DRUG CLASSES
Anticoagulants
Antiplatelets
Thrombolytics
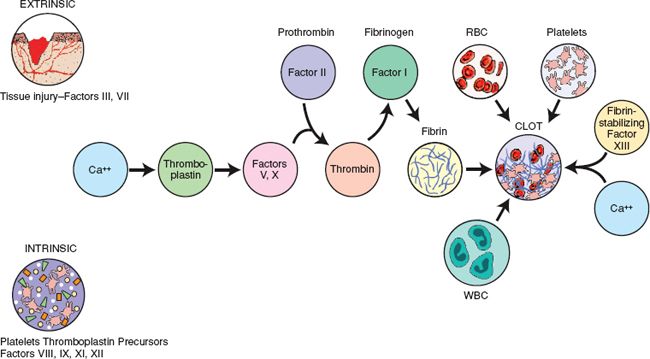
Clotting is an essential body mechanism. When a blood vessel is injured, a series of events occurs to form a clot and stop the bleeding. This process is called hemostasis. It involves a complex process also called the coagulation cascade. Figure 37.1 shows the blood clotting pathway and the extrinsic and intrinsic factors involved. The blood clotting or coagulation cascade is so named because as each factor is activated, it acts as a catalyst that enhances the next reaction, with the net result being a large collection of fibrin (the clot) that forms a plug in the vessel, thus stopping the bleeding. This is a normal event, taking a few minutes, that happens daily in response to tears and leaks in blood vessels throughout the body.
Clotting can also cause damage to both blood vessels and the tissues nourished by those vessels. Thrombosis is the formation of a blood clot, or thrombus. A thrombus may form in any vessel (artery or vein), impeding blood flow. For example, a venous thrombus can develop as the result of venous stasis (decreased blood flow), injury to the vessel wall, or altered blood coagulation. Venous thrombosis most often occurs in the lower extremities and is associated with venous stasis. Deep vein thrombosis (DVT) occurs in the lower extremities and is the most common type of venous thrombosis.
PHARMACOLOGY IN PRACTICE

Mr. Phillip is a widower and lives alone. He had not been seen in a number of years, and his physical exam shows that he has atrial fibrillation, for which he was prescribed Coumadin to take at home. The clinical pharmacist asks you about Mr. Phillip’s mental status. It seems that the weekly lab work for Mr. Phillip fluctuates considerably despite weekly teaching. After you read about these drugs, think about what action could be taken.
Figure 37.1 Blood clotting pathway. Blood coagulation results in the formation of a stable fibrin clot. Formation of this clot involves a cascade of interactions of clotting factors, platelets, and other substances. Clotting factors exist in the blood in inactive form and must be converted to an active form before the next step in the clotting pathway can occur. Each factor is stimulated in turn until the process is complete and a fibrin clot is formed. In the intrinsic pathway, all of the components necessary for clot formation are in the circulating blood. Clot formation in the intrinsic pathway is initiated by factor XII. In the extrinsic pathway, coagulation is initiated by release of tissue thromboplastin, a factor not found in circulating blood. RBC, red blood cell; WBC, white blood cell.
Arterial thrombosis can occur because of atherosclerosis or arrhythmias, such as atrial fibrillation. The thrombus may begin small, but fibrin, platelets, and red blood cells attach to the thrombus, increasing its size. When a thrombus detaches itself from the wall of the vessel and is carried along through the bloodstream, it becomes an embolus. The embolus travels until it reaches a vessel that is too small to permit its passage. If the embolus goes to the lung and obstructs a pulmonary vessel, it is called a pulmonary embolism (PE). Similarly, if the embolus detaches and occludes a vessel supplying blood to the heart, it can cause a myocardial infarction (MI).
The type of drugs discussed in this chapter include drugs that prevent the formation of blood clots (anticoagulants), drugs that suppress platelet aggregation (antiplatelets), and drugs that help to eliminate the clot (thrombolytics). For more information about specific drugs, see the Drug Summary Table: Anticoagulant, Antiplatelet, and Thrombolytic Agents.
Anticoagulants are used to prevent the formation and extension of a thrombus. Anticoagulants have no direct effect on an existing thrombus and do not reverse any damage from the thrombus. However, once the presence of a thrombus has been established, anticoagulant therapy can prevent additional clots from forming. Although they do not thin the blood, they are commonly called blood thinners by patients. The anticoagulant group of drugs includes warfarin (Coumadin; a coumarin derivative) and fractionated and unfractionated heparin. The anticoagulant drugs are used prophylactically in patients who are at high risk for clot formation.
Warfarin is the oral anticoagulant most commonly prescribed. Although primarily given by the oral route, warfarin is also available for parenteral administration. Because it can be given orally, it is the drug of choice for patients requiring long-term therapy with an anticoagulant. Peak activity is reached 1.5 to 3 days after therapy is initiated.
Heparin preparations are available as heparin sodium and the low–molecular-weight heparins (LMWHs; fractionated heparins). Heparin is not a single drug, but rather a mixture of high– and low–molecular-weight drugs. Examples of LMWH include dalteparin (Fragmin) and enoxaparin (Lovenox). LMWHs produce very stable responses when administered at recommended dosages. Because of this stability, frequent laboratory monitoring, as with heparin, is not necessary. In addition, bleeding is less likely to occur with LMWHs than with heparin.
Desirudin (Iprivask) and fondaparinux (Arixtra) are both anticoagulating drugs that inhibit portions of the coagulation cascade. They are used to prevent DVT in patients undergoing hip, knee, or abdominal surgeries.
Actions
All anticoagulants interfere with the clotting mechanism of the blood. Warfarin and anisindione interfere with the manufacturing of vitamin K–dependent clotting factors by the liver. This results in the depletion of clotting factors II (prothrombin), VII, IX, and X. It is the depletion of prothrombin (see Fig. 37.1), a substance that is essential for the clotting of blood, that accounts for most of the action of warfarin.
By contrast, heparin inhibits the formation of fibrin clots, inhibits the conversion of fibrinogen to fibrin, and inactivates several of the factors necessary for the clotting of blood. Heparin cannot be taken orally, because it is inactivated by gastric acid in the stomach; therefore, it must be given by injection. The LMWHs act to inhibit clotting reactions by binding to antithrombin III, which inhibits the synthesis of factor X and the formation of thrombin. These drugs have no effect on clots that have already formed and aid only in preventing the formation of new blood clots.
Desirudin and fondaparinux produce strong anticoagulant effects with a different mechanism of action than heparin. Additionally, their therapeutic index is narrower than heparin and can be associated with hemorrhagic complications.
Uses
Anticoagulants are used for the following:
- Prevention (prophylaxis) and treatment of DVT
- Prevention and treatment of atrial fibrillation with embolization
- Prevention and treatment of PE
- Adjuvant treatment of MI
- Prevention of thrombus formation after valve replacement surgery
Parenteral anticoagulants are used specifically for the following:
- Prevention of postoperative DVT and PE in certain patients undergoing surgical procedures, such as major abdominal surgery
- Prevention of clotting in arterial and heart surgery, in the equipment used for extracorporeal (occurring outside the body) circulation (e.g., in dialysis procedures), in blood transfusions, and in blood samples for laboratory purposes
- Prevention of a repeat cerebral thrombosis in some patients who have experienced a stroke
- Treatment of coronary occlusion, acute MI, and peripheral arterial embolism
- Diagnosis and treatment of disseminated intravascular coagulation (DIC), a severe hemorrhagic disorder
- Maintaining patency of intravenous (IV) catheters (very low doses of 10 to 100 units)
Adverse Reactions
The principal adverse reaction associated with anticoagulants is bleeding, which may range from very mild to severe. Bleeding may be seen in many areas of the body, such as the skin (bruising and petechiae), bladder, bowel, stomach, uterus, and mucous membranes. Other adverse reactions are rare but may include the following:
- Nausea, vomiting, abdominal cramping, diarrhea
- Alopecia (loss of hair)
- Rash or urticaria (hives)
- Hepatitis (inflammation of the liver), jaundice (yellowish discoloration of the skin and mucous membranes), thrombocytopenia (low platelet count), and blood dyscrasias (disorders)
Additional adverse reactions include local irritation when heparin is given by the subcutaneous (subcut) route. Hypersensitivity reactions may also occur with any route of administration and include fever and chills. More serious hypersensitivity reactions include an asthma-like reaction and an anaphylactic reaction. See the Summary Drug Table: Anticoagulant, Antiplatelet, and Thrombolytic Agents for additional adverse reactions.
Contraindications
Anticoagulants are contraindicated in patients with known hypersensitivity to the drugs, active bleeding (except when caused by DIC), hemorrhagic disease, tuberculosis, leukemia, uncontrolled hypertension, gastrointestinal (GI) ulcers, recent surgery of the eye or central nervous system, aneurysms, or severe renal or hepatic disease, and during lactation. Use during pregnancy can cause fetal death (oral agents are in pregnancy category X and parenteral agents are in pregnancy category C). The LMWHs are also contraindicated in patients with a hypersensitivity to pork products.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Jewish/Muslim Cultural Practices
Use of pork or porcine products is prohibited by some religious groups. Alert the primary health care provider if the patient notes a Jewish or Muslim religious preference and is likely to undergo anticoagulant therapy. The drug fondaparinux (Arixtra) is artificially produced and does not contain pork products; this may be used as a substitute for one of the pork derivative heparin products.
