Chapter 3 The Abdomen
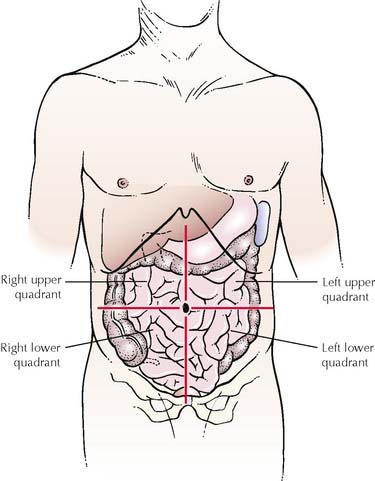
TABLE 3-1 Location of Organs in Abdominal Quadrants
| Right Upper Quadrant | Left Upper Quadrant |
|---|---|
| Right Lower Quadrant | Left Lower Quadrant |
|---|---|
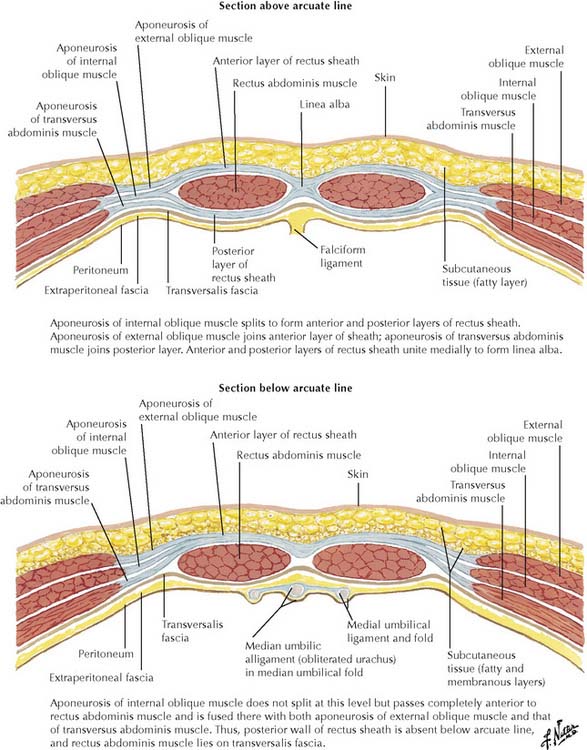
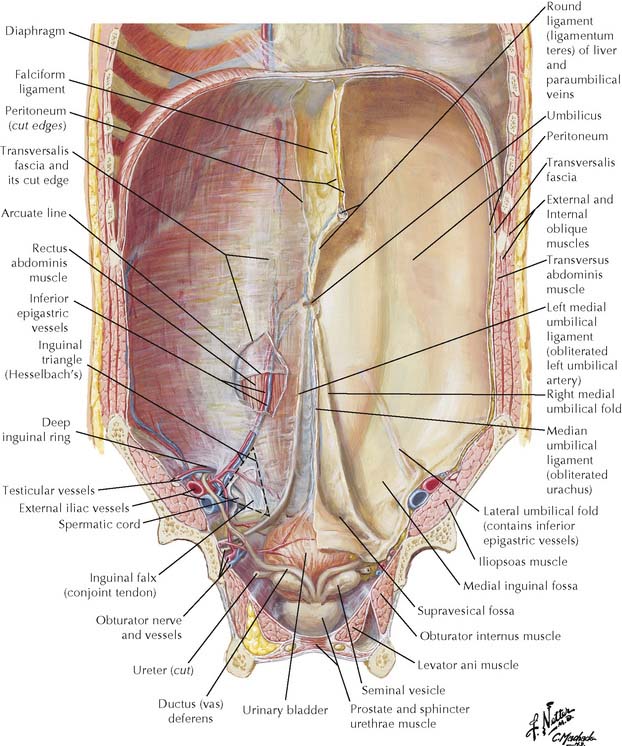
3-4 Formation of rectus sheath above (upper figure) and below (lower figure) arcuate line. The arcuate line (see Figure 3-7) is located midway between the umbilicus and pubic crest and marks the level below which all three aponeurotic layers pass anterior to the rectus abdominis muscle, which lies against transversalis fascia posteriorly. The arcuate line is also the point at which the inferior epigastric vessels enter the rectus sheath.
(From Netter, F H: Atlas of Human Anatomy, 4th ed. Philadelphia, Saunders, 2006, Plate 252.)
