Abdomen
Cards 4-1 to 4-31
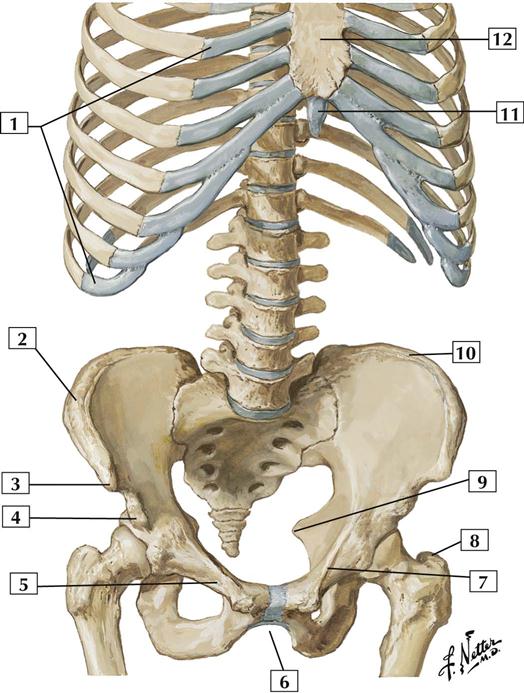
Bones and Joints
4-1 Bony Framework of Abdomen
Atlas Plate 243
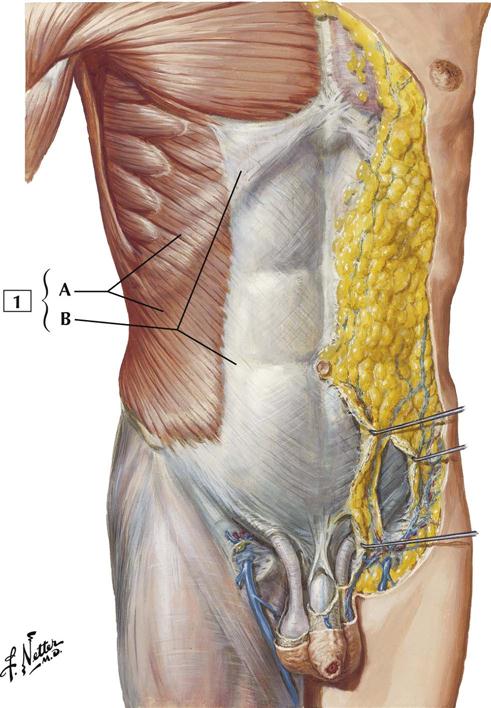
Muscles
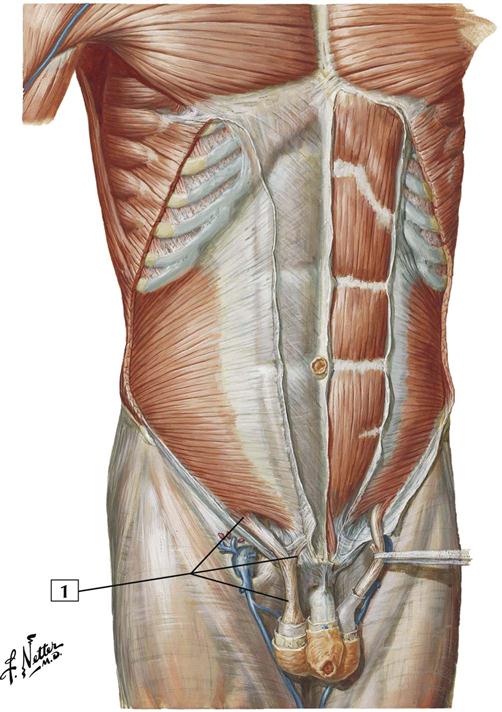
4-2 Anterior Abdominal Wall: Superficial Dissection
Origin:
Arises by fleshy digitations from the external surfaces and inferior borders of the lower 8 ribs.
