnancy makes diabetes more difficult to manage. Insulin requirements usually decrease in the first trimester, increase during the second and third trimesters, and decrease rapidly after delivery. The patient with diabetes or a history of gestational diabetes must be encouraged to maintain good metabolic control before conception and throughout pregnancy.
Interactions
When certain drugs are administered with insulin, a resultant decrease or increase in hypoglycemic effect can occur. Display 42.1 identifies selected drugs that decrease and increase the hypoglycemic effect of insulin.
Patients may not volunteer information regarding their use of complementary and alternative remedies. You should always inquire about use of herbal products. Although lab testing is not conclusive, medical reports indicate a possible interaction with eucalyptus products, causing decreased blood sugar.
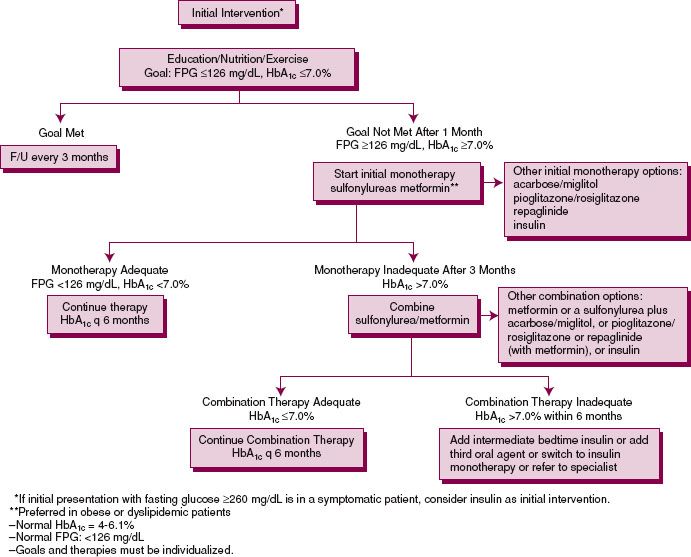
Figure 42.3 Pharmacologic algorithm for treating type 2 diabetes. FPG, fasting plasma glucose; HbA1c, glycosylated hemoglobin; F/U, follow-up.
Oral antidiabetic drugs are used to treat patients with type 2 diabetes that is not controlled by diet and exercise alone. These drugs are not effective for treating type 1 diabetes. These drugs may also be called oral hypoglycemics. A number of oral antidiabetic drugs are currently in use and can be categorized into two groups:
• Sulfonylureas
• Nonsulfonylureas
Newer agents include those that interact or mimic the action of incretin hormones. These additional drugs are listed in the Summary Drug Table: Antidiabetic Drugs.
Uses
Oral antidiabetic drugs are used in the treatment of patients with type 2 diabetes mellitus whose condition cannot be controlled by diet alone. These drugs may also be used with insulin in the management of some patients with diabetes. Use of an oral antidiabetic drug with insulin may help to decrease the insulin dosage in some individuals. Two oral antidiabetic drugs (e.g., a sulfonylurea and metformin) may also be used together when one antidiabetic drug and diet do not control blood glucose levels of those with type 2 diabetes. Figure 42.3 illustrates an example of a treatment protocol for type 2 diabetes.
Actions
Sulfonylureas
Sulfonylureas appear to lower blood glucose by stimulating the β cells of the pancreas to release insulin. Sulfonylureas are not effective if the β cells of the pancreas cannot release a sufficient amount of insulin to meet the individual’s needs. The most commonly used sulfonylureas are the second- and third-generation drugs, such as glimepiride (Amaryl), glipizide (Glucotrol), and glyburide (DiaBeta). The first-generation sulfonylureas (e.g., chlorpropamide [Diabinese], tolazamide, and tolbutamide) are not commonly used today because they have a long duration of action and a higher incidence of adverse reactions and are more likely to react with other drugs.
Like the sulfonylureas, the meglitinides act to lower blood glucose levels by stimulating the release of insulin from the pancreas. This action depends on the ability of the β cells in the pancreas to produce some insulin. However, the action of the meglitinides is more rapid than that of the sulfonylureas and their duration of action much shorter. Because of this, they must be taken three times a day. Examples of the meglitinides include nateglinide (Starlix) and repaglinide (Prandin).
Nonsulfonylureas
The liver normally releases glucose by detecting the level of circulating insulin. When insulin levels are high, glucose is available in the blood, and the liver produces little or no glucose. When insulin levels are low, there is little circulating glucose, so the liver produces more glucose. In type 2 diabetes, the liver may not detect levels of glucose in the blood and, instead of regulating glucose production, releases glucose despite adequate blood glucose levels.
Metformin sensitizes the liver to circulating insulin levels and reduces hepatic glucose production. The alpha (α)-glucosidase inhibitors acarbose (Precose) and miglitol (Glyset) lower blood glucose levels by delaying the digestion of carbohydrates and absorption of carbohydrates in the intestine. The thiazolidinediones, also called glitazones, decrease insulin resistance and increase insulin sensitivity by modifying several processes, resulting in decreased hepatic glucogenesis (formation of glucose from glycogen) and increased insulin-dependent muscle glucose uptake. Examples of the thiazolidinediones are rosiglitazone (Avandia) and pioglitazone (Actos).
