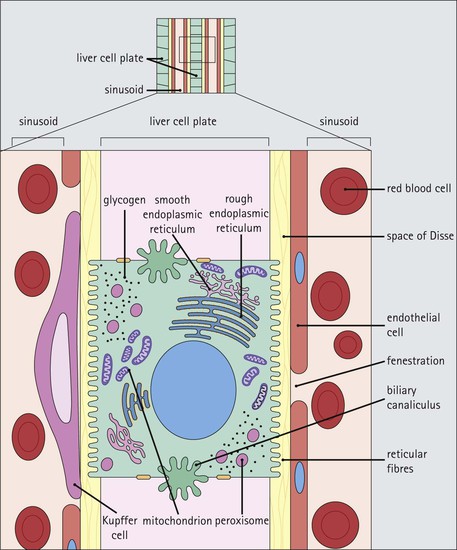
The liver acts as a vast biosynthetic chemical factory, synthesizing large complex molecules from substances brought to it in the blood, particularly substances recently absorbed by the intestine and transported by a portal blood system. The liver has a wide range of functions, which accounts for its complex structure All of the biochemical functions of the liver are carried out by the epithelial parenchymal cells of the liver, the hepatocytes, and are dependent on close interrelationships between: • The vasculature (hepatic artery and portal vein branches, sinusoids and central veins) • The bile drainage systems (the canaliculi and intrahepatic bile ducts, Fig. 12.1). Bile synthesis and secretion. The liver produces bile, which is an alkaline secretion containing water, ions, phospholipids, bile pigments (mainly bilirubin glucuronide) and bile acids (glycocholic and taurocholic). Excretion of bilirubin. Bilirubin is produced in the spleen from the breakdown of the haem component of haemoglobin. In the liver the bilirubin is conjugated with glucuronic acid, and the conjugate (bilirubin glucuronide) is excreted in the bile and thence the faeces. Protein metabolism. The liver is centrally involved in protein metabolism. It brings about deamination of amino acids; it produces urea from circulating ammonia; it also interconverts amino acids and produces the so-called non-essential amino acids. The liver synthesizes many proteins, including most of the plasma proteins such as albumin, blood clotting factors, such as fibrinogen, and prothrombin. The profile of proteins secreted by the liver can be influenced by cytokines circulating in the blood. In patients with inflammatory disorders, circulating cytokines can increase the concentration of several liver-produced proteins in the blood, such as fibrinogen, transferrin and serum-amyloid A protein. The production of some other proteins is downregulated, for example albumin. This is called an ‘acute-phase response’. Carbohydrate metabolism. Lipids and amino acids are converted into glucose in the liver by gluconeogenesis. The liver makes and stores glycogen, as well as forming intermediary compounds in carbohydrate metabolism. Lipid metabolism. The liver is involved in synthesis of cholesterol, lipoproteins and phospholipids. It synthesizes fat from other precursors. It also oxidizes fatty acids to provide energy. Storage. The liver acts as a store for vitamins A, D and B12. It stores iron as ferritin. Conjugation and elimination of metabolites and toxins. The smooth endoplasmic reticulum of the liver possesses large numbers of enzymes that break down or conjugate metabolites or toxic substances (e.g. alcohol, barbiturates, etc.). Certain hormones are eliminated by the liver. The liver receives blood from two vessels, the hepatic artery and the hepatic portal vein The liver receives blood from two sources: In the liver, the two input circulations (hepatic artery and hepatic portal vein) discharge their blood into a common network of anastomosing small vascular channels, the sinusoids (Fig. 12.2). The terminal parts of the hepatic portal and arterial systems run together in a connective tissue framework called portal tracts, which also contain bile ductules. After entering the liver at the porta hepatis, the portal vein divides within the liver into progressively smaller branches (interlobar, segmental and interlobular branches), which then branch further, eventually forming an extensive anastomosing network of terminal portal venules. Lateral side branches (inlet venules) of the terminal portal venules empty blood into the sinusoids, where it blends with blood from the terminal hepatic artery branches. The hepatic artery divides into successively smaller branches, the terminal elements running with the terminal branches of the hepatic portal vein before emptying into the hepatic sinusoids by short side branches (the arteriosinusoidal branches). A peribiliary plexus of small arterial branches supplies oxygenated blood into the large intrahepatic bile ducts before draining into the sinusoids, where it blends with blood from the portal venous system. The sinusoids are surrounded on all sides by hepatocytes. In this way, blood flowing through the liver is exposed to a massive surface area of liver cells. Hepatic sinusoids are the highly specialized liver capillary equivalents The hepatic sinusoids permeate the whole of the liver. They are lined by a thin, discontinuous, highly fenestrated endothelium, which is closely related externally to plates and cords of hepatocytes (Fig. 12.3), albeit separated from them by a space. This perisinusoidal space of Disse is the main site where material is transferred between the blood-filled sinusoids and hepatocytes. This transfer is in both directions, with some material being taken up by hepatocytes as well as being secreted. The hepatic sinusoids are partly lined by phagocytic cells (Kupffer cells), which are a form of macrophage and are derived from circulating blood monocytes. Blood leaving the sinusoids enters the central venules of the liver lobules Blood which has passed through the functioning liver parenchyma enters terminal hepatic venules (central veins of the lobules; discussed later on p. 231), which in turn unite to form intercalated veins; these then fuse to form larger hepatic vein branches. Hepatic veins are devoid of valves and open separately into the inferior vena cava as it passes through the liver on its way to the right atrium. Lymphatic fluid drains from the liver to the thoracic duct The liver produces a large volume of lymph. Fluid drains from the space of Disse into the portal tracts, in which it travels in fine channels. These lymphatic channels increase in size as the branches of the portal tracts merge towards the hepatic hilum. Finally, lymph drains into the thoracic duct. Such is the extent of lymph production by the liver that it comprises about half of the total lymph flow in the body under resting conditions. The main functional cell of the liver is the hepatocyte Hepatocytes (liver cells), which are intimately associated with the network of blood vessels (sinusoids), are polarized polyhedral cells with three identifiable types of surface (see below). As would be expected in cells that are so metabolically active, their cytoplasm is packed with a wide range of organelles. The nuclei are large, spherical and central, and contain scattered clumps of chromatin and prominent nucleoli. Many cells are binucleate, and nuclei are frequently polyploid; progressively more tetraploid nuclei develop with age. The Golgi is large and active, or small and multiple, and is mainly seen near the nucleus, with an extension lying close to the canalicular surface. The vesicles and tubules of the abundant smooth and rough endoplasmic reticulum are continuous with the Golgi. There are numerous free ribosomes in the cytosol, as well as large glycogen deposits and some lipid droplets, the glycogen often being closely related to the smooth endoplasmic reticulum. Lysosomes (see p. 24) of various sizes are numerous, some containing lipofuscin and lamellated lipoprotein. They are particularly large and numerous near the canalicular surface. Peroxisomes (see p. 25) usually number 200–300 per cell. Mitochondria are also abundant, numbering more than 1000 per cell, and are randomly scattered. This vast mitochondrial component gives the hepatocyte cytoplasm its eosinophilic granular appearance in H&E-stained paraffin sections. Hepatocytes have three important surfaces The hepatocyte surfaces are important because they are involved in the transfer of substances between hepatocyte, blood vessels and bile canaliculi. The three types of surface are sinusoidal, canalicular and intercellular (Figs 12.4, 12.5). Sinusoidal surfaces are separated from the sinusoidal vessel by the space of Disse Sinusoidal surfaces account for approximately 70% of the total hepatocyte surface. They are covered by short microvilli, which protrude into the space of Disse. Between the bases of the microvilli are coated pits (see Fig. 2.5), which are involved in endocytosis.
Liver
Introduction
Liver Vasculature



Hepatocytes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Liver
Chapter 12
FIGURE 12.3 Hepatic sinusoids. (a) High-power micrograph showing the relationship between the sinusoidal channels (S) and the cuboidal hepatocytes (H). Note the terminal hepatic venule, V. (b) Micrograph of liver stained to demonstrate reticulin fibres (black), which run in the space of Disse between the hepatocyte surface and the endothelial cells lining the sinusoid (see also Fig. 12.5c,d). This method delineates the outline of the sinusoid (S) and the hepatocyte columns (H) and is used in the histological diagnosis of liver disease on small cores of liver tissue obtained by needle biopsy (see also Fig. 1.1). (c) Immunoperoxidase preparation (showing lysozyme) identifying scattered phagocytic Kupffer cells (K) in the sinusoid lining.