Chapter 10
The respiratory system
Respiratory bronchioles and alveoli
Ageing and the respiratory system
Disorders of the upper respiratory tract
10.1 Air distribution through the upper respiratory tract 242
10.2 Air distribution through the lower respiratory tract 242
10.3 Respiratory mucosa 243
10.4 Bronchi and bronchioles 252
10.6 Respiratory membrane 253
10.7 Role of the diaphragm in breathing 255
10.8 Pulmonary ventilation 256
10.9 External respiration 259
10.10 Internal respiration 259
This chapter describes the structure and functions of the respiratory system.
The cells of the body need energy for all their metabolic activities. Most of this energy is derived from chemical reactions, which can only take place in the presence of oxygen (O2). The main waste product of these reactions is carbon dioxide (CO2). The respiratory system provides the route by which the supply of oxygen present in the atmospheric air enters the body, and it provides the route of excretion for carbon dioxide.
The condition of the atmospheric air entering the body varies considerably according to the external environment, e.g. it may be dry or moist, warm or cold, and carry varying quantities of pollutants, dust or dirt. As the air breathed in moves through the air passages to reach the lungs, it is warmed or cooled to body temperature, saturated with water vapour and ‘cleaned’ as particles of dust stick to the mucus which coats the lining membrane. Blood provides the transport system for O2 and CO2 between the lungs and the cells of the body. Exchange of gases between the blood and the lungs is called external respiration and that between the blood and the cells internal respiration. The organs of the respiratory system are:
• nose
• pharynx
• larynx
• trachea
• two bronchi (one bronchus to each lung)
• bronchioles and smaller air passages
• two lungs and their coverings, the pleura
• muscles of breathing – the intercostal muscles and the diaphragm.
Figure 10.1 shows the organs of the respiratory system and associated structures. ![]() 10.1, 10.2
10.1, 10.2
The effects of ageing on respiratory function are described on p. 261, and important respiratory disorders on p. 262.
Nose and nasal cavity
Position and structure
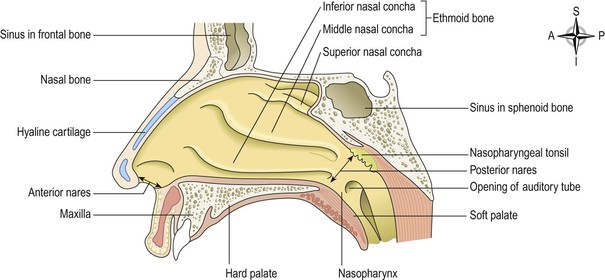
The nasal cavity is the main route of air entry, and consists of a large irregular cavity divided into two equal passages by a septum. The posterior bony part of the septum is formed by the perpendicular plate of the ethmoid bone and the vomer. Anteriorly, it consists of hyaline cartilage (Fig. 10.2).
The roof is formed by the cribriform plate of the ethmoid bone and the sphenoid bone, frontal bone and nasal bones.
The floor is formed by the roof of the mouth and consists of the hard palate in front and the soft palate behind. The hard palate is composed of the maxilla and palatine bones and the soft palate consists of involuntary muscle.
The medial wall is formed by the septum.
The lateral walls are formed by the maxilla, the ethmoid bone and the inferior conchae (Fig. 10.3).
The posterior wall is formed by the posterior wall of the pharynx.
Lining of the nasal cavity  10.3
10.3
The nasal cavity is lined with very vascular ciliated columnar epithelium (ciliated mucous membrane, see Fig. 10.12, respiratory mucosa) which contains mucus-secreting goblet cells (p. 249). At the anterior nares this blends with the skin and posteriorly it extends into the nasal part of the pharynx (the nasopharynx).
Openings into the nasal cavity
The anterior nares, or nostrils, are the openings from the exterior into the nasal cavity. Nasal hairs are found here, coated in sticky mucus.
The posterior nares are the openings from the nasal cavity into the pharynx.
The paranasal sinuses are cavities in the bones of the face and the cranium, containing air. There are tiny openings between the paranasal sinuses and the nasal cavity. They are lined with mucous membrane, continuous with that of the nasal cavity. The main sinuses are:
The sinuses are involved in speech (p. 248) and also lighten the skull. The nasolacrimal ducts extend from the lateral walls of the nose to the conjunctival sacs of the eye (p. 204). They drain tears from the eyes.
Respiratory function of the nose
The nose is the first of the respiratory passages through which the inspired air passes. In the nasal cavity, air is warmed, moistened and filtered. The three projecting conchae (Figs 10.3 and 10.4) increase the surface area and cause turbulence, spreading inspired air over the whole nasal surface. The large surface area maximises warming, humidification and filtering.
Warming.
The immense vascularity of the mucosa permits rapid warming as the air flows past. This also explains the large blood loss when a nosebleed (epistaxis) occurs.
Filtering and cleaning.
Hairs at the anterior nares trap larger particles. Smaller particles such as dust and bacteria settle and adhere to the mucus. Mucus protects the underlying epithelium from irritation and prevents drying. Synchronous beating of the cilia wafts the mucus towards the throat where it is swallowed or coughed up (expectorated).
Humidification.
As air travels over the moist mucosa, it becomes saturated with water vapour. Irritation of the nasal mucosa results in sneezing, a reflex action that forcibly expels an irritant.
The sense of smell
The nose is the organ of the sense of smell (olfaction). Specialised receptors that detect smell are located in the roof of the nose in the area of the cribriform plate of the ethmoid bones and the superior conchae (Figs 10.4 and 8.23A). These receptors are stimulated by airborne odours. The resultant nerve signals are carried by the olfactory nerves to the brain where the sensation of smell is perceived (p. 206).
Pharynx
Position
The pharynx (throat) is a passageway about 12–14 cm long. It extends from the posterior nares, and runs behind the mouth and the larynx to the level of the 6th thoracic vertebra, where it becomes the oesophagus.
Structures associated with the pharynx
Superiorly – the inferior surface of the base of the skull
Inferiorly – it is continuous with the oesophagus
Anteriorly – the wall is incomplete because of the openings into the nose, mouth and larynx
Posteriorly – areolar tissue, involuntary muscle and the bodies of the first six cervical vertebrae.
For descriptive purposes the pharynx is divided into three parts: nasopharynx, oropharynx and laryngopharynx.
The nasopharynx
The nasal part of the pharynx lies behind the nose above the level of the soft palate. On its lateral walls are the two openings of the auditory tubes (p. 193), one leading to each middle ear. On the posterior wall are the pharyngeal tonsils (adenoids), consisting of lymphoid tissue. They are most prominent in children up to approximately 7 years of age. Thereafter they gradually atrophy.
The oropharynx
The oral part of the pharynx lies behind the mouth, extending from below the level of the soft palate to the level of the upper part of the body of the 3rd cervical vertebra. The lateral walls of the pharynx blend with the soft palate to form two folds on each side. Between each pair of folds is a collection of lymphoid tissue called the palatine tonsil.
When swallowing, the soft palate and uvula are pushed upwards, sealing off the nasal cavity and preventing the entry of food and fluids.
The laryngopharynx
The laryngeal part of the pharynx extends from the oropharynx above and continues as the oesophagus below, with the larynx lying anteriorly.
Structure
The walls of the pharynx contain several types of tissue.
Mucous membrane lining
The mucosa varies slightly in the different regions. In the nasopharynx it is continuous with the lining of the nose and consists of ciliated columnar epithelium; in the oropharynx and laryngopharynx it is formed by tougher stratified squamous epithelium, which is continuous with the lining of the mouth and oesophagus. This lining protects underlying tissues from the abrasive action of foodstuffs passing through during swallowing.
Submucosa
The layer of tissue below the epithelium (the submucosa) is rich in mucosa-associated lymphoid tissue (MALT, p. 139), involved in protection against infection. Tonsils are masses of MALT that bulge through the epithelium. Some glandular tissue is also found here.
Smooth muscle
The pharyngeal muscles help to keep the pharynx permanently open so that breathing is not interfered with. Sometimes in sleep, and particularly if sedative drugs or alcohol have been taken, the tone of these muscles is reduced and the opening through the pharynx can become partially or totally obstructed. This contributes to snoring and periodic wakenings, which disturb sleep.
Constrictor muscles close the pharynx during swallowing, pushing food and fluid into the oesophagus.
Blood and nerve supply
Blood is supplied to the pharynx by several branches of the facial artery. The venous return is into the facial and internal jugular veins.
The nerve supply is from the pharyngeal plexus, and includes both parasympathetic and sympathetic nerves. Parasympathetic supply is by the vagus and glossopharyngeal nerves. Sympathetic supply is by nerves from the superior cervical ganglia (p. 174).
Functions
Passageway for air and food
The pharynx is involved in both the respiratory and the digestive systems: air passes through the nasal and oral sections, and food through the oral and laryngeal sections.
Warming and humidifying
By the same methods as in the nose, the air is further warmed and moistened as it passes towards the lungs.
Hearing
The auditory tube, extending from the nasopharynx to each middle ear, allows air to enter the middle ear. This leads to air in the middle ear being at the same pressure as the outer ear, protecting the tympanic membrane (eardrum, p. 193) from any changes in atmospheric pressure.
Protection
The lymphatic tissue of the pharyngeal and laryngeal tonsils produces antibodies in response to swallowed or inhaled antigens (Ch. 15). The tonsils are larger in children and tend to atrophy in adults.
Speech
The pharynx functions in speech; by acting as a resonating chamber for sound ascending from the larynx, it helps (together with the sinuses) to give the voice its individual characteristics.
Larynx
Position
The larynx or ‘voice box’ links the laryngopharynx and the trachea (Figs 10.1 and 10.4). It lies in front of the laryngopharynx and the 3rd, 4th, 5th and 6th cervical vertebrae. Until puberty there is little difference in the size of the larynx between the sexes. Thereafter, it grows larger in the male, which explains the prominence of the ‘Adam’s apple’ and the generally deeper voice.
Structure
Cartilages
The larynx is composed of several irregularly shaped cartilages attached to each other by ligaments and membranes. The main cartilages are:

Several ligaments attach the cartilages to each other and to the hyoid bone (Figs 10.5, 10.6 and 10.8).
The thyroid cartilage (Figs 10.5 and 10.6).
This is the most prominent of the laryngeal cartilages. Made of hyaline cartilage, it lies to the front of the neck. Its anterior wall projects into the soft tissues of the front of the throat, forming the laryngeal prominence or Adam’s apple, which is easily felt and often visible in adult males. The anterior wall is partially divided by the thyroid notch. The cartilage is incomplete posteriorly, and is bound with ligaments to the hyoid bone above and the cricoid cartilage below.
The upper part of the thyroid cartilage is lined with stratified squamous epithelium like the larynx, and the lower part with ciliated columnar epithelium like the trachea. There are many muscles attached to its outer surface.
The thyroid cartilage forms most of the anterior and lateral walls of the larynx.
The cricoid cartilage (Fig. 10.7).
This lies below the thyroid cartilage and is also composed of hyaline cartilage. It is shaped like a signet ring, completely encircling the larynx with the narrow part anteriorly and the broad part posteriorly. The broad posterior part articulates with the arytenoid cartilages and with the thyroid cartilage. It is lined with ciliated columnar epithelium and there are muscles and ligaments attached to its outer surface (Fig. 10.7). The lower border of the cricoid cartilage marks the end of the upper respiratory tract.
The arytenoid cartilages.
These are two roughly pyramid-shaped hyaline cartilages situated on top of the broad part of the cricoid cartilage forming part of the posterior wall of the larynx (Fig. 10.5). They give attachment to the vocal cords and to muscles and are lined with ciliated columnar epithelium.
The epiglottis (Figs 10.4–10.6 and 10.8).
This is a leaf-shaped fibroelastic cartilage attached on a flexible stalk of cartilage to the inner surface of the anterior wall of the thyroid cartilage immediately below the thyroid notch. It rises obliquely upwards behind the tongue and the body of the hyoid bone. It is covered with stratified squamous epithelium. If the larynx is likened to a box then the epiglottis acts as the lid; it closes off the larynx during swallowing, protecting the lungs from accidental inhalation of foreign objects.