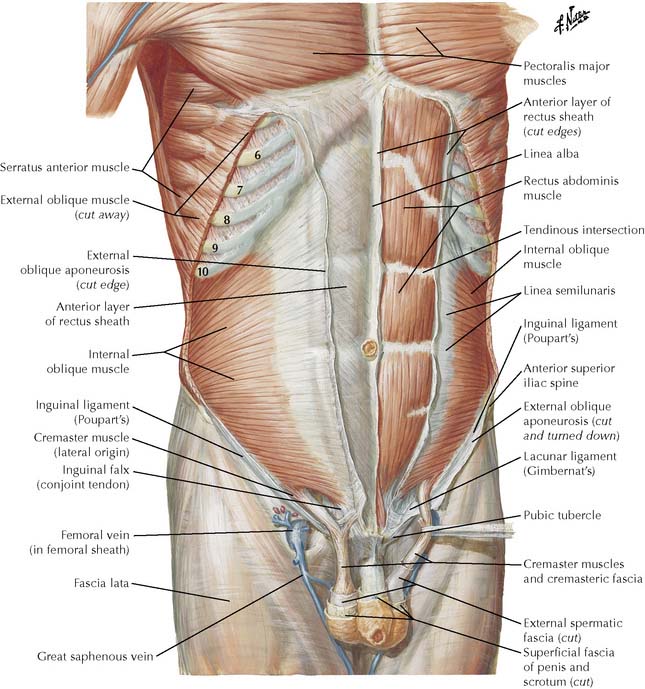
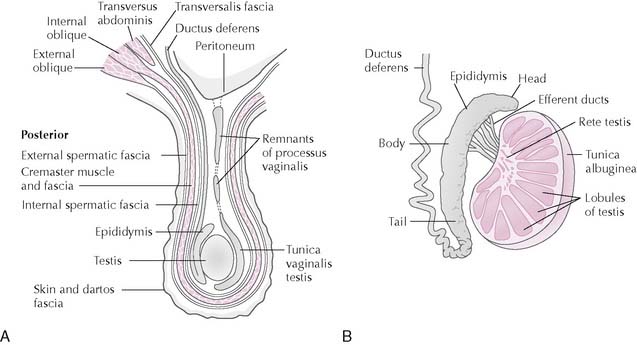
| Structure | Derived from | Comments |
|---|---|---|
| Superficial inguinal ring | Aponeurosis of external abdominal oblique | Lies above and lateral to pubic tubercle; transmits spermatic cord or round ligament |
| Deep inguinal ring | Oval defect in transversalis fascia | Lies lateral to inferior epigastric vessels and just above inguinal ligament |
| Inguinal ligament | Lower border of external oblique aponeurosis | Extends from anterior superior iliac spine to pubic tubercle. Curves inward, forming shallow trough that contains structures in inguinal canal |
| Lacunar ligament | Medial portion of inguinal ligament | Passes posteroinferiorly, forming medial border of femoral ring |
| Conjoint tendon | Aponeuroses of transversus abdominis and internal abdominal oblique muscles | Reinforces posterior wall of superficial inguinal ring |
| Pectineal ligament | Lacunar ligament | In inguinal hernia repair will hold sutures anchoring conjoint tendon |
| Iliopubic tract | Thickened inferior margin of transversalis fascia | Landmark on internal aspect of inguinal ligament on laparoscopic view |
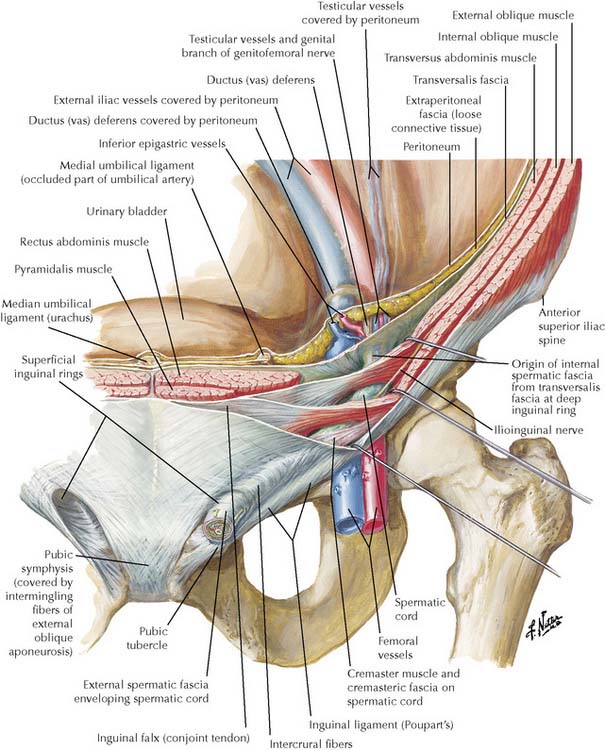
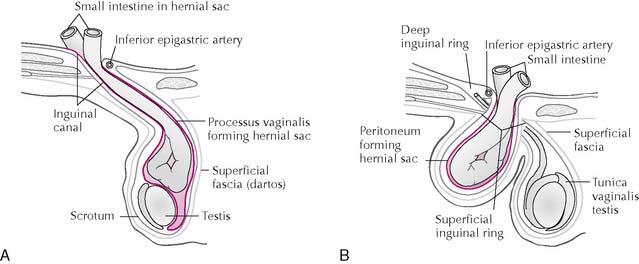
TABLE 3-3 Direct and Indirect Inguinal Hernias
| Characteristic | Indirect Inguinal Hernia | Direct Inguinal Hernia |
|---|---|---|
| Incidence | Most common type of hernia in both sexes but much more common in males, especially male children | 50% or less frequency of indirect inguinal hernias; more common in males over 40 |
| Predisposing Factors | Persistent processus vaginalis | Weak or narrow conjoint tendon, large superficial inguinal ring |
| Course through Abdominal Wall | Passes lateral to inferior epigastric vessels and through deep inguinal ring, inguinal canal, and superficial inguinal ring; often descends into scrotum or labium majus | Passes medial to inferior epigastric vessels through inguinal triangle and superficial inguinal ring; rarely descends into scrotum |
| Covering(s) of Herniating Structure | Same three covering layers as spermatic cord—external spermatic fascia, cremasteric layer, and internal spermatic fascia | External spermatic fascia after pushing through superficial inguinal ring |
| Complications | Prone to obstruction and strangulation of herniating intestine; surgical repair on diagnosis | More easily reduced than indirect hernias and less likely obstruction and strangulation |
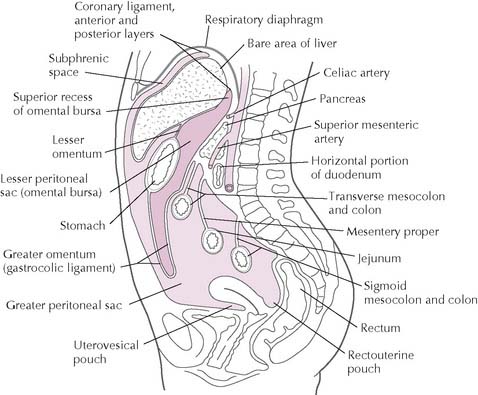
TABLE 3-4 Peritoneal Ligaments and Mesenteries
| Structure | Embryologic Origin | Comments |
|---|---|---|
| Greater omentum | Dorsal mesogastrium | Can prevent spread of infection by adhering to and localizing areas of inflammation |
| Gastrosplenic ligament | Contains short gastric arteries and veins | |
| Gastrocolic ligament | Contains gastro-omental (gastroepiploic) vessels | |
| Splenorenal ligament | Contains tail of pancreas and splenic vessels | |
| Lesser omentum | Septum transversum | Ventral mesentery of stomach and anterior wall of lesser peritoneal sac |
| Hepatogastric ligament | Contains right and left gastric vessels along lesser curvature | |
| Hepatoduodenal ligament | Contains common bile duct, proper hepatic artery, and portal vein | |
| Falciform ligament | Septum transversum | In its free edge contains ligamentum teres hepatis, remnant of left umbilical vein of fetus |
| Mesentery proper | Embryonic common dorsal mesentery | Contains vessels, nerves, and lymphatics supplying jejunum and ileum |
| Transverse mesocolon | Embryonic common dorsal mesentery | Contains middle colic vessels |
| Sigmoid mesocolon | Embryonic common dorsal mesentery | Contains sigmoidal arteries and veins |
| Mesoappendix | Embryonic common dorsal mesentery | Transmits appendicular artery and vein |
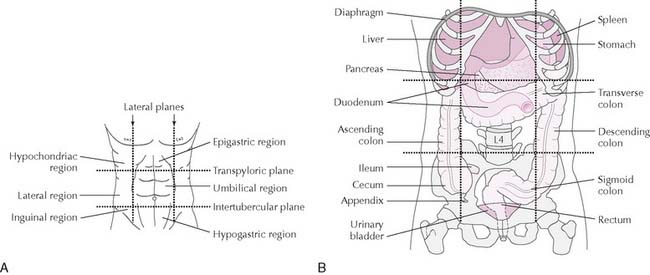
TABLE 3-5 Classification of Peritoneal Organs
| Intraperitoneal | Retroperitoneal | Secondarily Retroperitoneal |
|---|---|---|
| Duodenum, first part | Kidneys | Duodenum, second, third, and fourth parts |
| Liver and gallbladder | Ureters | Colon, ascending and descending |
| Pancreas, tail | Suprarenal glands | Rectum |
| Stomach | Abdominal aorta | Pancreas, head, neck, and body |
| Spleen | Inferior vena cava | |
| Jejunum | ||
| Ileum | ||
| Cecum | ||
| Appendix | ||
| Transverse colon | ||
| Sigmoid colon |
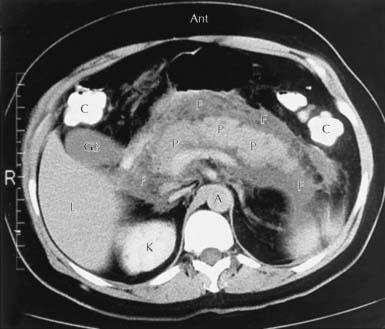
In acute pancreatitis fluid may accumulate within or around the pancreas as a pancreatic pseudocyst, and most often enters the omental bursa (Figure 3-11). Pseudocysts may become infected and may compress or erode adjacent structures. The majority of cases of acute pancreatitis are due to alcohol abuse or a gallstone obstructing the distal bile duct. Patients show constant severe epigastric pain radiating to the back with fever, nausea, and vomiting. Seventy percent of acute pancreatitis patients have elevated serum amylase (hyperamylasemia) for about 3 days. In necrotizing pancreatitis blood may dissect along fascial planes to produce ecchymoses in the flank (Grey-Turner sign) or periumbilical region (Cullen sign).
Pancreatic pseudocyst is a fluid collection in pancreatitis, most frequently in the omental bursa.
Flank or periumbilical ecchymoses may signal necrotizing pancreatitis.
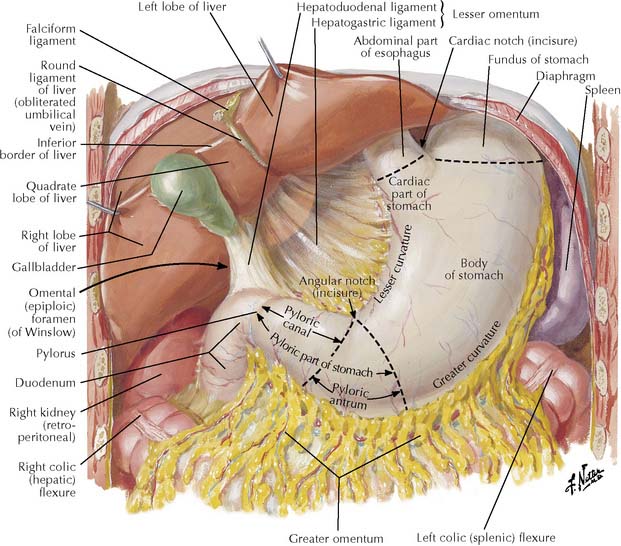
3-12 Stomach in situ with its parts labeled.
(From Netter, F H: Atlas of Human Anatomy, 4th ed. Philadelphia, Saunders, 2006, Plate 275.)
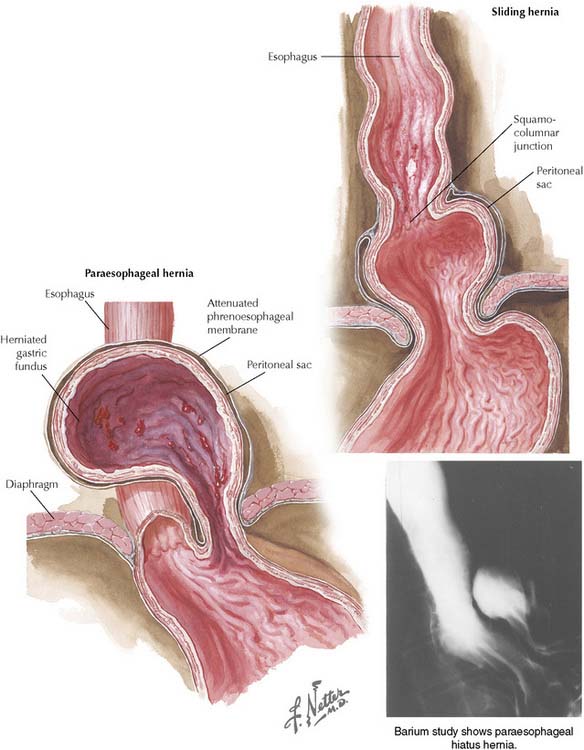
In a sliding hiatal hernia, the gastroesophageal junction herniates through the esophageal hiatus of the diaphragm with part of the stomach (Figure 3-14), predisposing to gastroesophageal reflux. Heartburn from hiatal hernia can mimic the substernal pain of myocardial infarction but differs in that the pain is usually lessened when the patient sits upright or takes antacids. In the less common paraesophageal hiatal hernia the gastroesophageal junction remains in place, but the adjacent fundus herniates into the thorax. A paraesophageal hernia usually does not cause reflux.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree