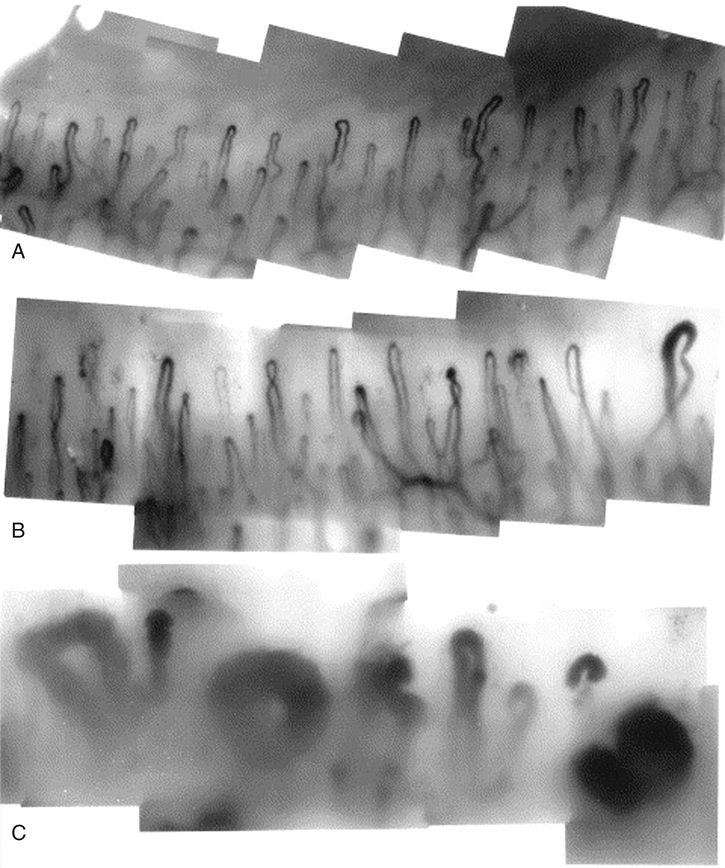
R. Michelle Koolaee The etiologies of weakness are very broad but can be narrowed down with the proper history. First, determine the location of the weakness (i.e., is the weakness focal or diffuse? Proximal versus distal? Ascending versus descending?). Inflammatory myopathies typically involve proximal more than distal muscles. Some neuromuscular diseases (i.e., Guillain-Barre syndrome) are characterized by an ascending pattern of weakness. Electrolyte and metabolic disturbances may present with more generalized weakness. Second, be sure to ask the duration of symptoms. Acute focal weakness, for instance, suggests etiologies such as stroke, infectious myopathies, and medication/toxin-related myopathies. Last, note the presence of constitutional symptoms such as fevers and unintentional weight loss; they can help determine whether the weakness is related to a paraneoplastic process. Proximal muscle weakness with associated skin changes raises an early suspicion for inflammatory myopathy, which should prompt you to ask some critical questions. These are highlighted in Table 60.1. TABLE 60.1 Critical Questions to Ask in Patients Where There Is Concern for Inflammatory Myopathy Nailfold capillaroscopy represents a way to analyze microvascular abnormalities in patients with autoimmune disease, with abnormalities seen classically in patients with scleroderma, dermatomyositis (DM), and mixed connective tissue disease (MCTD). Nailfold capillary loops are normally in a homogenous distribution just beneath the cuticle. Abnormal patterns include dilated and distorted nailfold capillary loops, loss of surrounding loop structures, and cuticle overgrowth. See Figure 60.1 for images of normal and abnormal nailfold capillary loops. There are three ways to examine the nailfold capillaries. A microcirculation microscope is a sophisticated instrument (resembling a traditional microscope) that transfers the image to a television monitor and can be used to measure the cross-section area of the microvessel, as well as the speed and the quantitative amount of blood flow. There are also portable capillaroscope devices that offer increased magnification and a strong light in order to view microvasculature. The most easily accessible and cost-effective means of viewing nailfold capillaries is through the use of the light of an ophthalmoscope (at around 20× magnification). Place some surgical lubricant on the nailfold capillary, just underneath the cuticle, and look through the ophthalmoscope to the nail (as you would normally use the ophthalmoscope), only in much closer proximity. This is a 65-year-old male presenting with progressive proximal muscle weakness, hypoxia with an interstitial radiographic pattern, rash, and elevated serum muscle enzymes. His chronic dyspnea on exertion, dry cough, hypoxia, lung exam with inspiratory rales, and interstitial pattern on chest radiograph are very suspicious for an underlying interstitial lung disease (ILD); computed tomography (CT) imaging of the lungs would be indicated to further evaluate the lung parenchyma.
A 65-Year-Old Male With Muscle Weakness
What questions are helpful to ask in anyone who complains of weakness?
What are the critical “red flags” to be aware of in someone with symptoms of myopathy?
Question
Reasoning
Do you have shortness of breath?
The diaphragm is a muscle that can be involved in inflammatory myopathies as well as some neuromuscular diseases. If severe, these patients can require mechanical ventilation. There should be a low threshold for inpatient admission for management of these respiratory issues, particularly if the symptoms are acute and severe.
Do you have difficulty swallowing?
Dysphagia can be a sign of oropharyngeal muscle weakness, which increases the risk for aspiration. This requires evaluation by a speech and swallow specialist and often warrants more aggressive immunosuppressive therapy.
Smoking history? Fevers? Unintentional weight loss? Age of the patient?
These questions risk-stratify the patient for a malignancy-associated process. Inflammatory myopathies are associated with a higher incidence of malignancy.
How do you examine the nailfold capillaries, and when is this of value?
What is your differential diagnosis at this point?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


60 A 65-Year-Old Male With Muscle Weakness
Case 60