Blood and nerve supply
Blood is supplied to the larynx by the superior and inferior laryngeal arteries and drained by the thyroid veins, which join the internal jugular vein.
The parasympathetic nerve supply is from the superior laryngeal and recurrent laryngeal nerves, which are branches of the vagus nerves. The sympathetic nerves are from the superior cervical ganglia, one on each side. These provide the motor nerve supply to the muscles of the larynx and sensory fibres to the lining membrane.
Interior of the larynx (Fig. 10.8)
The vocal cords are two pale folds of mucous membrane with cord-like free edges, stretched across the laryngeal opening. They extend from the inner wall of the thyroid prominence anteriorly to the arytenoid cartilages posteriorly.
When the muscles controlling the vocal cords are relaxed, the vocal cords open and the passageway for air coming up through the larynx is clear; the vocal cords are said to be abducted (open, Fig. 10.9A). Vibrating the vocal cords in this position produces low-pitched sounds. When the muscles controlling the vocal cords contract, the vocal cords are stretched out tightly across the larynx (Fig. 10.9B), and are said to be adducted (closed). When the vocal cords are stretched to this extent, and are vibrated by air passing through from the lungs, the sound produced is high pitched. The pitch of the voice is therefore determined by the tension applied to the vocal cords by the appropriate sets of muscles. When not in use, the vocal cords are adducted. The space between the vocal cords is called the glottis.
Functions
Speech.
This is produced when the sounds produced by the vocal cords are amplified and manipulated by the tongue, cheeks and lips.
Protection of the lower respiratory tract.
During swallowing (p. 297) the larynx moves upwards, blocking the opening into it from the pharynx. In addition, the hinged epiglottis closes over the larynx. This ensures that food passes into the oesophagus and not into the trachea.
Passageway for air.
The larynx links the pharynx above with the trachea below.
Humidifying, filtering and warming.
These processes continue as inspired air travels through the larynx.
Trachea
Position
The trachea or windpipe is a continuation of the larynx and extends downwards to about the level of the 5th thoracic vertebra where it divides at the carina into the right and left primary bronchi, one bronchus going to each lung. It is approximately 10–11 cm long and lies mainly in the median plane in front of the oesophagus (Fig. 10.10).
Structure
The tracheal wall is composed of three layers of tissue, and is held open by between 16 and 20 incomplete (C-shaped) rings of hyaline cartilage lying one above the other. The rings are incomplete posteriorly where the trachea lies against the oesophagus (Fig. 10.11). The cartilages are embedded in a sleeve of smooth muscle and connective tissue, which also forms the posterior wall where the rings are incomplete.
Three layers of tissue ‘clothe’ the cartilages of the trachea.
• The outer layer contains fibrous and elastic tissue and encloses the cartilages.
• The middle layer consists of cartilages and bands of smooth muscle that wind round the trachea in a helical arrangement. There is some areolar tissue, containing blood and lymph vessels and autonomic nerves. The free ends of the incomplete cartilages are connected by the trachealis muscle, which allows for adjustment of tracheal diameter.
• The lining is ciliated columnar epithelium, containing mucus-secreting goblet cells (Fig. 10.12).
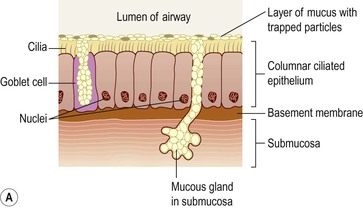

Figure 10.12 Cells lining the trachea. A. Ciliated mucous membrane. B. Coloured scanning electron micrograph of bronchial cilia.
Blood and nerve supply, lymph drainage
Arterial blood supply is mainly by the inferior thyroid and bronchial arteries and venous return is by the inferior thyroid veins into the brachiocephalic veins.
Parasympathetic nerve supply is by the recurrent laryngeal nerves and other branches of the vagi. Sympathetic supply is by nerves from the sympathetic ganglia. Parasympathetic stimulation constricts the trachea, and sympathetic stimulation dilates it.
Lymph from the respiratory passages drains through lymph nodes situated round the trachea and in the carina, the area where it divides into two bronchi.
Functions
Support and patency.
Tracheal cartilages hold the trachea permanently open (patent), but the soft tissue bands in between the cartilages allow flexibility so that the head and neck can move freely without obstructing or kinking the trachea. The absence of cartilage posteriorly permits the oesophagus to expand comfortably during swallowing. Contraction or relaxation of the trachealis muscle, which links the free ends of the C-shaped cartilages, helps to regulate the diameter of the trachea.
Mucociliary escalator.
This is the synchronous and regular beating of the cilia of the mucous membrane lining that wafts mucus with adherent particles upwards towards the larynx where it is either swallowed or coughed up (Fig. 10.12B).
Cough reflex.
Nerve endings in the larynx, trachea and bronchi are sensitive to irritation, which generates nerve impulses conducted by the vagus nerves to the respiratory centre in the brain stem (p. 160). The reflex motor response is deep inspiration followed by closure of the glottis, i.e. closure of the vocal cords. The abdominal and respiratory muscles then contract causing a sudden and rapid increase of pressure in the lungs. Then the glottis opens, expelling air through the mouth, taking mucus and/or foreign material with it.
Warming, humidifying and filtering.
These continue as in the nose, although air is normally saturated and at body temperature when it reaches the trachea.
Lungs
Position and gross structure (Fig. 10.13)
There are two lungs, one lying on each side of the midline in the thoracic cavity. They are cone-shaped and have an apex, a base, a tip, costal surface and medial surface.
The apex
This is rounded and rises into the root of the neck, about 25 mm above the level of the middle third of the clavicle. It lies close to the first rib and the blood vessels and nerves in the root of the neck.
The base
This is concave and semilunar in shape, and lies on the upper (thoracic) surface of the diaphragm.
The costal surface
This is the broad outer surface of the lung that lies directly against the costal cartilages, the ribs and the intercostal muscles.
The medial surface
The medial surface of each lung faces the other directly across the space between the lungs, the mediastinum. Each is concave and has a roughly triangular-shaped area, called the hilum, at the level of the 5th, 6th and 7th thoracic vertebrae. The primary bronchus, the pulmonary artery supplying the lung and the two pulmonary veins draining it, the bronchial artery and veins, and the lymphatic and nerve supply enter and leave the lung at the hilum (Fig. 10.14).
The mediastinum contains the heart, great vessels, trachea, right and left bronchi, oesophagus, lymph nodes, lymph vessels and nerves.
The right lung is divided into three distinct lobes: superior, middle and inferior. The left lung is smaller because the heart occupies space left of the midline. It is divided into only two lobes: superior and inferior. The divisions between the lobes are called fissures.
Pleura and pleural cavity
The pleura consists of a closed sac of serous membrane (one for each lung) which contains a small amount of serous fluid. The lung is pushed into this sac so that it forms two layers: one adheres to the lung and the other to the wall of the thoracic cavity (Figs 10.1 and 10.15).
The visceral pleura
This is adherent to the lung, covering each lobe and passing into the fissures that separate them.
The parietal pleura
This is adherent to the inside of the chest wall and the thoracic surface of the diaphragm. It is not attached to other structures in the mediastinum and is continuous with the visceral pleura round the edges of the hilum.
The pleural cavity
This is only a potential space and contains no air, so the pressure within is negative relative to atmospheric pressure. In health, the two layers of pleura are separated by a thin film of serous fluid (pleural fluid), which allows them to glide over each other, preventing friction between them during breathing. The pleural fluid is secreted by the epithelial cells of the membrane. The double membrane arrangement of the pleura is similar to the serous pericardium of the heart (p. 87).
The two layers of pleura, with pleural fluid between them, behave in the same way as two pieces of glass separated by a thin film of water. They glide over each other easily but can be pulled apart only with difficulty, because of the surface tension between the membranes and the fluid. This is essential for keeping the lung inflated against the inside of the chest wall. The airways and the alveoli of the lungs are embedded in elastic tissue, which constantly pull the lung tissues towards the hilum, but because pleural fluid holds the two pleura together, the lung remains expanded. If either layer of pleura is punctured, air is sucked into the pleural space and part or all of the entire underlying lung collapses.
Interior of the lungs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree