Patient Story
A 78-year-old white woman presents with loss of central vision that has gradually worsened over the last 6 months. Fully independent before, she can no longer drive and has difficulty with activities of daily living. Her peripheral vision remains normal. Funduscopic examination reveals macular depigmentation and drusen (yellowish-colored subretinal deposits on the macula) (Figure 23-1). She is diagnosed with dry, age-related macular degeneration. After her physician discusses the available information about antioxidants and therapeutic options, she decides to start antioxidants and see an ophthalmologist to discuss laser, surgical, or medical treatments.
Introduction
Age-related macular degeneration (AMD) causes central vision loss in elderly patients. The pathophysiology of AMD is incompletely understood, but involves chronic changes in the retina and retinal pigment epithelium mediated by environmental and genetic factors. AMD is diagnosed by ophthalmoscopic detection of drusen. Healthy lifestyle decreases the risk of development and progression of AMD. Refer patients to an ophthalmologist to evaluate for intravitreal injections, laser photocoagulation or photodynamic therapy, or surgery.
Epidemiology
- Prevalence of advanced AMD is 1.4% in patients older than 40 years of age and 15% in white women older than 80 years of age.1
- AMD that causes significant vision loss is more common in whites than blacks or Hispanics.2
- Smoking increases risk in women (relative risk [RR] 2.5 for current smokers; 2.0 for former smokers).2
- AMD aggregates in families, but the specific genetic and familial risk factors are not clear.2
Etiology and Pathophysiology
AMD affects central but not peripheral vision. Environment and genetic attributes increase risk of these pathologic changes with aging.3
- Oxidative stress from the buildup of free oxygen radicals causes retinal pigment epithelial (RPE) injury.
- RPE injury evokes a chronic inflammatory response. The complement system is involved and specific polymorphisms of complement genes are associated with advanced disease and progression.4
- RPE injury/inflammation forms an abnormal extracellular matrix (ECM), which alters diffusion of nutrients to the retina and RPE.
- The abnormal ECM and diffusion leads to retinal atrophy and new vessel growth.
Risk Factors
- For advanced AMD, strong risk factors are age, current cigarette smoking, previous cataract surgery (replaced lens provides less eye protection from sunlight), and family history of AMD.
- Moderate risk factors include higher body mass index, history of cardiovascular disease, hypertension, and high plasma fibrinogen.
- Weak or inconsistent risk factors include gender, ethnicity, diabetes, iris color, history of cerebrovascular disease, total cholesterol, high-density lipoprotein, and triglyceride levels.5
Diagnosis
Diagnosis is made by ophthalmoscopy. AMD can be dry (early, intermediate, or advanced) or wet (always considered advanced).
- Early dry—May have no vision change; drusen present (Figure 23-2).
- Intermediate dry—Distortion in the center of vision; multiple medium-size drusen (see Figure 23-1).
- Advanced dry—(Nonexudative) Significant central vision loss from breakdown of support tissues around the macula.
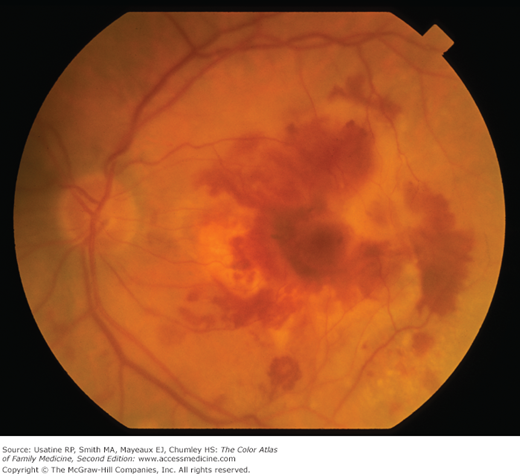
- Advanced wet—(Exudative) Gradual or sudden significant loss of vision; new onset of distortion in vision (straight lines appear wavy); abnormal blood vessels grow under the macula and can cause hemorrhage (Figure 23-3). Late changes include subretinal scarring and retinal atrophy (Figure 23-4).