Precautions
Anticoagulants are used cautiously in patients with fever, heart failure, diarrhea, diabetes, malignancy, hypertension, renal or hepatic disease, psychoses, or depression. Precaution is taken with patients undergoing spinal procedures (anesthesia or diagnostic) to be aware of the potential of spinal or epidural hematoma formation when parenteral anticoagulants are used. Women of childbearing age must use a reliable contraceptive to prevent pregnancy. These drugs are used with caution in all patients with a potential site for bleeding or hemorrhage.
Interactions
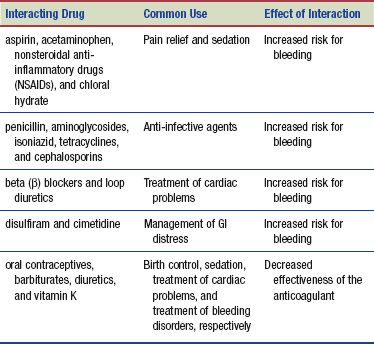
The following interactions may occur when an anticoagulant is administered with another agent:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Any herbal remedy should be used with caution in patients taking warfarin. Warfarin, a drug with a narrow therapeutic index, has the potential to interact with many herbal remedies. For example, warfarin should not be combined with any of the following substances, because they may have additive or synergistic activity and increase the risk for bleeding: celery, chamomile, clove, dong quai, feverfew, garlic, ginger, ginkgo biloba, ginseng, green tea, onion, passion flower, red clover, St. John’s wort, and turmeric.
Thrombi forming in the venous system are composed primarily of fibrin and red blood cells. In contrast, it is believed that arterial thrombosis formation is due to clumping of platelet aggregates. Therefore, anticoagulant drugs prevent thrombosis in the venous system, and the antiplatelet drugs prevent thrombus formation in the arterial system. In addition to aspirin therapy, the antiplatelet drugs include adenosine diphosphate (ADP) receptor blockers and glycoprotein receptor blockers.
Actions and Uses
These drugs work by decreasing the platelets’ ability to stick together (aggregate) in the blood, thus forming a clot. Aspirin works by prohibiting the aggregation of the platelets for the lifetime of the platelet. The ADP blockers alter the platelet cell membrane, preventing aggregation. Glycoprotein receptor blockers work to prevent enzyme production, again inhibiting platelet aggregation. Antiplatelet drug therapy is designed primarily to treat patients at risk for acute coronary syndrome, MI, stroke, and intermittent claudication.
Adverse Reactions
Some of the more common adverse reactions include the following:
• Heart palpitations
• Bleeding
• Dizziness and headache
• Nausea, diarrhea, constipation, dyspepsia
Contraindications and Precautions
Antiplatelet drugs are contraindicated in pregnant or lactating patients and those with known hypersensitivity to the drugs, congestive heart failure, active bleeding, or thrombotic thrombocytopenic purpura (TTP). These drugs are to be used cautiously in older adult patients, pancytopenic patients, or those with renal or hepatic impairment. If TTP is diagnosed, the antiplatelet treatment should be stopped immediately. Clopidogrel is a pregnancy category B and the others are pregnancy category C; none of these drugs have been well studied in humans. Antiplatelet drugs should be discontinued 1 week before any surgical procedure.
Interactions
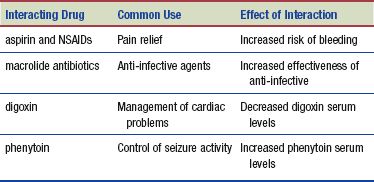
The following interactions may occur when an antiplatelet is administered with another agent:
Although these agents produce strong anticoagulant effects, their mechanism of action is distinct from that of heparins; thus, these agents should be used carefully using specific guidelines provided for each product. Thrombin inhibitors are effective anticoagulants; however, their therapeutic index is narrower than heparin and as such their nonoptimized use is potentially associated with hemorrhagic complications.
Whereas the anticoagulant agents prevent thrombus formation, the thrombolytic class of drugs dissolves blood clots that have already formed within the walls of a blood vessel. These drugs reopen blood vessels after they become occluded. Another term used to describe the thrombolytic drugs is fibrolytic. Examples of the thrombolytics include alteplase recombinant (Activase), streptokinase (Streptase), and tenecteplase (TNKase).
Actions
Although the exact action of each of the thrombolytic drugs is slightly different, these drugs break down fibrin clots by converting plasminogen to plasmin. Plasmin is an enzyme that breaks down the fibrin of a blood clot. This reopens blood vessels after their occlusion and prevents tissue necrosis. Because thrombolytic drugs dissolve all clots encountered (both occlusive and those repairing vessel leaks), bleeding is a great concern when using these agents. Before these drugs are used, their potential benefits must be weighed carefully against the potential dangers of bleeding.
Uses
These drugs are used to treat the following:
• Acute stroke or MI by lysis (breaking up) of blood clots in the coronary arteries
• Blood clots causing pulmonary emboli and DVT
• Suspected occlusions in central venous catheters
See the Summary Drug Table: Anticoagulant, Antiplatelet, and Thrombolytic Agents for a more complete listing of the use of these drugs.
Adverse Reactions
Bleeding is the most common adverse reaction seen with the use of these drugs. Bleeding may be internal and involve areas such as the GI tract, genitourinary tract, and brain. Bleeding may also be external (superficial) and seen at areas of broken skin, such as venipuncture sites and recent surgical wounds. Allergic reactions may also be seen.
Contraindications and Precautions
Thrombolytic drugs are contraindicated in a patient with known hypersensitivity to the drugs, active bleeding, and history of stroke, aneurysm, and recent intracranial surgery.
These drugs are used cautiously in patients who have recently undergone major surgery (within 10 days), such as coronary artery bypass grafting; who experienced stroke, trauma, vaginal or cesarean section delivery, GI bleeding, or trauma within the last 10 days; who have hypertension, diabetic retinopathy, or any condition in which bleeding is a significant possibility; or who are currently receiving oral anticoagulants. All of the thrombolytic drugs discussed in this chapter are classified in pregnancy category C, with the exception of urokinase, which is a pregnancy category B drug.
Interactions
When a thrombolytic is administered with medications that prevent blood clots, such as aspirin, dipyridamole, or an anticoagulant, the patient is at increased risk for bleeding.
NURSING PROCESS
PATIENT RECEIVING AN UPPER RESPIRATORY SYSTEM DRUG
ASSESSMENT
Preadministration Assessment
When immobilization is anticipated, patients are often started on preventative anticoagulant therapy. Routinely examine the extremities for color and skin temperature. In addition to vital signs, check immobile patients for a pedal pulse, noting the rate and strength of the pulse. Should a patient have a DVT, it usually occurs in a lower extremity. It is important to record any difference between the affected extremity and the unaffected extremity. Document areas of redness or tenderness and asks the patient to describe current symptoms. The affected extremity may appear edematous and a positive Homans’ sign (pain in the calf when the foot is dorsiflexed) may be elicited. A positive Homans’ sign suggests DVT.
Before administering the first dose of an anticoagulant or thrombolytic, ask the patient about all drugs taken during the previous 2 to 3 weeks (if the patient was recently admitted to the hospital). If the patient was taking any drugs before admission, review the drugs with the primary health care provider before starting an anticoagulant. The first dose of warfarin is not given until blood is drawn for a baseline prothrombin time (PT) and the international normalized ratio (INR). The dosage is individualized based on the results of the PT or the INR.
The most commonly used test to monitor heparin is the activated partial thromboplastin time (aPTT).
A complete blood count is usually drawn before the administration of the thrombolytic agents. Radiologic testing such as a computed tomography (CT) scan will be performed. Most patients receiving a thrombolytic agent are admitted or transferred to an intensive care unit, because close monitoring is necessary for 48 hours or more after therapy. If the patient is experiencing pain because of the blood clot, include a thorough pain assessment.
Ongoing Assessment
In the ongoing assessment, a patient receiving an anticoagulant, antiplatelet, or thrombolytic drug requires close observation and careful monitoring. During the course of therapy for both oral and parenteral drugs, continually assess the patient for any signs of bleeding and hemorrhage. Areas of assessment include the gums, nose, stools, urine, or nasogastric drainage. Level of consciousness should be assessed on a routine basis to monitor for intracranial bleeding.
Patients receiving warfarin for the first time often require daily adjustment of the dose, which is based on the daily PT/INR results. In settings such as long-term care or rehabilitation, this may be done with an INR monitor, similar to the glucometers used for monitoring blood glucose. If the PT exceeds 1.2 to 1.5 times the control value or the INR ratio exceeds 3, the primary health care provider is notified before the drug is given. A daily PT/INR is performed until it stabilizes and when any other drug is added to or removed from the patient’s drug regimen. After the INR has stabilized, it is monitored every 4 to 6 weeks. See Display 37.1 for more information on the laboratory tests for monitoring warfarin.
Display 37.1 Understanding Prothrombin Time and International Normalized Ratio
Prothrombin time (also called pro-time or abbreviated as “PT”) and the international normalized ratio (INR) are used to monitor the patient’s response to warfarin therapy. The daily dose of the oral anticoagulant is based on the patient’s daily PT/INR. The therapeutic range of the PT is 1.2 to 1.5 times the control value. Studies indicate that levels greater than 2 times the control value do not provide additional therapeutic effects in most patients and are associated with a higher incidence of bleeding.
Laboratories report results for the INR along with the patient’s PT and the control value. The INR “corrects” the routine PT results from different laboratories. By measuring against a known standard, the INR gives a more consistent value. The INR is maintained between 2 and 3. Values above 5 can be dangerous, and values below 1 are ineffective.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree