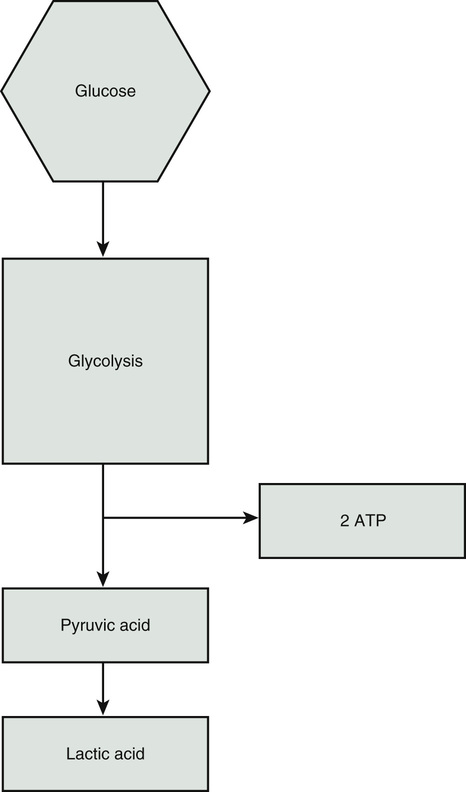
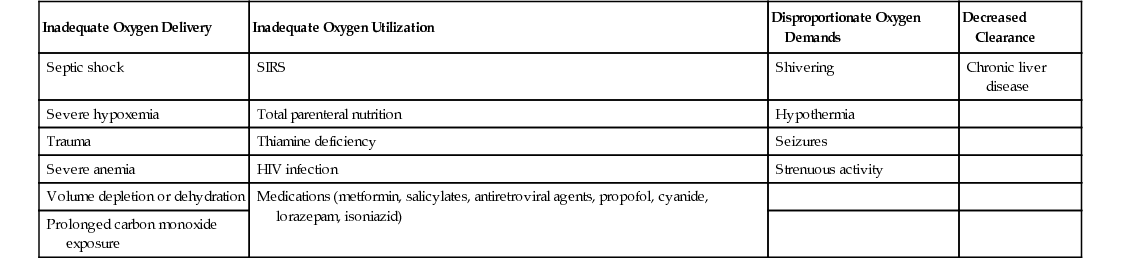
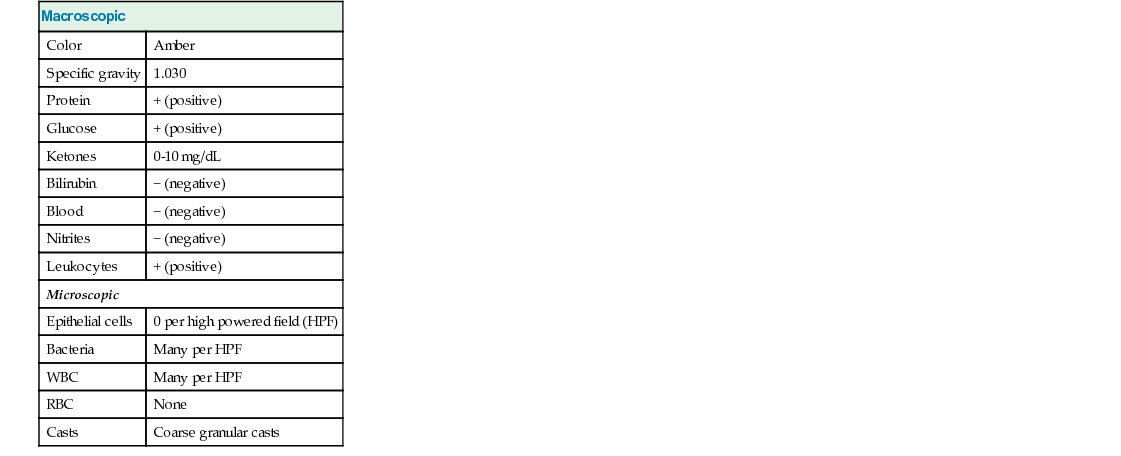
Aarti Chawla Mittal, Walter Chou, Raj Dasgupta, Joe Crocetti Orthostatic hypotension, or postural hypotension, is low blood pressure that causes symptoms only when the patient is in an upright position. This happens because when upright, there is pooling of blood in the lower extremities and splanchnic bed, which decreases venous return, thus dropping cardiac output and blood pressure. This is what causes the symptom of dizziness or lightheadedness when upright. Normally, the baroreceptors in the arteries near the heart and neck sense the low blood pressure, which provokes increased sympathetic tone, which increases pulse rate, peripheral vascular resistance, and cardiac output, thus limiting the symptoms. Depending on the cause and if the symptoms are severe, the hypotension can lead to syncope. Etiologies for orthostatic hypotension are dehydration or problems with the cardiovascular, endocrine, or nervous systems. With the limited history, dehydration due to the patient’s fever is the most likely cause. All of the patient’s vital signs are abnormal and worrisome, except the oxygen saturation. These findings point to the systemic inflammatory response syndrome (SIRS), which is a nonspecific cytokine-mediated inflammatory state involving multiple organ systems of the body. SIRS is usually a response to an infection but can also be caused by ischemia, burns, or trauma. The differential diagnosis for this patient is very broad because SIRS is so nonspecific. Highest on the list is infection, as this is the most common cause of SIRS. Other possibilities also must be considered, such as pulmonary embolism, autoimmune disorders, pancreatitis, and substance abuse. Because the top differential diagnosis is infection and the patient complains of dysuria, it would be wise to start with a urinalysis and urine culture. To see if the patient has bacteremia, blood cultures should be ordered as part of the initial infectious workup. It is also wise to ask for a complete blood count (CBC) with a differential of the white blood cells. This will indicate whether the patient has any leukocytosis (or leukopenia) and bands. It is also possible to see whether the patient is anemic, which may explain her orthostatic hypotension. A basic metabolic panel will provide information regarding her general electrolytes, kidney function, and current glucose level. Given the high suspicion for infection, along with the patient’s hypotension, tachycardia, and tachypnea, it would also be prudent to order a serum lactate level. With her hypotension, the patient may not be adequately perfusing all of her organs and tissues. As cells become more hypoxic, they switch from aerobic to anaerobic metabolism for energy production. A by-product of the anaerobic pathway is a buildup of lactic acid (see Fig. 61.1). An elevated lactate level in someone with infection is something to be very concerned about. All elevated levels, however, are not due to infection. Table 61.1 shows various mechanisms and causes of elevated lactate levels.
A 43-Year-Old Female With Fevers
What are the potential causes of dizziness while sitting or standing that resolve when supine?
These vitals are concerning for what clinical syndrome?
What is your differential diagnosis?
What labs would you like to order and why?
How do you interpret these data?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


61 A 43-Year-Old Female With Fevers
Case 61