, Arthur H. Cohen2, Robert B. Colvin3, J. Charles Jennette4 and Charles E. Alpers5
(1)
Department of Pathology, Microbiology and Immunology, Vanderbilt University Medical Center, Nashville, Tennessee, USA
(2)
Department of Pathology and Laboratory Medicine, Cedars-Sinai Medical Center, Los Angeles, California, USA
(3)
Department of Pathology Harvard Medical School, Massachusetts General Hospital, Boston, Massachusetts, USA
(4)
Department of Pathology and Laboratory Medicine, University of North Carolina, Chapel Hill, North Carolina, USA
(5)
Department of Pathology, University of Washington, Seattle, Washington, USA
Abstract
Acute interstitial nephritis (AIN) may be the result of indirect injury by drugs, reaction to systemic infections, direct renal infection (viral and selected bacteria), humoral immune responses (anti-tubular basement membrane disease), hereditary and metabolic disorders, and obstruction and reflux in the acute stages. Similar changes can also be observed in the kidney in systemic diseases such as lupus erythematosus and in transplant rejection. Acute tubulointerstitial nephritis also occurs to varying degrees in association with glomerulonephritides. This section is largely confined to the drug-induced, reactive, idiopathic, and immunologic disorders inducing AIN. Acute interstitial nephritis usually presents with acute renal failure, often oliguric; it is sometimes associated with systemic manifestations, such as arthralgia, fever, eosinophilia, and rash, typically as a consequence of drug hypersensitivity [1–3].
Introduction/Clinical Setting
Acute interstitial nephritis (AIN) may be the result of indirect injury by drugs, reaction to systemic infections, direct renal infection (viral and selected bacteria), humoral immune responses (anti-tubular basement membrane disease), hereditary and metabolic disorders, and obstruction and reflux in the acute stages. Similar changes can also be observed in the kidney in systemic diseases such as lupus erythematosus and in transplant rejection. Acute tubulointerstitial nephritis also occurs to varying degrees in association with glomerulonephritides. This section is largely confined to the drug-induced, reactive, idiopathic, and immunologic disorders inducing AIN. Acute interstitial nephritis usually presents with acute renal failure, often oliguric; it is sometimes associated with systemic manifestations, such as arthralgia, fever, eosinophilia, and rash, typically as a consequence of drug hypersensitivity [1–3].
General Pathologic Findings
On gross examination, kidneys with AIN are enlarged with a pale cortex and a distinct corticomedullary junction. Histologically, there is diffuse interstitial edema with an interstitial infiltrate of lymphocytes, monocyte macrophages, and plasma cells to varying degrees (Fig. 13.1). Eosinophils may comprise from 0 to 10 % of the infiltrate, depending on the etiology of the AIN. When there are many eosinophils, they may be focally concentrated (Fig. 13.2). The inflammatory cells are often prominent at the corticomedullary junction and are generally confined to the cortex. Neutrophils and basophils are infrequent; large numbers of neutrophils suggest a diagnosis of acute infectious interstitial nephritis. In some cases, granulomas may be found in the interstitium or around ruptured tubules. Glomeruli and vessels are usually uninvolved. The inflammation extends into the walls and lumina of tubules (tubulitis), with distal tubules more often affected than proximal tubules. There are varying numbers of degenerating and regenerating tubular epithelial cells; occasionally desquamated cells may be observed in tubular lumina. Proximal tubules often have focal loss of brush border staining. Immunofluorescence studies are usually negative but infrequently reveal granular deposits of complement in the tubular basement membranes (TBMs) and rarely fibrin in the interstitium. In cases of anti-TBM antibody formation, there is linear staining of TBMs for immunoglobulin G (IgG).
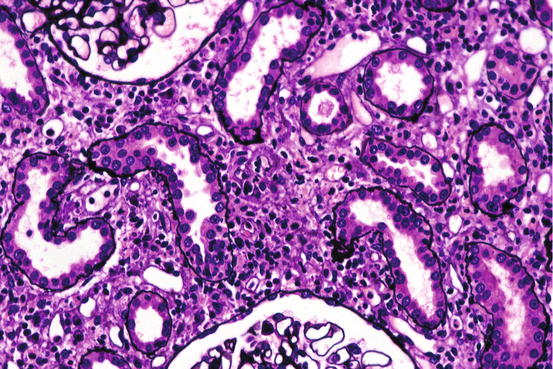
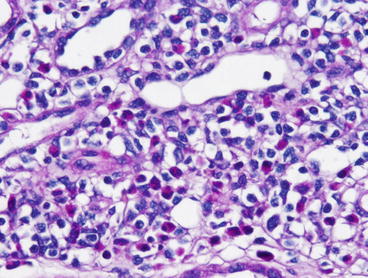
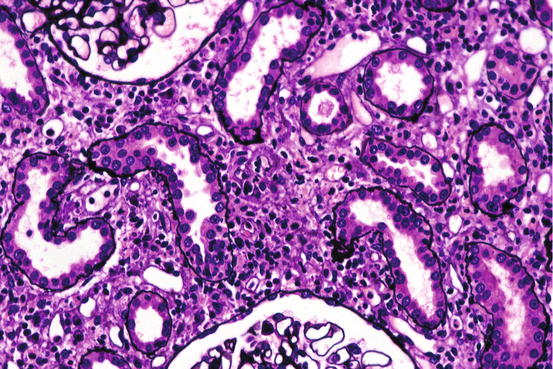
Fig. 13.1
The interstitium is edematous (tubules with normal basement membranes are separated) and infiltrated by lymphocytes, some of which are in the walls of tubules [periodic acid-Schiff (PAS) stain]
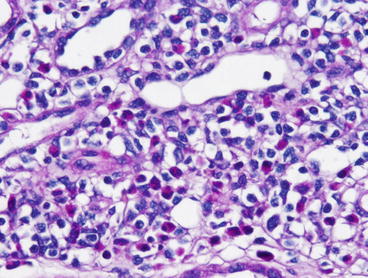
Fig. 13.2




There are numerous eosinophils in the interstitium along with lymphocytes and edema (H&E)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


