Lymphatic System
OVERVIEW OF THE LYMPHATIC SYSTEM
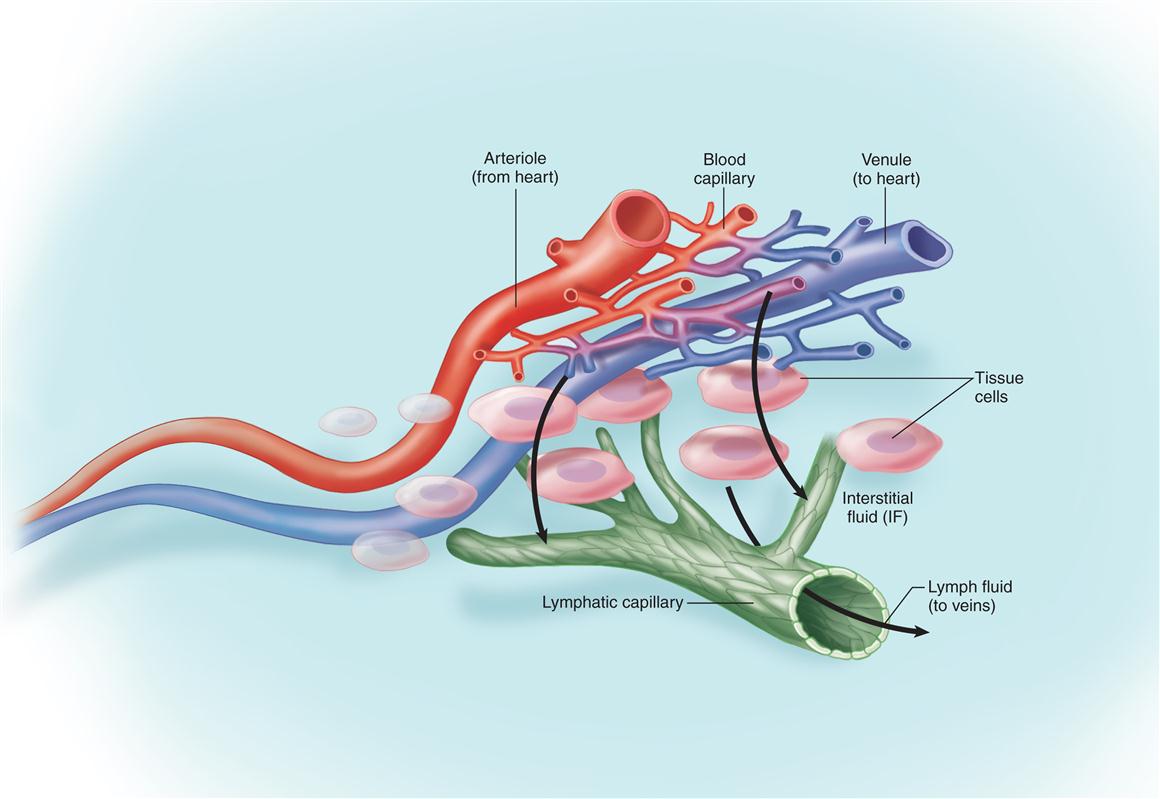
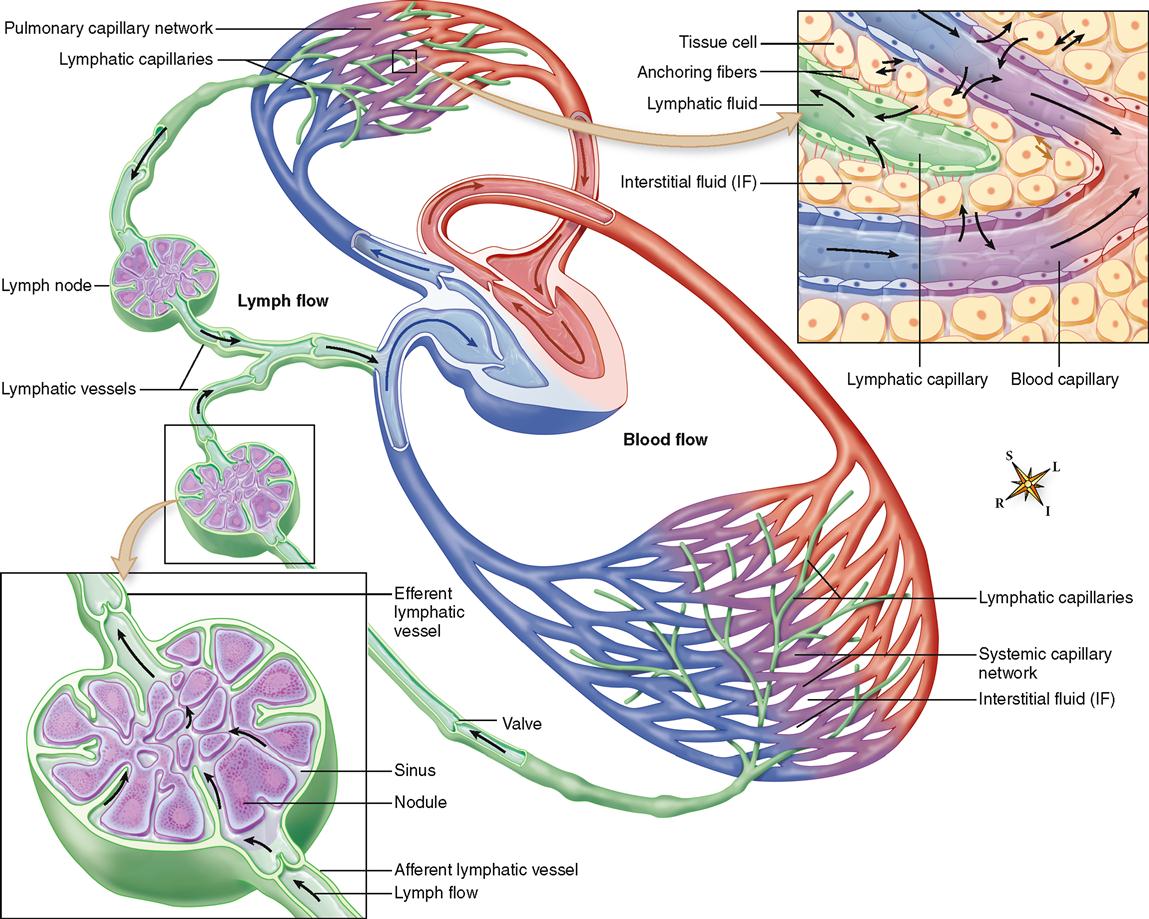
The importance of the lymphatic system in maintaining a balance of fluid in the internal environment is best explained by the diagram in Figure 23-1. As this figure shows, plasma filters into interstitial spaces from blood flowing through capillaries. Most of this interstitial fluid (IF) is absorbed by tissue cells or reabsorbed by the blood before it flows out of the tissue. However, a small percentage of the interstitial fluid remains behind (review Figure 22-26, A, on p. 703). If this continued for even a brief period, the increased interstitial fluid would cause massive edema (swelling) of the tissue. The high fluid pressure from this edema could cause tissue destruction or perhaps even death as normal functions became disrupted. Such a problem is avoided by the presence of lymphatic vessels that act as “drains” to collect the excess tissue fluid and return it to the venous blood just before it reaches the heart.
The lymphatic system is a component of the circulatory system because it consists of a moving fluid (lymph) derived from the blood and tissue fluid and a group of vessels (lymphatics) that return the lymph to the blood. In general, the lymphatic vessels that drain the peripheral areas of the body parallel the venous return.