Insertion:
The muscle attaches to the anterior half of the iliac crest, to the anterior superior iliac spine, and into a broad aponeurosis along a line from the 9th costal cartilage to the anterior superior iliac spine. The aponeurosis inserts into the midline linea alba.
Action:
Compresses the abdominal contents. Contracting bilaterally, the muscles flex the vertebral column or trunk. Acting alone, the muscle bends the vertebral column laterally and rotates it so as to bring the shoulder of the same side forward.
Innervation:
Supplied by intercostal nerves T7-11 and the subcostal nerve (T12).
Comment:
This is the largest and most superficial of the 3 flat abdominal muscles.
Atlas Plate 245
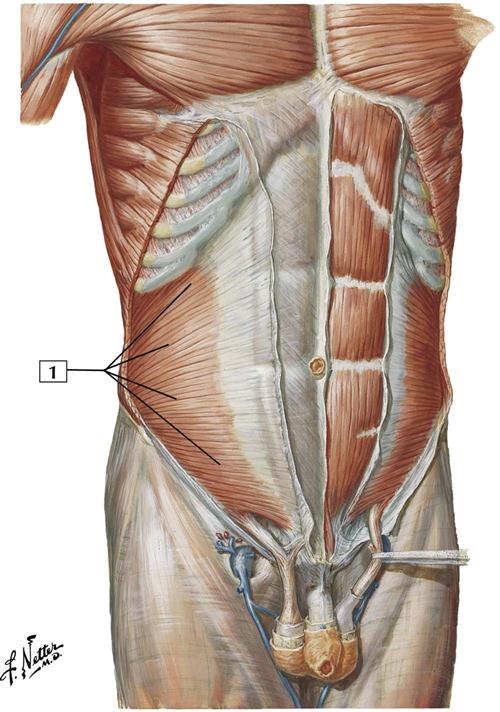
4-3 Anterior Abdominal Wall
Origin:
Arises from the lateral half of the inguinal ligament, the iliac crest, and the thoracolumbar fascia.
Insertion:
Attaches to the inferior borders of the cartilages of the last 3 or 4 ribs, the linea alba, the pubic crest, and the pectineal line.
Action:
Compresses the abdominal contents. Contraction of both internal oblique muscles flexes the vertebral column. Contraction on one side only bends the vertebral column laterally and rotates it, moving the shoulder of the opposite side anteriorly.
Innervation:
By the intercostal nerves T7-11, subcostal nerve (T12), and iliohypogastric and ilio-inguinal nerves (L1).
Comment:
In the inguinal region, the aponeuroses of the internal oblique and transverse abdominal muscles fuse to form the conjoint tendon.
Atlas Plate 246
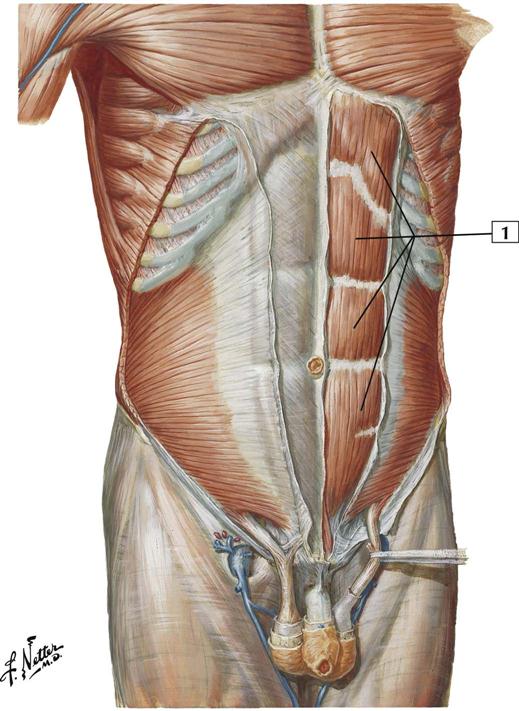
4-4 Anterior Abdominal Wall
Origin:
Arises inferiorly by 2 tendons. The lateral tendon is attached to the pubic crest, and the medial tendon interlaces with the tendon of the opposite side to arise from the pubic symphysis.
Insertion:
Attaches into the cartilages of the 5th, 6th, and 7th ribs and the xiphoid process.
Action:
Flexes the vertebral column or trunk, tenses the anterior abdominal wall, and depresses the ribs.
Innervation:
Intercostal nerves (T7-11) and the subcostal nerve (T12).
Comment:
The rectus abdominis muscle is contained in the rectus sheath and is separated from the rectus abdominis on the other side by the linea alba.
The muscle is crossed by fibrous bands, which are the 3 tendinous intersections; this gives the appearance of “6-pack abs.”
Atlas Plate 246
4-5 Anterior Abdominal Wall
Origin:
This thin muscle arises from the middle of the inguinal ligament and is a continuation of the internal abdominal oblique muscle.
Insertion:
Attaches by a small tendon to the pubic tubercle and crest.
Action:
Draws the testes upward.
Innervation:
Genital branch of the genitofemoral nerve (L1 and L2).
Comment:
After passing through the inguinal ring, the muscle fibers of the cremaster form a series of loops that are embedded in the cremasteric fascia (surrounding the spermatic cord in a male).
The spermatic cord is covered by 3 fascial layers derived from the abdominal wall. The external spermatic fascia is derived from the external abdominal oblique aponeurosis; the middle spermatic (cremasteric) fascia, from the internal abdominal oblique muscle; and the internal spermatic fascia, from the transversalis fascia.
Atlas Plate 246
4-6 Anterior Abdominal Wall: Deep Dissection
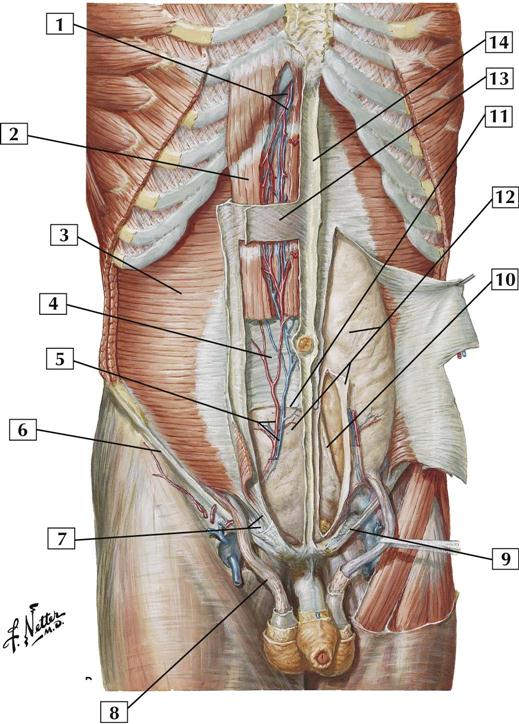
1. Superior epigastric vessels
3. Transversus abdominis muscle
4. Posterior layer of rectus sheath
5. Inferior epigastric vessels
6. Inguinal ligament (Poupart’s ligament)
7. Inguinal falx (conjoint tendon)
8. Cremasteric muscle (middle spermatic fascia)
9. Lacunar ligament (Gimbernat’s ligament)
10. Medial umbilical ligament (occluded part of umbilical artery)
11. Arcuate line
13. Anterior layer of rectus sheath
14. Linea alba
Comment:
Above the arcuate line, the anterior layer of the rectus sheath comprises the fused aponeuroses of the external and internal abdominal oblique muscles, whereas the posterior layer comprises the fused aponeuroses of the internal abdominal oblique and transversus abdominis muscles. Below the arcuate line, the aponeuroses of all 3 muscles fuse to form the anterior layer of the sheath; and the rectus abdominis muscle rests only on the thin transversalis fascia.
Atlas Plate 247
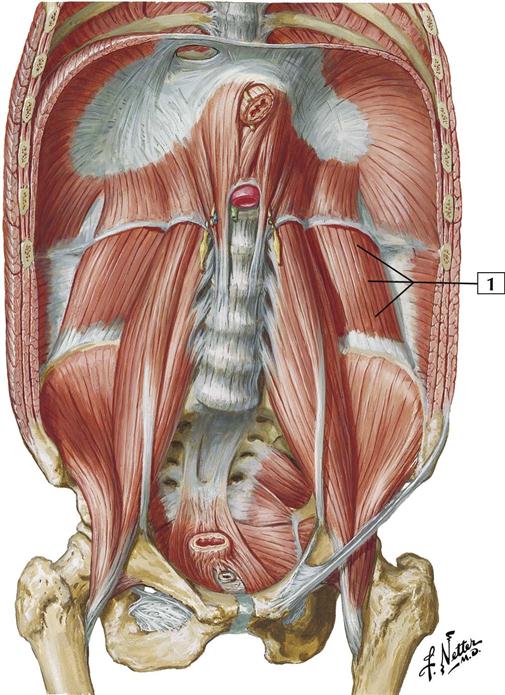
4-7 Posterior Abdominal Wall: Internal View
Origin:
Arises from the transverse processes of L3-5, the iliolumbar ligament, and the iliac crest.
Insertion:
Attaches to the lower border of the last rib and the transverse processes of L1-3 vertebrae.
Action:
With the pelvis fixed, this muscle laterally flexes the lumbar vertebral column (trunk). It also fixes the 12th rib during inspiration. When both quadratus lumborum muscles act together, they can help extend the lumbar vertebral column.
Innervation:
Subcostal nerve (T12 and L1-4 nerves).
Comment:
Superiorly, the diaphragm forms the lateral arcuate ligament (lumbocostal arch) where it passes over the quadratus lumborum.
Atlas Plate 258
See also Plate 192
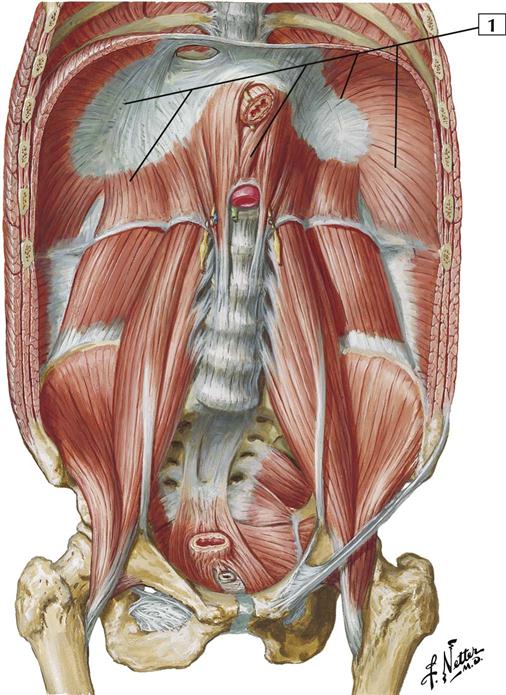
4-8 Posterior Abdominal Wall: Internal View
Origin:
This dome-shaped musculofibrous septum arises from the circumference of the thoracic outlet, with fibers arising from a sternal portion (xiphoid process), a costal portion (lower 6 costal cartilages), and a lumbar portion (L1-3 vertebrae).
Insertion:
The muscles converge and insert into the central tendon.
Action:
Attached to the ribs and lumbar vertebrae, the muscular diaphragm draws the central tendon downward and forward during inspiration. This increases the volume of the thoracic cavity and decreases the volume of the abdominal cavity.
Innervation:
Phrenic nerve (C3, C4, and C5).
Comment:
The diaphragm has 3 large openings: the caval hiatus for the inferior vena cava (at the level of the T8 vertebra), the esophageal hiatus (at the level of the T10 vertebra), and the aortic hiatus (in front of the T12 vertebra).
Where the diaphragm passes over the aorta, it forms an arch called the median arcuate ligament. As the diaphragm passes over the psoas major muscle, it forms the medial arcuate ligament; and where it passes over the quadratus lumborum, it forms the lateral arcuate ligament.
Atlas Plate 258
See also Plate 192
Nerves
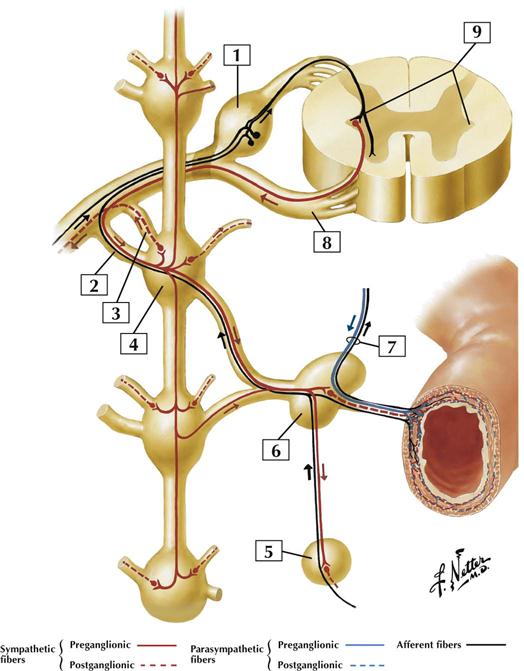
4-9 Autonomic Nerves and Ganglia of Abdomen
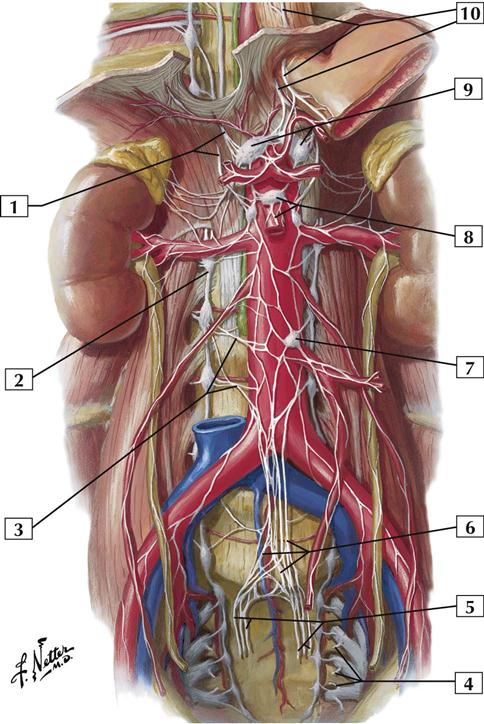
Comment:
Sympathetic and parasympathetic nerves innervate the viscera of the abdominal cavity. Sympathetic nerves coursing in the thoracic splanchnic nerves (from T5-12 spinal cord levels) and lumbar splanchnics (upper lumbar levels) synapse largely in 3 major collections of ganglia: celiac, superior mesenteric, and inferior mesenteric ganglia. A nerve plexus continuing from this most inferior ganglion gives rise to the superior hypogastric plexus, which provides sympathetic innervation to pelvic viscera.
Parasympathetic innervation to the upper two thirds of the abdominal viscera (derived from the foregut and midgut portions of the embryonic gut) comes from the vagus nerve. The remaining portions of the abdominal and pelvic viscera (embryonic hindgut) receive parasympathetics from S2, S3, and S4 via pelvic splanchnic nerves.
Most of these autonomic fibers reach the viscera by traveling on the blood vessels originating from the celiac trunk and the superior and inferior mesenteric arteries.
Atlas Plate 297
4-10 Autonomic Reflex Pathways: Schema