High Yield Terms to Learn
Amine hypothesis of mood The hypothesis that major depressive disorders result from a functional deficiency of norepinephrine or serotonin at synapses in the CNS MAO inhibitors (MAOIs) Drugs inhibiting monoamine oxidases that metabolize norepinephrine and serotonin MAO type A) and dopamine (MAO type B) Tricyclic antidepressants (TCAs) Structurally related drugs that block reuptake transporters of both norepinephrine (NE) and serotonin (5-HT) Selective serotonin reuptake inhibitors (SSRIs) Drugs that selectively inhibit serotonin (5-HT) transporters with only modest effects on other neurotransmitters Serotonin-norepinephrine reuptake inhibitors (SNRIs) Heterocyclic drugs that block NE and 5-HT transporters, but lack the alpha blocking, anticholinergic and antihistaminic actions of TCAs 5-HT2 receptor antagonists Structurally related drugs that block this subgroup of serotonin receptors with only minor effects on amine transporters Heterocyclics Term used for antidepressants of varying chemical structures, the characteristics of which do not strictly conform to any of the above designations
The Amine Hypothesis of Mood
The amine hypothesis of mood postulates that brain amines, particularly norepinephrine (NE) and serotonin (5-HT), are neurotransmitters in pathways that function in the expression of mood. According to the hypothesis, a functional decrease in the activity of such amines is thought to result in depression; a functional increase of activity results in mood elevation. The amine hypothesis is largely based on studies showing that many drugs capable of alleviating symptoms of major depressive disorders enhance the actions of the central nervous system (CNS) neurotransmitters 5-HT and NE. Difficulties with this hypothesis include the facts that (1) postmortem studies do not reveal any decreases in the brain levels of NE or 5-HT in patients suffering from depression; (2) although antidepressant drugs may cause changes in brain amine activity within hours, weeks may be required for them to achieve clinical effects; (3) most antidepressants ultimately cause a downregulation of amine receptors; and (4) at least 1 effective antidepressant, bupropion, has minimal effects on brain NE or 5-HT.
Drug Classification & Pharmacokinetics
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs; eg, imipramine, amitriptyline ) are structurally related to the phenothiazine antipsychotics and share certain of their pharmacologic effects. The TCAs are well absorbed orally but may undergo first-pass metabolism. They have high volumes of distribution and are not readily dialyzable. Extensive hepatic metabolism is required before their elimination; plasma half-lives of 8-36 h usually permit once-daily dosing. Both amitriptyline and imipramine form active metabolites, nortriptyline and desipramine, respectively.
Selective Serotonin Reuptake Inhibitors
Fluoxetine is the prototype of a group of drugs that are selective serotonin reuptake inhibitors (SSRIs). All of them require hepatic metabolism and have half-lives of 18-24 h. However, fluoxetine forms an active metabolite with a half-life of several days (the basis for a once-weekly formulation). Other members of this group (eg, citalopram, escitalopram, fluvoxamine, paroxetine, and sertraline) do not form long-acting metabolites.
Heterocyclics
These drugs have varied structures and include drugs that are serotonin-norepinephrine reuptake inhibitors (SNRIs, duloxetine, venlafaxine ), 5-HT 2 receptor antagonists ( nefazodone, trazodone ) and miscellaneous other heterocyclic agents including amoxapine, bupropion, maprotiline, and mirtazapine. The pharmacokinetics of most of these agents are similar to those of the TCAs. Nefazodone and trazodone are exceptions; their half-lives are short and usually require administration 2 or 3 times daily.
Monoamine Oxidase Inhibitors
Monoamine oxidase inhibitors (MAOIs; eg, phenelzine, tranylcypromine ) are structurally related to amphetamines and are orally active. The older, standard drugs inhibit both MAO-A (monoamine oxidase type A), which metabolizes NE, 5-HT, and tyramine, and MAO-B (monoamine oxidase type A), which metabolizes dopamine. Tranylcypromine is the fastest in onset of effect but has a shorter duration of action (about 1 week) than other MAOIs (2-3 weeks). In spite of these prolonged actions, the MAOIs are given daily. They are inhibitors of hepatic drug-metabolizing enzymes and cause drug interactions. Selegiline, a selective inhibitor of MAO type B, was recently approved for treatment of depression.
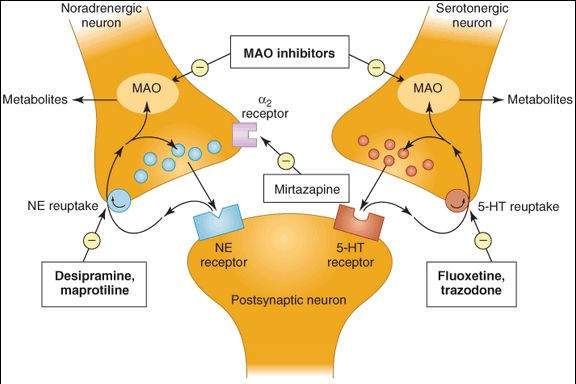
Mechanisms of Antidepressant Action
Potential sites of action of antidepressants at CNS synapses are shown in Figure 30-1. By means of several mechanisms, most antidepressants cause potentiation of the neurotransmitter actions of NE, 5-HT, or both. However, nefazodone and trazodone are weak inhibitors of NE and 5-HT transporters, and their main action appears to be antagonism of the 5-HT2A receptor. Long-term use of tricyclics and MAOIs, but not SSRIs, leads to downregulation of  receptors.
receptors.
FIGURE 30-1
Possible sites of action of antidepressant drugs. Inhibition of neuronal uptake of norepinephrine (NE) and serotonin (5-HT) increases the synaptic activities of these neurotransmitters. Inhibition of monoamine oxidase increases the presynaptic stores of both NE and 5-HT, which leads to increased neurotransmitter effects. Blockade of the presynaptic  2 autoreceptor prevents feedback inhibition of the release of NE. Note: These are acute actions of antidepressants.
2 autoreceptor prevents feedback inhibition of the release of NE. Note: These are acute actions of antidepressants.
TCAs
The acute effect of tricyclic drugs is to inhibit the reuptake mechanisms (transporters) responsible for the termination of the synaptic actions of both NE and 5-HT in the brain. This presumably results in potentiation of their neurotransmitter actions at postsynaptic receptors.
SSRIs
The acute effect of SSRIs is a highly selective action on the serotonin transporter (SERT). SSRIs allosterically inhibit the transporter, binding at a site other than that of serotonin. They have minimal inhibitory effects on the NE transporter, or blocking actions on adrenergic and cholinergic receptors.
SNRIs
SNRIs bind to transporters for both serotonin and NE, presumably enhancing the actions of both neurotransmitters. Venlafaxine has less affinity for the NE transporter than desvenlafaxine or duloxetine. The SNRIs differ from the TCAs in lacking significant blocking effects on peripheral receptors including histamine H1, muscarinic, or  -adrenergic receptors.
-adrenergic receptors.
Serotonin 5-HT2 Receptor Antagonists
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree