29
CHAPTER OUTLINE
■ HERBAL REMEDIES WITH ANTIADDICTIVE POTENTIALS
■ OPIOID DETOXIFICATION WITH TRANSCUTANEOUS ELECTRICAL ACUPUNCTURE STIMULATION
■ PREVENTION OF CRAVING AND RELAPSE TO OPIOID ABUSE
■ ACUPUNCTURE AND ALCOHOL ABUSE
Addiction is a complex process with physiologic, behavioral, psychological, and social components, so treatment is usually multifaceted. There are two fundamental approaches: prevention of the onset of compulsive use and prevention of relapse and the craving that leads to relapse. In the past, much medical attention has been directed at the symptoms of acute abstinence (detoxification), and these symptoms can be treated with available therapies and medications. However, relapse, which is often precipitated by withdrawal and/or intense craving even after prolonged abstinence, poses the most serious therapeutic challenge. In view of the complexity of drug dependence and a limited number of effective treatments, it is conceivable that certain selected alternative pharmacotherapies may have important clinical significance. This chapter reviews traditional herbal medicines and therapies for the prevention of drug and alcohol relapse.
HERBAL REMEDIES WITH ANTIADDICTIVE POTENTIALS
Poppy has been known in China for 12 centuries and for its medicinal use for 9 centuries. Opiates, alkaloids derived from poppy, effectively activate the endogenous opioid system in the body. This activation produces many cardiovascular, endocrine, immune, and neuropsychologic effects including euphoria, analgesia, and addiction. It has been clear that the effects of opioid drugs are mediated through interaction with opioid receptors. Moreover, studies of the binding of various related opioid compounds in the brain indicate the existence of a multitude of opioid receptor types and subtypes such as μ, κ, and δ (1). Since the rewarding effects of opioids are mediated through action at μ opioid receptors, interference with actions at these receptors presents a rational strategy for developing medications for opioid addiction (2,3). Specifically, medications that block activation of μ opioid receptors (e.g., naltrexone) might reduce drug-seeking behavior (1,3,4).
It was not until the middle of the 19th century that smoking opium for recreational purposes was practiced throughout China. The quantity of opium imported into China rose from 5,000 chests in 1820 to 16,000 in 1830; 20,000 in 1838; and 70,000 in 1858. After more than a century of steady demor-alization, with half the Chinese population (nearly that of the US population today) addicted, China finally determined to give up opium, which ultimately led to the “Opium Wars.” During this period, Chinese herbal remedies were developed for treating addiction or relieving the withdrawal syndrome.
The Chinese remedies developed during the Opium Wars era were combinations of more than a dozen herbs; thus, a mixture of herbs may well represent a multitargeted approach acting on opioid receptors that would have the benefits of improved overall efficacy with reduced toxicity. However, it is necessary to isolate and characterize the bioactive compounds as well as elucidate the mechanism of actions for further development of safe and complementary natural medications for drug abuse. Few original remedies have been investigated scientifically. One, YGT (NPI-025), consists of five herbs (Qiang Huo, Gou Teng, Chun Xiong, Fu Zi, and Yan Hu Suo) most frequently used for substance abuse treatment in China. Yang et al. (5) observed YGT effects among 300 individuals with “drug” addiction over a 10-year period and reported that NPI-025 significantly was associated with reduced withdrawal symptoms (−48%) compared to addicted individuals without treatment. Follow-up visits of many “cured” patients 1 to 3 years after treatment suggested that the use of NPI-025 may have been associated with overcoming craving for drugs.
After the cloning of the mouse κ opioid receptor (6,7), μ, δ and κ receptors of several species were cloned (for reviews, see 8,9). These cloned opioid receptors provide excellent tools for pharmacologic screening of traditional remedies for drug abuse. For instance, YGT (NPI-025), used clinically in Hong Kong (5,10), was subjected to bioactivity-guided fractionation and showed potent opioid receptor–binding activities (11). These studies provide important evidence for further development of such natural products.
Corydalis yanhusuo
Corydalis yanhusuo (Fig. 29-1) is one of the five Chinese medicinal plants in NPI-025. Chemical fractionation resulted in the isolation and characterization of d,l-tetrahydropalma-tine (d,l-THP) (Fig. 29-2) as one of the bioactive components. Optical resolution or chemical synthesis resulted in pure l-THP, which is the active compound with significant binding activities to D1 and D5 dopamine receptors.

FIGURE 29-1 Corydalis yanhusuo.
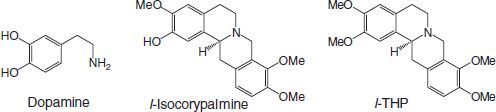
FIGURE 29-2 Structure of dopamine, isocorypalmine, and l-tetrahydropalmatine (THP).
Dopamine Receptors and Pharmacologic Actions of l-THP
Despite extensive research for new approaches, there is currently no effective pharmacotherapy for cocaine or methamphetamine addiction (12–14). Some effects of l-THP on cocaine and methamphetamine self-administration have been demonstrated (15,16), suggesting potential, but not yet proven, clinical utility. Cocaine binds differentially to the dopamine, serotonin, and norepinephrine transporter proteins and directly prevents the reuptake of dopamine, serotonin, and norepinephrine into presynaptic neurons (17–19). Inhibition of reuptake subsequently elevates the synaptic concentrations of each of these neurotransmitters, thus potentially reducing craving for cocaine and methamphetamine but also possibly causing reward, reinforcement, and addiction on their own.
Two types of dopamine receptors, D1 class and D2 class, mediate dopamine neurotransmission. The D1 class includes both D1 and D5 receptors, while the D2 class includes D2, D3, and D4 receptors (20). There is a high-density distribution of D1 and D2 receptors in the striatum, which is relevant to the pharmacology of cocaine. Recent preclinical studies suggest that drugs that are selective for D1 or D2 receptors may reduce some aspects of cocaine self-stimulation (21,22) or ethanol self-administration (23). Though both selective D1 and D2 receptor agonists can reduce cocaine self-administration, these agents can also mimic the discriminative stimulus produced by cocaine and stimulate locomotor activity (24–26); therefore, there is a risk that these drugs may also have abuse potential and would not be useful in practice for cocaine treatment.
Though selective D1 receptor agonists or D2 receptor antagonists might modulate cocaine-induced behavior (27), they have side effects that prevent them from becoming useful therapeutic agents. Indeed, preliminary clinical studies have not provided promising results (28,29). Because of the limited success of these selective compounds, interest has turned to drugs that may have dual actions. In particular, a drug that stimulates D1 receptors and blocks D2 receptors may have the right profile to become a promising treatment for cocaine or drug abuse. A recent study of one such compound, an ergoline derivative (LEK-8829) with D1 agonistic and D2 antagonist characteristics, attenuated reinstatement of cocaine seeking induced by cocaine-priming injections and diminished cocaine intake in cocaine self- administration sessions (30). Thus, it has a better profile than selective D1 receptor agonists alone for inhibiting cocaine self- administration. Furthermore, LEK-8829 reduced cocaine reinstatement behavior but did not induce reinstatement of cocaine. The combined results suggest that the strategy of using compounds with dual D1 receptor agonist/D2 receptor antagonist properties to treat drug addiction may be worth pursuing.
Similar to LEK-8829, plant-derived l-THP has both D1 receptor agonist and D2 receptor antagonist actions. Its effects on cocaine and methamphetamine addiction are suggested (15,16). One mechanism is that l-THP appears to suppress the expression of stimulant-induced conditioned place preference (CPP). l-THP could also block the discrimination behavior for methamphetamine and the reestablishment after its extinction. Interestingly, it has been reported that l-THP suppresses the craving/relapse for cocaine in addiction. Thus, these findings suggest that l-THP may have potential as a novel natural medication for inhibiting the craving/relapse of the psychostimulants addiction including cocaine and methamphetamine.
In summary, l-THP and l-isocorypalmine, a demethylated analog of l-THP, are two interesting compounds isolated from C. yanhusuo. In vitro binding study showed that both l-THP and l-isocorypalmine have affinity toward D1 and D5 receptors. In the functional assay, d,l-isocorypalmine is more potent than l-THP as D1 and D5 partial agonists. It is interesting to note that the partial skeleton of both l-THP and isocorypalmine resembles the dopamine molecule (see Fig. 29-2) with different number of methoxy group attached. These bioactive compounds derived from fractionation and in vitro screening may provide a better understanding of the mechanism of action of NPI-025 as a whole. Our recent study revealed that l-isocorypalmine is the metabolite of l-THP and has strong affinity to D1 and D5 receptors.
Uncaria rhynchophylla
Uncaria rhynchophylla (Fig. 29-3) is an important traditional Chinese medicine used in the treatment of pain, infantile convulsions, headaches, dizziness, hypertension, and rheumatoid arthritis. Uncaria rhynchophylla is another ingredient in NPI-025 (5). In order to clarify the mechanism of action, 12 compounds have been isolated by solvent extraction, followed by silica gel fractionation and Toyopearl HW-40, MCI gel column chromatography. Two major alkaloids, rhynchophylline and isorhynchophylline (Fig. 29-4), have been identified as the antiaddictive components with moderate binding activity for dopamine receptors [3H]DIP rMOR and [3H]DIP mDOR. The clinical significance of these findings is not clear.

FIGURE 29-3 Uncaria rhynchophylla.
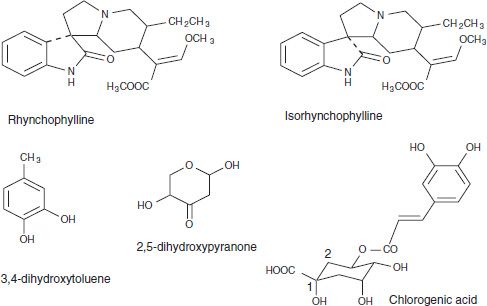
FIGURE 29-4 Structures of rhynchophylline and isorhynchophylline.
Reduction of Alcohol Drinking by the Extract of Pueraria Lobata
Isoflavone compounds naturally occurring in the root of the kudzu plant (Pueraria lobata) have been used historically to treat alcohol-related problems (31). Early work by Overstreet et al. (32,33) showed that the herbal formula NPI-028, which contains P. lobata, reduced acute alcohol consumption in two strains of alcohol-preferring rats when administered parenterally (0.25 to 1 g/kg i.p.) or orally (1 and 1.5 g/kg) without affecting water intake. Daily treatment with 1 g/kg i.p. for 5 days also was effective, as was 0.18 to 0.75 g/kg i.p. in African vervet monkeys. Several studies have systematically explored the ability of three major isoflavones of kudzu root—daidzin, daidzein, and puerarin—to reduce alcohol consumption in animals and humans. The effects of the isoflavones singly on alcohol consumption also have been studied. Keung and Vallee (34) showed that daidzin reduced consumption by 50% in Syrian golden hamsters. Heyman et al. (35) showed a dose-related decrease in alcohol-reinforced lever pressing by daidzin in rats. Puerarin was effective in two studies: Lin et al. (36,37) showed a 40% reduction of intake in female alcohol- preferring rats given 100 mg/kg/d for 7 days mixed in food and a 65% reduction at 300 mg/kg/d. In the same study, daidzin and daidzein 100 mg/kg/d reduced consumption to 75% and 50%. Benlhabib et al. (38) showed a 50% suppression of intake in rats by puerarin 50 mg/kg. In humans, Lukas et al. (39) studied the effects of a kudzu root extract that contained 25% isoflavones (19% puerarin, 4% daidzin, 2% daidzein) in heavy drinkers. Three grams of the extract (750 mg total isoflavones) was administered for 1 week before a 1.5-hour afternoon drinking session. In comparison to drinking following the placebo week, there was a significant reduction in beer consumption in addition to several significant changes in drinking topography, including an increase in the number of sips taken to finish a beer and an increase in the latency to open subsequent beers. In a second study, where the same extract was administered for 4 weeks in an outpatient setting, Penetar et al. (40) found a significant reduction in intake during weeks 2 through 4. Building on these encouraging results, we repeated the in-laboratory afternoon drinking session paradigm with the single isoflavone puerarin and found that participants consumed on average 3.5 (±0.6) beers after placebo and 2.4 (±0.4) after puerarin. None of the puerarin subjects drank five or six beers, while three placebo subjects drank five, and one drank all six (41). These studies demonstrate that puerarin may reduce alcohol drinking in humans. However, the mechanism of action of puerarin remains to be elucidated, and the implications outside of laboratory settings remain to be confirmed.
TRANSCUTANEOUS ELECTRICAL ACUPUNCTURE STIMULATION AS A NONINVASIVE ALTERNATIVE THERAPY FOR ALCOHOL AND DRUG ABUSE
In a serendipitous observation in 1972, Dr. H. L. Wen in Hong Kong noted that electroacupuncture relieved a patient’s withdrawal from opium (42). Dr. Wen and Dr. Cheung at the Kwong Wah Hospital (42) subsequently reported that, in a study of 40 individuals addicted to heroin and/or opium, acupuncture combined with electrical stimulation was effective in relieving withdrawal. This method was later adopted in many clinical settings in Western countries, including the Lincoln Hospital in New York. However, the body acupuncture points originally used by Wen and Cheung on the arm and hand were gradually omitted, with only auricular acupuncture being used (43), and electrical stimulation also was omitted, leaving only needles staying in situ. Whether these two omissions will affect therapeutic efficacy deserves further investigation.
The discovery of morphine-like substances (endorphins) in the mammalian brain (44) had a great impact on acupuncture research. It was soon made clear that acupuncture-induced analgesia (manual needling) can be blocked by the narcotic antagonist naloxone, suggesting the involvement of endogenous opioid substances (45). In animal experiments, manual acupuncture or acupuncture combined with electrical stimulation (electroacupuncture, or EA) was shown to accelerate the production and release of endorphins that can interact with different kinds of opioid receptors to ease pain (46). It was further clarified that endorphins are, in fact, a group of neuropeptides possessing different characteristics. Among these neuropeptides, β-endorphin and enkephalin are primarily agonists at μ and δ opioid receptors, whereas dynorphin is an agonist at κ receptors (47). Interestingly, electrical stimulation of different frequencies can induce the release of different kinds of endorphins. For example, low-frequency (2 to 4 Hz) EA accelerates the release of enkephalins to interact with μ and δ receptors, whereas high-frequency (100 Hz) EA accelerates the release of dynorphin to interact with κ receptors (48). These findings strengthen the scientific basis of this ancient healing art and point the way to its use in areas beyond pain control.
It is natural to hypothesize that, if acupuncture can release endogenous opioids in the brain to ease pain, it might relieve withdrawal symptoms. In fact, the first observation made by Dr. Wen in 1972 was that he attempted to use acupuncture for reducing surgical pain and incidentally found that it ameliorated the opioid withdrawal syndrome. This hypothesis was tested in morphine-dependent rats. Withdrawal signs were significantly reduced by high-frequency (100 Hz) EA administered on the hind limb acu-points St 36 and Sp 6 (49). This effect was much greater than that induced by low-frequency (2 Hz) stimulation. On the basis of these results, EA was applied to individuals addicted to heroin and obtained very promising results. However, it was inconvenient for patients to go to the clinic for treatment several times a day. As a result, they missed sessions, thus affecting the therapeutic outcome. One possible solution was to have patients treat themselves by using acupoints stimulation without a needle but still under the control of a physician. To overcome this problem, Han et al. developed a constant current electrical stimulator: Han’s Acupoint Nerve Stimulator (HANS).
Experiments in the rat using HANS showed that electrical stimulation applied at the surface of the skin over acupoints can produce an analgesic effect similar to that produced by EA (50). Satisfactory results were obtained using this transcutaneous electrical acupoint stimulation (TEAS) by HANS for the treatment of heroin withdrawal syndrome in humans (51). Later, the method was shown to suppress CPP, an animal model of craving for drugs of abuse for morphine in rats (52). Subsequent human studies revealed that this form of stimulation could indeed suppress craving in heroin-dependent patients.
OPIOID DETOXIFICATION WITH TRANSCUTANEOUS ELECTRICAL ACUPUNCTURE STIMULATION
Animal Studies
Systematic studies have revealed that the mechanism of acupuncture analgesia is attributed mainly to the increased release of endogenous opioid peptides in the central nervous system (CNS) (46). A rational extrapolation would be that the activation of the endogenous opioid system by acupuncture should ease opioid withdrawal symptoms.
Transauricular electrostimulation was reported to suppress the naloxone-induced morphine withdrawal syndrome in mice (53) and rats (54). Auriacombe et al. (55) demonstrated that transcutaneous electro nerve stimulation with an intermittent high-frequency current effectively attenuated signs in the rat after abrupt cessation of morphine; the mechanism remains obscure. Based on the findings that low-frequency EA (2 Hz) accelerated the release of β-endorphin and enkephalin in the CNS, whereas high-frequency EA (100 Hz) accelerated the release of dynorphin (48,56) in the spinal cord, the effect of EA was tested in naloxone-precipitated morphine withdrawal in the rat. Because the effect of 2 Hz EA is to accelerate the release of the morphine-like opioid peptides enkephalin and endorphin, it was predicted that 2 Hz would be more effective than 100 Hz in replacing morphine and ameliorating the abstinence syndrome. However, 2 Hz was only marginally effective in reducing two of five withdrawal signs, whereas 100 Hz suppressed all five signs (49).
Human Studies
To observe the effect of TEAS on the withdrawal syndrome in heroin-dependent patients, the method was applied for 30 minutes once a day for 10 days in an addiction treatment center (51). In addition to a standard questionnaire, two objective parameters were measured—heart rate and body weight.
Single Treatment
To observe the immediate effect on heart rate, the two pairs of output leads were placed on four acupoints in the upper extremities: one pair at Hegu (LI4) on the dorsum of the hand and on the palmar aspect of the hand opposite to LI4 Laogon, P-8) to complete the circuit, the other pair at Neiguan (PC6) on the palmar side of the forearm 2 inches above the palmar groove between the two tendons, and Waiguan (TE5) on the opposite side of PC6. A dense-and-disperse (DD) mode of stimulation was administered, with 2 Hz alternating automatically with 100 Hz, each lasting 3 seconds. This mode was shown to release four of the opioid peptides in the CNS (48), thus producing maximal therapeutic effect. The control group received the same placement of electrodes, which were disconnected from the circuitry. The average heart rate of the abstinent individuals was 109 beats per minute before treatment. DD stimulation for 30 minutes reduced the heart rate significantly, as shown in Figure 29-5. Reduction occurred within the first 5 to 10 minutes, continued for 20 minutes, and plateaued at 90 per minute in the last 10 minutes. The aftereffect remained for 20 minutes, after which the heart rate began to return to the original level (57).
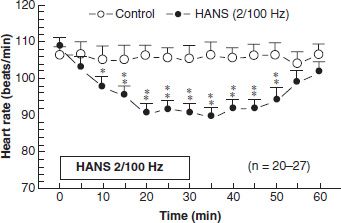
FIGURE 29-5 Effects of 2/100 Hz electric stimulation (HANS) on the heart rate of heroin-dependent individuals during episodes of withdrawal. *,** represent p < 0.05 and p < 0.01, respectively, compared with control groups. (Reprinted with permission from Han JS, Trachtenberg AI, Lowinson JH. Acupuncture. In: Lowinson JH, et al., eds. Substance abuse: a comprehensive textbook. Philadelphia, PA: Lippincott Williams & Wilkins, 2004:743–782.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