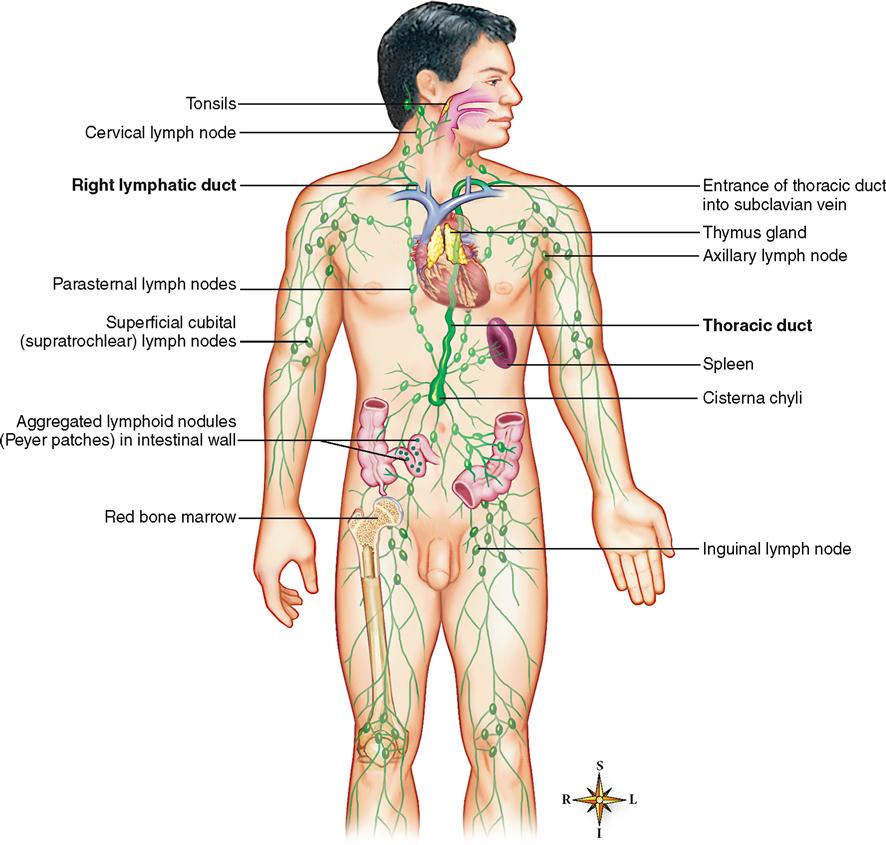
In addition to lymph and the lymphatic vessels, the system includes various structures that contain lymphoid tissue—a type of reticular tissue (see Chapter 6) that contains lymphocytes and other defensive cells. For example, lymph nodes are located along the paths of the collecting lymphatic vessels. Isolated nodules of lymphatic tissue, such as the aggregated lymphoid nodules called Peyer patches in the intestinal wall or the nodules of the vermiform appendix of the large intestine, are other examples. Additional lymphoid structures include the tonsils, thymus, spleen, and bone marrow (Figure 23-2).
Although it serves a unique transport function by returning tissue fluid, proteins, fats, and other substances to the general circulation, lymph flow differs from the true “circulation” of blood seen in the cardiovascular system. Unlike vessels in the blood vascular system, lymphatic vessels do not form a closed ring, or circuit, but instead begin blindly in the intercellular spaces of the soft tissues of the body (see Figure 23-1).
LYMPH AND INTERSTITIAL FLUID
Lymph (or lymphatic fluid) is the clear, watery-appearing fluid found in the lymphatic vessels. Interstitial fluid (IF), which fills the spaces between the cells, is not the simple fluid it seems to be. Studies show that it is an important and complex part of the ECM (extracellular matrix). Interstitial fluid and blood plasma together constitute the extracellular fluid compartment of the body, or in the words of Claude Bernard, the “internal environment of the body”—the fluid environment of cells in contrast to the atmosphere, or external environment, of the body.
Both lymph and interstitial fluid closely resemble blood plasma in composition. The main difference is that they contain a lower percentage of proteins than does plasma. Lymph is isotonic and almost identical in chemical composition to interstitial fluid when comparisons are made between the two fluids taken from the same area of the body. However, the average concentration of protein (4 grams/100 ml) in lymph taken from the thoracic duct (see Figure 23-2) is about twice that found in most interstitial fluid samples.
The elevated protein level of thoracic duct lymph (a mixture of lymph from all areas of the body) results from protein-rich lymph flowing into the duct from the liver and small intestine. A little more than one half of the 2800 to 3000 ml total daily lymph flowing through the thoracic duct is derived from these two organs.
Box 23-1 discusses the effects of abnormal loss of lymphatic fluid.
LYMPHATIC VESSELS
Distribution of Lymphatic Vessels
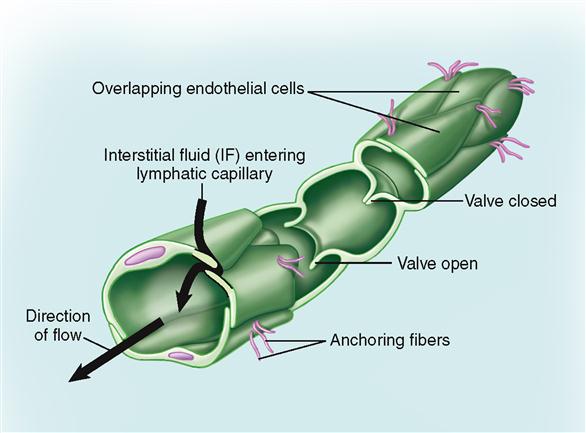
Lymphatic vessels—often simply called lymphatics—originate as microscopic blind-end vessels called lymphatic capillaries. (Those originating in the villi of the small intestine are called lacteals; see Chapter 29.) The wall of each lymphatic capillary consists of a single layer of flattened endothelial cells. Each blindly ending capillary is attached, or fixed, to surrounding cells by tiny connective tissue filaments. Networks of lymphatic capillaries branch and anastomose extensively. Lymphatic networks are located in the intercellular (interstitial) spaces and are widely distributed throughout the body. As a rule, lymphatic and blood capillary networks lie side by side but are always independent of each other.
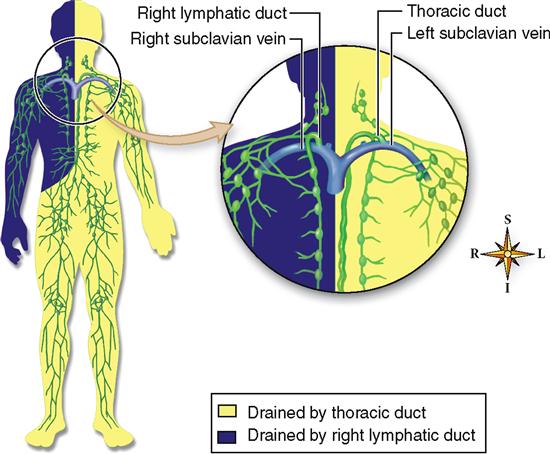
As twigs of a tree join to form branches, branches join to form larger branches, and larger branches join to form the tree trunk, so do lymphatic capillaries merge, forming slightly larger lymphatics that join other lymphatics to form still larger vessels, which merge to form the main lymphatic trunks: the right lymphatic duct and the thoracic duct (see Figure 23-2).
Lymph from the entire body, except for the upper right quadrant, drains eventually into the thoracic duct, which drains into the left subclavian vein at the point where it joins the left internal jugular vein (Figure 23-3). Lymph from the upper right quadrant of the body empties into the right lymphatic duct and then into the right subclavian vein. However, this structure can be vary among individuals. For example, in most people there are three separate lymphatic ducts that drain into the right subclavian vein rather than a single right lymphatic duct.
Because most of the lymph of the body returns to the bloodstream by way of the thoracic duct, this vessel is considerably larger than the other main lymph channels, the right lymphatic ducts, but is much smaller than the large veins, which it resembles in structure. It has an average diameter of about 5 mm (1.5 inches) and a length of about 40 cm (16 inches). It originates as a dilated structure, the cisterna chyli or chyle cistern, in the lumbar region of the abdominal cavity—where fatty lymph called chyle from the intestinal tract collects. The thoracic duct then ascends a curving pathway to the root of the neck, where it joins the subclavian vein as just described (see Figures 23-2 and 23-3).
Structure of Lymphatic Vessels
Lymphatics resemble veins in structure with these exceptions:
 Lymphatics have thinner walls.
Lymphatics have thinner walls.
 Lymphatics contain more valves.
Lymphatics contain more valves.
 Lymphatics contain lymph nodes located at certain intervals along their course.
Lymphatics contain lymph nodes located at certain intervals along their course.
The lymphatic capillary wall is formed by a single layer of large but very thin and flat endothelial cells (Figure 23-4). Although the openings (clefts) between endothelial cells of lymphatic capillary walls are small, they are larger than those found in blood capillaries—a fact that explains the remarkable permeability of this system.
As lymph flows from the thin-walled capillaries into vessels with a larger diameter (0.2 to 0.3 mm), the walls become thicker and exhibit the three coats, or layers, typical of arteries and veins (see Table 21-1, p. 646). Interlacing elastic fibers and several strata of circular smooth muscle bundles are found in both the tunica media and the tunica externa of the large lymphatic vessel wall. Boundaries between layers are less distinct in the thinner lymphatic vessel walls than in arteries or veins.
One-way valves are extremely numerous in lymphatics of all sizes and give the vessels a somewhat varicose and beaded appearance. Valves are present every few millimeters in large lymphatics and are even more numerous in the smaller vessels. Formed from folds of the tunica intima, each valve projects into the vessel lumen in a slightly expanded area circled by bundles of smooth muscle fibers.
Experimental evidence suggests that most lymph vessels have the capacity for repair or regeneration when damaged. Formation of new lymphatic vessels occurs by extension of solid cellular cores, or sprouts, formed by mitotic division of endothelial cells in existing vessels, which later become “canalized.”
Functions of Lymphatic Vessels
The lymphatics play a critical role in numerous interrelated homeostatic mechanisms. The high degree of permeability of the lymphatic capillary wall permits very large molecules and even particulate matter, which cannot be absorbed into a blood capillary, to be removed from the interstitial spaces. Proteins that accumulate in the tissue spaces can return to blood only by way of lymphatics. This fact has great clinical importance. For instance, if anything blocks lymphatic return, blood protein concentration and blood osmotic pressure soon fall below normal, and fluid imbalance and death will result (discussed in Chapter 32).
Lacteals (lymphatics in the villi of the small intestine) serve an important function in the absorption of fats and other nutrients. The milky lymph found in lacteals after digestion contains 1% to 2% fat and is called chyle. Interstitial fluid has a much lower lipid content than chyle (see Chapter 29).
CIRCULATION OF LYMPH
Water and solutes continually filter out of capillary blood into the interstitial fluid (see Figure 23-1). To balance this outflow, fluid continually reenters blood from the interstitial fluid. Newer evidence has disproved the old idea that healthy capillaries do not “leak” proteins. In truth, each day about 50% of the total blood proteins leak out of the capillaries into the tissue fluid and return to the blood by way of the lymphatic vessels. For more details about fluid exchange between blood and interstitial fluid, see Chapter 32. From lymphatic capillaries, lymph flows through progressively larger lymphatic vessels to eventually reenter blood at the junction of the internal jugular and subclavian veins (Figure 23-5).
The Lymphatic Pump
Although there is no muscular pumping organ connected with the lymphatic vessels to force lymph onward as the heart forces blood, lymph still moves slowly and steadily along in its vessels. Lymph flows through the thoracic duct and reenters the general circulation at the rate of about 3 liters per day. This occurs despite the fact that most of the flow is against gravity, or “uphill.” It moves through the system in the right direction because of the large number of valves that permit fluid flow only in the central direction.
What mechanisms establish the pressure gradient required by the basic law of fluid flow? Two of the same mechanisms that contribute to the blood pressure gradient in veins also establish a lymph pressure gradient. These are breathing movements and skeletal muscle contractions (see Figure 22-24, p. 702). Box 23-2 explains one of many reasons a working knowledge of lymphatic flow is important.
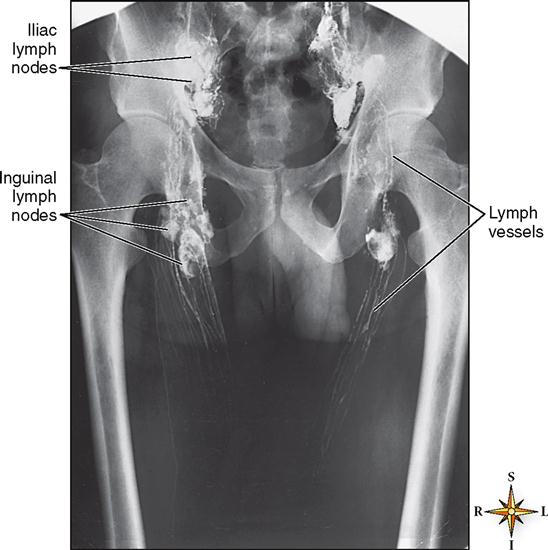
Activities that result in central movement, or flow, of lymph are called lymphokinetic actions (from the Greek kinetos, “movable”). Thus the flow of lymph may be called lymphokinesis. X-ray films taken after radiopaque material is injected into the lymphatics show that lymph pours into the central veins most rapidly at the peak of inspiration. This method of visualizing lymphatic vessels is called lymphangiography (Figure 23-6).