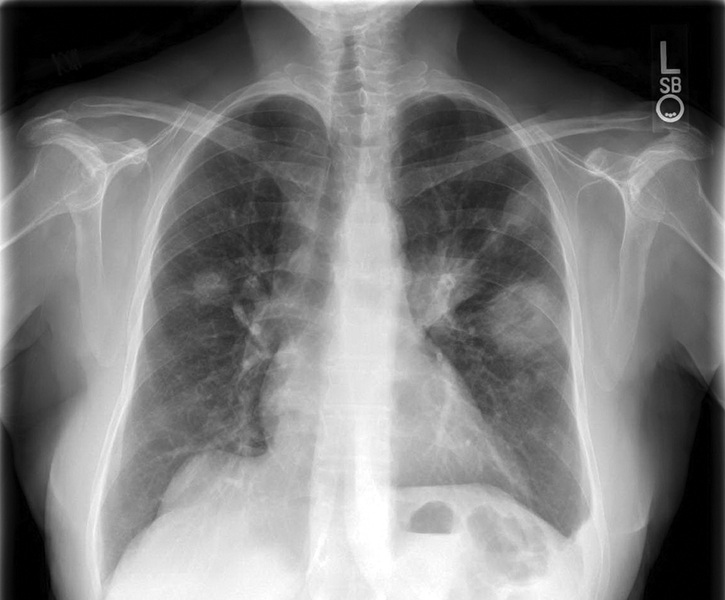
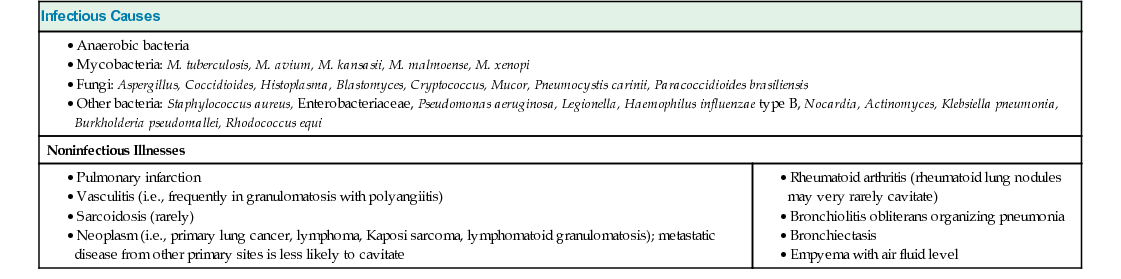
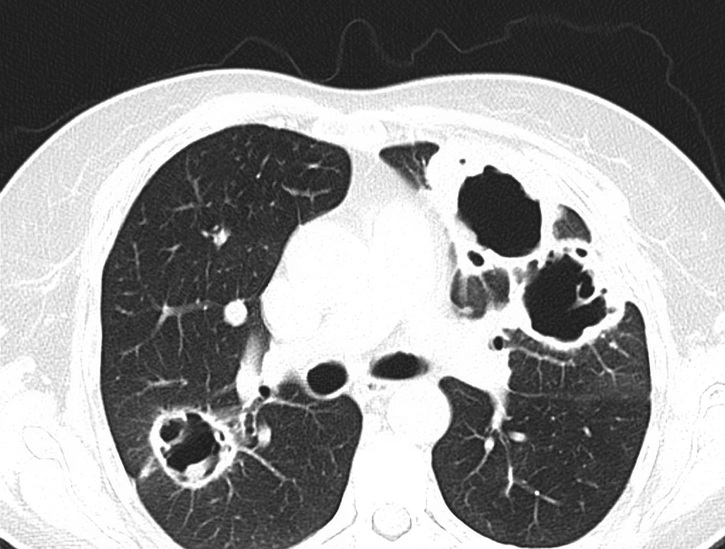
R. Michelle Koolaee There are various infectious and noninfectious causes of radiographic cavitary lung lesions, which are summarized in Table 53.1. Mycobacterium tuberculosis generally has the highest prevalence of cavities among persons with pulmonary disease of any infection because this pathogen causes extensive caseous necrosis (which leads to cavity formation). Lung abscess is another relatively common bacterial cause of cavitary lung lesions; this is usually polymicrobial. The most common noninfectious cause is pulmonary embolism with infarction; cavitary lesions occur as a result of pulmonary infarction and subsequent necrosis. Cavitary lung lesions in rheumatologic illness are relatively uncommon, with the exception of granulomatosis with polyangiitis (GPA), where this is a frequent finding. Vasculitis is defined by inflammatory infiltrate within the vessel walls, which can lead to compromise of vessel integrity, and subsequent tissue ischemia and necrosis. Affected vessels vary in size, type, and location. Vasculitis should be considered in situations where patients present with systemic symptoms along with either single or multiorgan disease involvement. There is no algorithmic approach to the vasculitides because disease manifestations are so variable. There are, however, classification criteria for most types of vasculitis proposed by the American College of Rheumatology. These criteria are most useful for clinical research purposes but may also often guide diagnostic evaluation. A detailed history and careful physical exam are essential in evaluating a patient with possible vasculitis. Also, be aware that the clinical manifestations of vasculitis can be mimicked by a number of other disorders (i.e., infection, malignancy, and other connective tissue diseases, to name a few). Although not sensitive or specific, some systemic symptoms of vasculitis may include fever, fatigue, neurologic dysfunction, respiratory dysfunction, renal insufficiency (with an active urine sediment), and abdominal pain. Radiographic findings are rarely definitive in establishing a diagnosis. Culturing respiratory specimens for bacteria, mycobacteria, and fungi is an appropriate first step in evaluating the etiology of a cavity; a bronchoscopy is typically performed in order to elicit this information (provided that the patient is hemodynamically stable). Supplemental testing (i.e., antigen and antibody tests for specific infectious organisms) is useful when focusing on specific infectious etiologies. Clinicians should pursue a tissue diagnosis when clinically warranted.
A 57-Year-Old Female With Cavitary Lung Lesions
What are some causes of cavitary lung lesions?
In general, when should you consider systemic vasculitis as a diagnosis?
What is the best way to elicit the cause of this patient’s cavitary lung lesions?