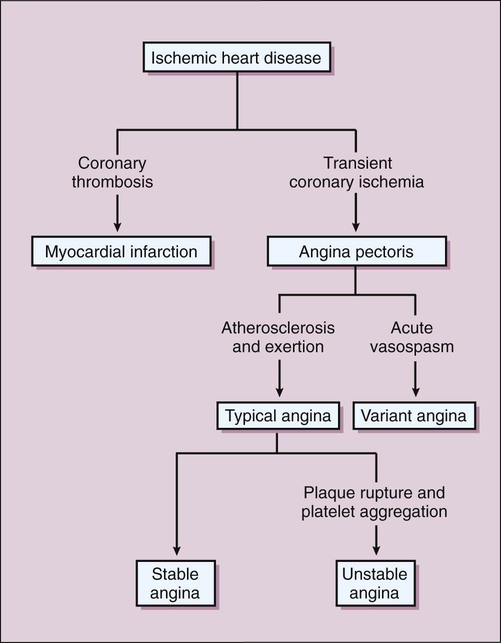
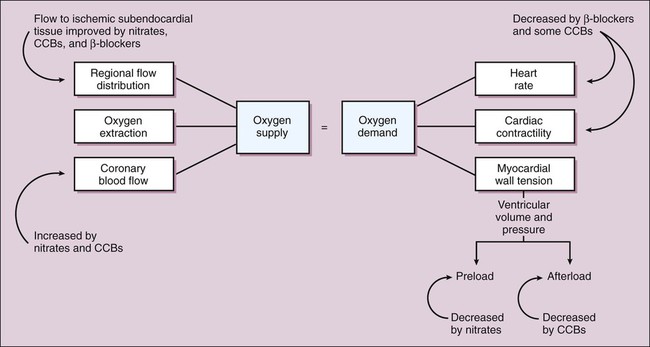
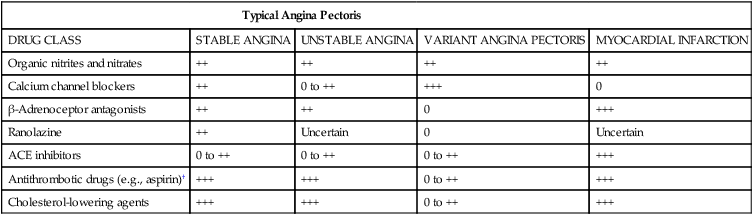
The spectrum of coronary heart disease (CHD) includes chronic angina pectoris (stable angina) and a group of acute coronary syndromes consisting of unstable angina and myocardial infarction (MI) (Fig. 11-1). Two forms of MI can be distinguished by the presence or lack of ST-segment elevation on the electrocardiogram, as described more fully in Chapter 16. All of these conditions are caused by coronary artery ischemia (inadequate blood flow) resulting from atherosclerosis, formation of thrombi (blood clots), or coronary vasospasm. Table 11-1 lists five classes of drugs and compares their efficacy in treating different forms of CHD. This chapter focuses on the anti-ischemic agents: organic nitrites and nitrates, calcium channel blockers (CCBs), and β-adrenoceptor antagonists (β-blockers), which are the primary agents used to treat angina symptoms. Chapter 15 discusses drugs for hyperlipidemia, and Chapter 16 covers antithrombotic drugs (e.g., aspirin). The latter two groups of drugs have been shown to reduce the risk of MI and death in persons with CHD. TABLE 11-1 Efficacy of Drugs Used in the Treatment of Coronary Heart Disease* ACE, Angiotensin-converting enzyme. *Ratings range from 0 (not efficacious) to +++ (highly efficacious). †Includes antiplatelet, anticoagulant, and fibrinolytic drugs. The anti-ischemic agents used in treating angina serve to prevent or counteract myocardial ischemia and thereby increase exercise tolerance and reduce the frequency of anginal attacks. This is accomplished by restoring the balance between myocardial oxygen supply and demand, by either increasing oxygen supply or decreasing oxygen demand. The factors that determine supply and demand are illustrated in Figure 11-2.
Antianginal Drugs
Overview
Coronary Heart Disease
Typical Angina Pectoris
DRUG CLASS
STABLE ANGINA
UNSTABLE ANGINA
VARIANT ANGINA PECTORIS
MYOCARDIAL INFARCTION
Organic nitrites and nitrates
++
++
++
++
Calcium channel blockers
++
0 to ++
+++
0
β-Adrenoceptor antagonists
++
++
0
+++
Ranolazine
++
Uncertain
0
Uncertain
ACE inhibitors
0 to ++
0 to ++
0 to ++
+++
Antithrombotic drugs (e.g., aspirin)†
+++
+++
0 to ++
+++
Cholesterol-lowering agents
+++
+++
0 to ++
+++
Mechanisms and Effects of Antianginal Drugs
Vasodilators
Organic Nitrites and Nitrates
Nitroglycerin, Isosorbide Dinitrate, and Isosorbide Mononitrate
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antianginal Drugs
Only gold members can continue reading. Log In or Register to continue