Adverse Reactions
Sulfonylureas
Adverse reactions associated with sulfonylureas include hypoglycemia, anorexia, nausea, vomiting, epigastric discomfort, weight gain, heartburn, and various vague neurologic symptoms, such as weakness and numbness of the extremities. Often, these can be eliminated by reducing the dosage or giving the drug in divided doses. If these reactions become severe, the primary health care provider may try another oral antidiabetic drug or discontinue the use of these drugs. If the drug therapy is discontinued, it may be necessary to control the diabetes with insulin. Adverse reactions associated with the administration of the meglitinides include upper respiratory tract infection, headache, rhinitis, bronchitis, headache, back pain, and hypoglycemia.
Nonsulfonylureas
Adverse reactions associated with nonsulfonylureas include GI upset (e.g., metallic taste, abdominal bloating, nausea, cramping, flatulence, and diarrhea). These adverse reactions are self-limiting and can be reduced if the patients are started on a low dose with dosage increased slowly, and if the drug is taken with meals. Hypoglycemia rarely occurs when a nonsulfonylurea is used alone. However, patients receiving these drugs in combination with insulin or other oral hypoglycemics (e.g., sulfonylureas) are at greater risk for hypoglycemia. A reduction in the dosage of insulin or the sulfonylurea may be required to prevent episodes of hypoglycemia.
Adverse reactions associated with the administration of thiazolidinediones include upper respiratory infections, sinusitis, headache, pharyngitis, myalgia, diarrhea, and back pain. Lactic acidosis (buildup of lactic acid in the blood) may also occur with the administration of metformin. Although lactic acidosis is a rare adverse reaction, its occurrence is serious and can be fatal. Lactic acidosis occurs mainly in patients with kidney dysfunction. Symptoms of lactic acidosis include malaise (vague feeling of bodily discomfort), abdominal pain, rapid respirations, shortness of breath, and muscular pain. In some patients, vitamin B12 levels are decreased. This can be reversed with vitamin B12 supplements or with discontinuation of the drug therapy. Because weight loss can occur, metformin is sometimes recommended for obese patients or patients with insulin-resistant diabetes.
Contraindications, Precautions, and Interactions
Sulfonylureas
Oral antidiabetic drugs are contraindicated in patients with known hypersensitivity to the drugs, DKA, severe infection, or severe endocrine disease. The first-generation sulfonylureas (chlorpropamide, tolazamide, and tolbutamide) are contraindicated in patients with coronary artery disease or liver or renal dysfunction. Other sulfonylureas are used cautiously in patients with impaired liver function because liver dysfunction can prolong the drug’s effect. In addition, sulfonylureas are used cautiously in patients with renal impairment and severe cardiovascular disease. There is a risk for cross-sensitivity with sulfonylureas and sulfonamides (sulfa anti-infectives).
Many drugs may affect the action of sulfonylureas; monitor blood glucose carefully when beginning therapy, when discontinuing therapy, and any time any change is made in the drug regimen with these drugs. Sulfonylureas may have an increased hypoglycemic effect when administered with anticoagulants, chloramphenicol, clofibrate, fluconazole, histamine H2 antagonists, methyldopa, monoamine oxidase inhibitors (MAOIs), nonsteroidal anti-inflammatory drugs (NSAIDs), salicylates, sulfonamides, and tricyclic antidepressants. The hypoglycemic effect of sulfonylureas may be decreased when the agents are administered with β blockers, calcium channel blockers, cholestyramine, corticosteroids, estrogens, hydantoins, isoniazid, oral contraceptives, phenothiazines, rifampin, thiazide diuretics, and thyroid agents.
Nonsulfonylureas
Nonsulfonylureas are contraindicated in patients with heart failure (HF), renal disease, hypersensitivity to the individual drug, and acute or chronic metabolic acidosis, including ketoacidosis. The drug is also contraindicated in patients older than 80 years and during pregnancy (pregnancy category B, the thiazolidinediones are pregnancy category C) and lactation.
Metformin use is temporarily discontinued for surgical procedures. The drug therapy is restarted when the patient’s oral intake has been resumed and renal function is normal. There is a risk of acute renal failure when iodinated contrast material used for radiologic studies is administered with metformin. Metformin therapy is stopped for 48 hours before and after radiologic studies using iodinated material. There is an increased risk of lactic acidosis when metformin is administered with the glucocorticoids.
Digestive enzymes may reduce the effect of miglitol. Acarbose and miglitol are used cautiously in patients with renal impairment or pre-existing GI problems, such as irritable bowel syndrome or Crohn’s disease. Thiazolidinediones are used cautiously in patients with edema, cardiovascular disease, and liver or kidney disease. These drugs may alter the effects of oral contraceptives.
These hormones are released in response to increases in glucose that occur after eating. Incretin hormones cause insulin to be made and reduce the amount of glucagon made by the pancreas. Hormone mimetic agents help control blood glucose levels by maintaining β cell function of the pancreas, enhancing insulin secretion, and suppressing glucagon, which signals the liver to decrease release of glucose. Gastric emptying is also delayed, which slows carbohydrate absorption.
Sitagliptin (Januvia) lowers the blood glucose level of those with type 2 diabetes by enhancing the secretion of the endogenous incretin hormone. Exenatide (Byetta) mimics the action of the incretin hormone. Pramlintide (Symlin) mimics the action of another secretion, amylin.
An incretin mimetic should be used cautiously in patients with chronic kidney disease or in older adults. This drug has not been studied in pregnant women but is believed to be a category B drug from animal studies, and it should be used cautiously in lactating women.
NURSING PROCESS
PATIENT RECEIVING AN UPPER RESPIRATORY SYSTEM DRUG
ASSESSMENT
Preadministration Assessment
When conducting a physical assessment, note that a general inspection of the skin is important for the patient with diabetes. Visualize the mucous membranes and extremities, with special attention given to any sores or cuts that appear to be infected or healing poorly, as well as any ulcerations or other skin or mucous membrane changes. Obtain the following information and include it in the patient’s record:
 Dietary habits
Dietary habits
 Family history of diabetes (if any)
Family history of diabetes (if any)
 Type and duration of symptoms experienced
Type and duration of symptoms experienced
Scan the patient’s record for recent laboratory and diagnostic tests. If the patient has diabetes and has been receiving insulin or an oral antidiabetic drug, include the type and dosage of drug used, dietary habits, and the frequency and methods used for glucose testing in the patient’s record.
Ongoing Assessment
The most important aspect of the ongoing assessment is tracking and treatment of high or low blood sugars (see Table 42.1). Frequent observation of the patient for symptoms of hypoglycemia, particularly during initial therapy or after a change in dosage, is an important ongoing assessment. The patient is particularly prone to hypoglycemic reactions at the time of peak insulin action (see the Summary Drug Table: Insulin Preparations) or when he or she has not eaten for some time or has skipped a meal. In acute care settings, frequent blood glucose monitoring is routinely done to help detect abnormalities of blood glucose.
Patients in the acute care setting are also monitored closely for hyperglycemia. Insulin needs increase in times of stress or illness. For a person without diabetes, blood glucose levels are considered within normal limits when the measure is 60 to 100 mg/dL. For a person with diabetes, the health care provider may have higher levels as the parameters for the patient. When products such as insulin glargine (Lantus) are used, the insulin levels do not fluctuate as often.
When ready for discharge, patients will need to be taught to use a glucometer for self-monitoring of blood glucose levels (see Patient Teaching for Improved Patient Outcomes: Obtaining a Blood Glucose Reading Using a Glucometer). The best way to monitor long-term glycemic control and response to treatment is with HbA1c levels measured at 3-month intervals. If the first HbA1c indicates that glycemic control during the last 3 months was inadequate, the dosages may be increased for better control.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Acute Confusion related to hypoglycemia effects on mentation
Acute Confusion related to hypoglycemia effects on mentation
 Deficient Fluid Volume related to fluid loss during DKA
Deficient Fluid Volume related to fluid loss during DKA
 Anxiety related to uncertainty of diagnosis, testing own glucose levels, self-injection, dietary restrictions, other factors (specify)
Anxiety related to uncertainty of diagnosis, testing own glucose levels, self-injection, dietary restrictions, other factors (specify)
 Ineffective Breathing Pattern related to hyperventilation in lactic acidosis with metformin use
Ineffective Breathing Pattern related to hyperventilation in lactic acidosis with metformin use
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes of the patient may include an optimal response to therapy, support of patient needs related to the management of adverse reactions, a reduction in anxiety, improved ability to cope with the diagnosis, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Nursing management of a patient with diabetes requires diligent, skillful, and comprehensive nursing care.
Patient Teaching for Improved Patient Outcomes
Obtaining a Blood Glucose Reading Using a Glucometer
When you teach, make sure your patient understands the following:
✓ Before initial use, carefully read the manufacturer’s instructions, because blood glucose monitoring devices vary greatly.
✓ Prepare the finger by cleansing the area with warm, soapy water. Rinse with warm water and dry well. (If the patient cannot prepare the area, the caregiver should wear gloves to comply with Standard Precautions, the guidelines of the Centers for Disease Control and Prevention.)
✓ Remove a test strip and close the container to prevent damage to the remaining strips. Insert the strip into the meter if the instructions call for this before obtaining the blood sample.
✓ Using the lancet (needle) device, perform a finger stick on the side of a finger (not the tip), where there are fewer nerve endings and more capillaries.
✓ Gently massage the finger to produce a large, hanging drop of blood. Using this technique to obtain a blood sample will help prevent inaccurate readings. Note: Do not smear the blood or try to obtain an extra drop.
✓ Drop the blood sample on the test strip and read the number on the meter. Note: Some glucometers, especially institutional devices, may have slightly different procedures.
✓ Record the time and test results in the record-keeping book recommended by your primary health care provider.
✓ Clean and calibrate the device according to the manufacturer’s recommendations to maintain accurate readings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree