Abdominal Wall Incisions and Repair Including Release
Stephen R.T. Evans
Parag Bhanot
Introduction
The success of any open abdominal operation requires adequate exposure via the appropriate selection of the incision as well as proper closure of the abdominal wall to limit unnecessary morbidity. In the current era of laparo-endoscopic surgery, the general surgeon must still be well versed with the anatomic principles of the abdominal wall. In the past several decades, there has been a broadening of the options available in selecting an incision for an abdominal operation. The primary factors that should be considered are the diagnosed intra-abdominal disease and the organ(s) that must be modified or removed to treat that disease process. Nevertheless, even among experienced surgeons, there are frequently differences of opinion about the best incision for treating a given disease in a particular patient.
There are three primary requirements for an incision to be used for any given operation. The incision must provide optimal exposure, be flexible, and allow for a reliable closure.
Exposure must be optimal. The incision must provide direct access to the peritoneal cavity without significant limitations if additional exposure is needed at a later point. There must be adequate visualization of the diseased organ or injured area, and provide sufficient working space so that the procedure can be performed directly and rapidly without limiting the intra-abdominal manipulation or excision, especially important in the trauma setting. Appropriate positioning of the patient (e.g. lithotomy for pelvic surgery) and application of abdominal wall retractors are ancillary measures. Inadequate lighting can make even a simple procedure very difficult; thus, headlights and lighted retractors should be readily available.
Flexibility is a requirement of any operative incision. The popularity of the vertical midline incision is partly based on its ability to be extended if the scope of the operation dictates a larger incision. The limitations of the vertical incision are the xiphoid process and the pubis symphysis. To some extent, transverse incisions are also amenable to a curvilinear extension. Of concern, is the innervation of the abdominal musculature should be minimally interfered with to preserve its functionality. This is a limitation with oblique and transverse incisions. Ideally, it is best to sacrifice less than one segmental nerve trunk ipsilaterally, regardless of the length of the incision. An incision should be so placed that it does not interfere with future stages of planned surgery.
A reliable closure must be obtained, unless postoperative intra-abdominal hypertension (IAH) is a concern. The integrity of the abdominal wall must be maintained with adequate fascial closure. In cases involving contamination, such as a perforated viscus, we advocate delayed closure of the skin to minimize postoperative soft tissue infections.
The morbidity from abdominal incisions is poorly reported and probably underestimated. Any error, such as a poorly placed incision and/or unsatisfactory method of closure can lead to complications including hematoma, stitch abscess, infection, wound dehiscence or evisceration, incisional hernia, or an unsightly scar. Rarely, a misdiagnosis may necessitate making a different incision altogether.
Types of Incisions
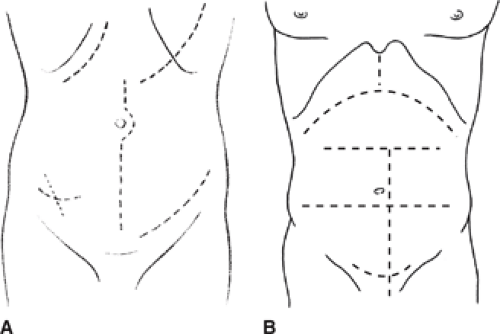
Figure 1 illustrates some common types of abdominal incisions.
Vertical. These incisions may be midline, paramedian, or even pararectus. They can be supraumbilical or infraumbilical and, if necessary (e.g. for extensive intra-abdominal trauma) can be extended in the midline upward to the xiphoid process and/or downward to the symphysis pubis.
Transverse or oblique. The best examples of these incisions are Kocher’s subcostal incision for cholecystectomy, a supraumbilical or infraumbilical transverse incision for intestinal surgery, McBurney’s or the Rockey-Davis’ incision for appendectomy, Pfannenstiel incision for gynecologic surgery, and a transverse or oblique central and lateral incision for exposure of the colon.
Retroperitoneal and extraperitoneal approaches. These incisions are ideal for surgery of the kidney or adrenal gland, renal transplantation, and aortoiliac surgery.
Thoracoabdominal. This incision gives excellent exposure of the upper abdominal organs by connecting the mediastinum, pleural, and peritoneal cavities into a single operative field.
Separate thoracic and abdominal incisions. These incisions spare the costal margin and cause less postoperative pain and disability than does the thoracoabdominal incision, as in an Ivor-Lewis esophagectomy.
Selection of the Incision
The choice of incision varies with the surgeon’s experience and preferences. Integral to the decision is the organ(s) or site that needs to be exposed, whether rapid access is needed as for severe hemorrhage or trauma, the certainty of the diagnosis, body habitus, the presence of previous abdominal incisions, and cosmesis.
Many surgeons prefer oblique or transverse incisions when adequate exposure can be obtained because the direction of pull of the lateral abdominal muscles is parallel to the incision, and much less distracting tension occurs on the wound edges than with vertical incisions. The wounds are stronger and less liable to dehiscence or herniation; in general, they seldom dehisce unless infection is present. However, these are somewhat more time-consuming to make than a midline incision. Also noteworthy is that they cause somewhat less postoperative pain than does an upper midline incision.
In emergency operations for major intra-abdominal hemorrhage, the midline approach gives the most rapid access and, if necessary, can be quickly extended from the xiphoid to the symphysis pubis. In general, an upper midline incision may be preferable in a thin patient with a very narrow costal angle, but in a patient with a wide costal angle, a unilateral or bilateral subcostal or transverse incision gives excellent exposure of upper abdominal viscera, especially the pancreas, liver, biliary tract, or spleen.
The McBurney or Rockey-Davis muscle-splitting incision for appendectomy is ideal and can be easily extended medially or obliquely laterally (Weir extension) if greater exposure is required. If an ileostomy or colostomy is to be part of an operative procedure, the main incision should be kept as far from the stoma as possible, with use of either a midline incision or even a paramedian approach on the opposite side from the planned stoma. Transverse incisions above the umbilicus provide ample room for an infraumbilical stoma, or vice versa.
When reoperating on the abdomen, the surgeon should, if possible, enter through the previous incision, particularly if the surgery entails excision of a disfiguring scar or repair of an incisional hernia. When operating through a previous scar, one must be wary of adhesions from bowel or omentum. The surgeon should never make a new incision closely parallel to a previous one because it may cause ischemia of the tissue between the incisions and lead to necrosis of the intervening skin and fascia.
Vertical Incisions
Midline Incision
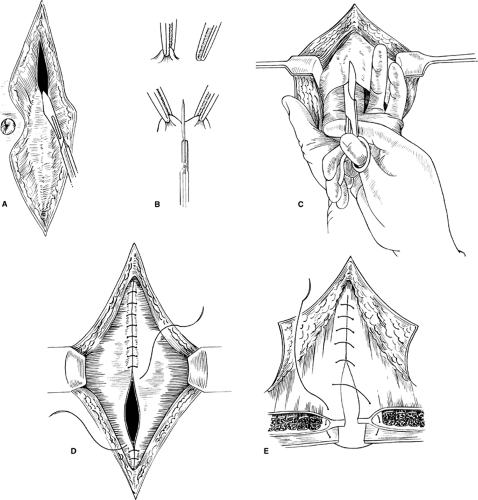
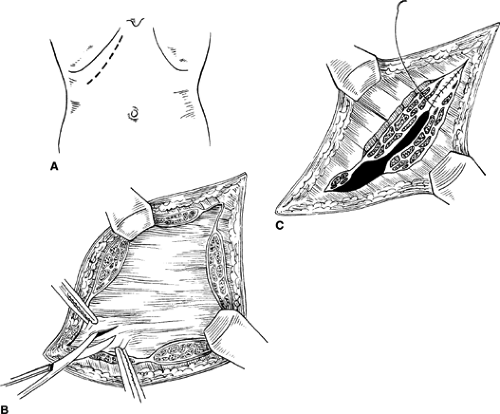
The midline incision provides the fastest and simplest approach making it a popular incision. It offers adequate exposure to any part of the abdominal cavity including the retroperitoneum. When speed is essential, it is clearly the incision of choice because it can be made and closed rapidly. It is almost avascular, allows for preservation of muscle fibers, and avoids nerve injury. It can be extended upward and downward the full length of the abdomen by curving the skin incision around the umbilicus (Fig. 2A). The incision is deepened through skin, subcutaneous fat, linea alba, properitoneal fat, and peritoneum. Properitoneal fat is abundant in obese individuals, and medium-sized vessels may be encountered. If the falciform ligament is encountered or is found interfering with exposure in the upper abdomen, it should be clamped, divided, and ligated. Upper midline incisions provide adequate exposure for most operations on the esophageal hiatus, abdominal esophagus (and vagus nerves), stomach, duodenum, gallbladder, pancreas, and spleen. Lower midline incisions provide good exposure for operations for the sigmoid colon and rectum, as well as all the pelvic organs.
When making vertical abdominal incisions, one should enter the peritoneum near the umbilicus to avoid injury to the bladder. Care must be exercised in opening the peritoneum to avoid injury to an underlying bowel loop, particularly when the bowel is distended in the setting of a bowel obstruction. A safe method is to pick up a fold of peritoneum with a pair of forceps, palpate it to ensure that no other structure has been caught up with it, and then carefully incise the raised fold with a scalpel or scissors (Fig. 2B). The small opening is enlarged to admit two fingers, which are used to protect viscera while the peritoneum is being opened throughout the length of the incision (Fig. 2C). When operating through a previous incision, one must be extra careful to avoid underlying adhesions involving bowel. If possible, the incision should begin 2 to 3 cm beyond the previous scar so that the peritoneum can be opened where it is relatively free of adhesions. Once the peritoneum has been opened, the fascia and peritoneum are held up with Kocher’s clamps so that the attachments of adhesions can be seen and carefully divided sharply to prevent thermal injury to the bowel.
When making the incision in the lower anterior abdominal wall, the surgeon must be careful to avoid a bladder injury. The bladder should always be decompressed by a Foley catheter. The anterior fascia can be incised to the pubic symphysis if needed, but the posterior incision involving the peritoneum should be angled away from the bladder. Blunt dissection in the space of Retzius can also be used to safely sweep the dome of the bladder away from the incision.
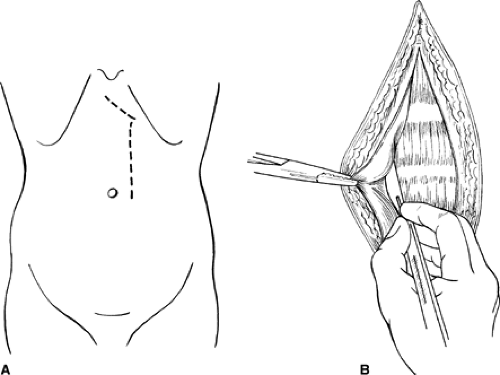
Paramedian Incision
A paramedian incision is a vertical incision made 2.5 to 4.0 cm from the midline (Fig. 3A). It is deepened through the subcutaneous fat onto the anterior rectus sheath, which is opened for the whole length of the wound no more than 2 to 3 cm from the midline (Fig. 3B). The medial portion of the anterior rectus fascia is then dissected off the muscle to the medial edge of the muscle. This dissection is more difficult in the upper abdomen because of the tendinous attachments (inscriptions) of the rectus muscle to the anterior fascia. These are located just below the xiphoid, at the umbilicus, and occasionally midway between these two points. Segmental blood vessels are encountered when the tendinous inscriptions are freed and must be electrocoagulated or clamped and ligated. Once the muscle is free anteriorly and medially, it can be retracted laterally by a ribbon retractor because it is not adherent to the posterior fascia. The posterior sheath and the peritoneum are then incised vertically for the length of and in line with the skin incision. The lower rectus sheath differs from the upper in two respects: the posterior fascial layer is largely absent below the semicircular line of Douglas, and the deep inferior epigastric vessels need to be divided and ligated as they run across the lower part of the incision.
The paramedian incision avoids injury to nerves, limits trauma to the rectus muscle, allows an anatomical and secure closure, and permits good restoration of abdominal wall function. If necessary, it can be extended from the pubis to the xiphoid by slanting the upper end of the incision medially toward the xiphoid. When placed on the appropriate side, it can be used satisfactorily for any intra-abdominal surgery, although it is more time-consuming to make than a vertical midline incision. The theoretical advantage of this incision is that the rectus muscle resumes its original place and splints the incisions in the anterior and posterior sheath, and thus should diminish the risk of wound dehiscence and incisional hernia. However, despite the known hernia incidence with midline incisions, the paramedian incision is less commonly employed because it is more time-consuming.
Vertical Muscle-Splitting Incision
The vertical muscle-splitting incision is performed in much the same way as the paramedian incision except that the rectus muscle is split longitudinally in its medial third, after which the posterior rectus sheath and peritoneum are opened in the same line. If the incision is short, it can be quickly made and repaired. It is very satisfactory when a limited incision is needed, for example, for placement of a Tenckhoff peritoneal dialysis catheter. An extensive incision should be avoided, however, because it results in more injury to nerves and muscle, and in substantially more bleeding than the midline or even the paramedian incision. If more than two nerves are sacrificed, the corresponding area of the abdominal wall may become dysfunctional postoperatively. The main value of this incision is in reopening the scar of a previous paramedian incision, when dissecting the rectus muscle from scar tissue in its sheath is very difficult and splitting the muscle may therefore be preferable.
Transverse or Oblique Incisions
There are several variations of transverse or oblique incisions (Fig. 1). Transverse incisions may be truly horizontal or may curve to varying degrees. Similarly, oblique incisions may be straight or curved and may vary considerably in angle. The incision may be limited to the oblique muscles, may involve division of all or part of one rectus muscle, or may even encompass the entire width of both recti as in the bilateral subcostal incision.
Transverse or oblique incisions mostly follow Langer lines and give better cosmetic results than vertical incisions. Any nerve injury that occurs is usually limited to one or, rarely, two nerves. In general, transverse or oblique incisions give limited exposure if disease is found in both the upper and lower abdomen, except possibly in a short individual with a wide abdomen and a wide costal margin. In such a patient a long, transverse supraumbilical incision gives very satisfactory exposure for most intra-abdominal surgery with the exception of the deep pelvis. An infraumbilical incision, properly placed, is satisfactory for operation in the pelvis, for example, the sigmoid colon or rectum. However, the same transverse incision may not provide adequate exposure if mobilization of the splenic flexure is also required as in a left hemicolectomy.
The transverse tendinous inscriptions attach the rectus muscle to the anterior rectus sheath, thereby keeping it from retracting significantly when it is incised. Tendinous inscriptions do not occur below the umbilicus, however, some retraction of the incised rectus muscle may occur in that area. One should avoid making a transverse incision at or very close to the symphysis pubis because, if a hernia develops, sufficient fascia may not be available along the lower margin of the incision to permit satisfactory repair without bony fixation.
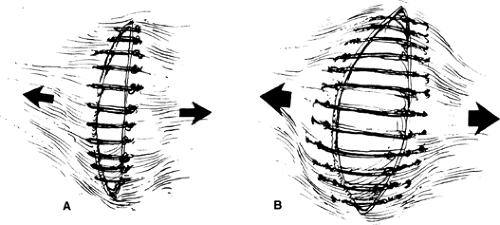
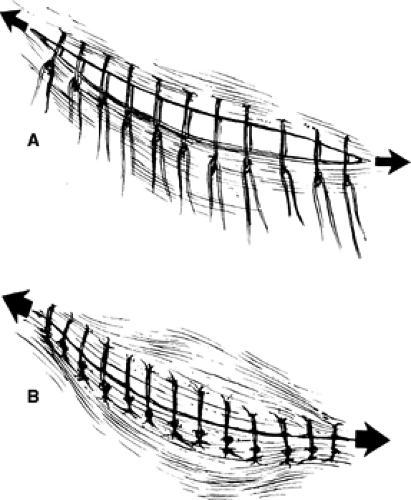
One should emphasize that transverse or oblique incisions have substantially more intrinsic strength than vertical incisions because fascial fibers are transversely oriented. When the incision is made, the fascia is incised parallel to the fibers. Closure of the incision places the sutures perpendicular to the fascial fibers making it more secure than in a vertical incision in which the sutures are parallel to the fiber orientation and can tear or cut through the fascia (Figs. 4 and 5). This is the reason that dehiscence or incisional hernia is three to five times as common with vertical incisions compared with transverse incisions.
Kocher’s Subcostal Incision
Frequently, a right subcostal incision is used for open operations in the gallbladder, liver, and biliary system, particularly in obese or muscular individuals with wide costal angles (Figs. 1 and 6). A left-sided subcostal incision is used mainly for elective splenectomy. A bilateral subcostal incision provides excellent exposure in the upper abdomen. It is useful for performing total gastrectomy in an obese individual, for anterior exposure of both adrenal glands, for major liver resections, for pancreatic operations, and for hepatic transplantation.
The standard subcostal incision starts in the midline 2.5 to 5.0 cm below the xiphoid and extends laterally approximately 2.5 cm below the costal margin for a variable distance, depending on the patient and the exposure required (Fig. 6A). If the liver is enlarged, the incision may have to be placed at a lower level. The incision should not be made too close to the costal margin because, if a hernia develops, enough abdominal wall fascia must be available at the upper margin to permit a satisfactory repair or bony fixation would be required to the ribs. After the anterior rectus sheath is incised, the rectus muscle is divided along the course of the wound; electrocautery is used to control branches of the superior epigastric artery and other blood vessels, or suture ligatures can be used. The lateral abdominal muscles can be divided for a variable distance. Although the eighth intercostal nerve is almost invariably divided, care must be taken to preserve the ninth nerve to prevent weakening of the abdominal musculature. The incision is then deepened to open the peritoneum (Fig. 6B). Although the rectus muscle is divided, this results in no weakening of the abdominal muscles, provided that the anterior and posterior sheaths are repaired because the incision generally cuts only one intercostal nerve. The rectus muscles have a segmental nerve supply, allowing a transverse or slightly oblique division without significant risk to its innervation. Healing of the incision simply results in an iatrogenically produced additional fibrous inscription in the muscle.
Transverse Incision
Transverse incisions are ideally suited for open operations on the small intestine and are usually performed through an infraumbilical transverse incision, located approximately 2 to 3 cm below the umbilicus. For
operations involving the proximal small intestine, the incision can be favored to the left of the midline. Right-sided transverse incisions provide excellent exposure for the distal small intestine, cecum, and the ascending colon to the midtransverse colon. For right colon operations, the incision is placed 2 to 3 cm above the umbilicus. If the left transverse colon or splenic flexure is to be operated, the mirror-image incision on the left is satisfactory. In either incision, it may be extended to the opposite side of the midline as far as is necessary to obtain adequate exposure in either right or left colon procedures. As previously noted, a transverse incision may be suboptimal in an extended left hemicolectomy when the splenic flexure requires mobilization with a pelvic anastomosis.
operations involving the proximal small intestine, the incision can be favored to the left of the midline. Right-sided transverse incisions provide excellent exposure for the distal small intestine, cecum, and the ascending colon to the midtransverse colon. For right colon operations, the incision is placed 2 to 3 cm above the umbilicus. If the left transverse colon or splenic flexure is to be operated, the mirror-image incision on the left is satisfactory. In either incision, it may be extended to the opposite side of the midline as far as is necessary to obtain adequate exposure in either right or left colon procedures. As previously noted, a transverse incision may be suboptimal in an extended left hemicolectomy when the splenic flexure requires mobilization with a pelvic anastomosis.
The layers of the abdominal wall to be incised are, for all practical purposes, the same as those described for the subcostal incision. In patients who are thin, especially those with a narrow costal margin, the straight transverse incision is frequently modified with the lateral end being placed in the same plane as the umbilicus, and the incision can be somewhat oblique superiorly so that the midline end of the incision is several centimeters above the umbilicus. If the incision needs to be extended across the midline for some distance, it then becomes a bilateral subcostal incision. In the event that it is necessary to enter the superior portion of the abdomen, a vertical extension in the midline can be utilized as far superiorly as the paraxiphoid area. The xiphoid process can be excised if additional exposure is required. This extension gives excellent exposure to the upper quadrants as necessary for operations close to the hiatus or for hepatic resections, especially in larger patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree