Jacqueline R. Bak
Wound Healing, Dressings, and Drains
The ability to heal wounds is one of the most powerful defensive properties humans possess. Wound healing is a complex, highly organized response by an organism to tissue disruption caused by injury. This process is highly reliable in the absence of endogenous and exogenous infection, mechanical interference, or certain disease processes. Apposition and maintenance of the edges of a cleanly incised wound almost always result in prompt healing. A primary goal of perioperative patient care is the prevention of surgical site (wound) infections. Surgical site infections (SSIs) are a significant cause of illness, death, and excessive healthcare costs. Surgical wounds have the potential for infection from strains of antibiotic-resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) (Research Highlight).
Postoperative SSIs are a major complication for approximately 30 million individuals undergoing surgery annually in the United States, with an estimated 20% acquiring a healthcare-associated infection (HAI). SSIs are the third most commonly reported HAI, resulting in a complication rate of 1% to 12% of all surgical procedures, with an estimated cost of $12,000 to $30,000 per infection (Peterson, 2009). Although many surgeries are performed on an ambulatory basis and the average number of admissions to hospitals and length of stay have decreased since the 1980s, the incidence of HAIs has increased (Ambulatory Surgery Considerations). In response to the Deficit Reduction Act of 2005, the Centers for Medicare & Medicaid Services (CMS) have modified payment for selected reasonably preventable complicating conditions that have evidence-based prevention guidelines. Examples of these conditions are catheter-related infections and infections associated with coronary artery bypass grafts, certain orthopedic procedures, and certain bariatric surgery procedures (CMS, 2012). Actions taken by perioperative personnel sometimes can mean the difference between developing an SSI and normal healing. A clear understanding of these actions along with a solid knowledge of wound healing and factors adversely affecting healing are essential to the appropriate management of patients undergoing surgery. It is also imperative in light of the evolving CMS-implemented reduction in payment for an expanding array of avoidable conditions that include wound-related infections.
Anatomy
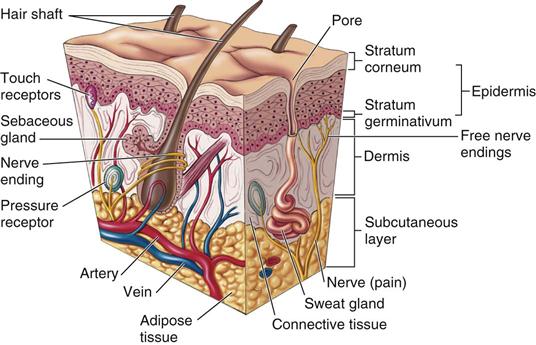
The skin is the largest organ of the body and acts as the first line of defense against infection. It provides protection and sensation, regulates fluid balance and temperature, and produces vitamins (e.g., vitamin D) and immune system components. The skin of the average adult covers about 3000 square inches, weighs about 6 pounds, and receives one third of the body’s circulating blood volume. It varies in thickness from 0.5 mm in the tympanic membrane to 6 mm on the soles of the feet and the palms of the hands. Key structures of the skin are the primary layers of the epidermis, the dermis, and the subcutaneous. The epidermis is the outermost layer of the skin, lines the ear canals, and is contiguous with the mucous membranes. The epidermis is composed of several layers consisting of keratin and lipids. Keratin is the primary substance that hardens nails and hair and protects the body from fluid loss and invasion by pathogens. The epidermis is supported by the dermis, which is thicker than the epidermis and composed of collagen. The dermis is the largest portion of the skin, providing strength and structure. Contained within the dermis are blood vessels, lymph ducts, hair roots, nerves, and sebaceous and sweat glands. The dermis is vascularized and innervated (Figure 9-1). The innermost subcutaneous layer is composed of adipose tissue that merges with the deepest layer of the dermis to provide insulation, shape, and support. Any wound or disruption of the skin can provide a portal for bacteria and possible infection.
Etiology of Wounds
The causes of wounds can be described as follows:
• Surgical—caused by an incision or excision
• Traumatic—caused by mechanical, thermal, or chemical destruction
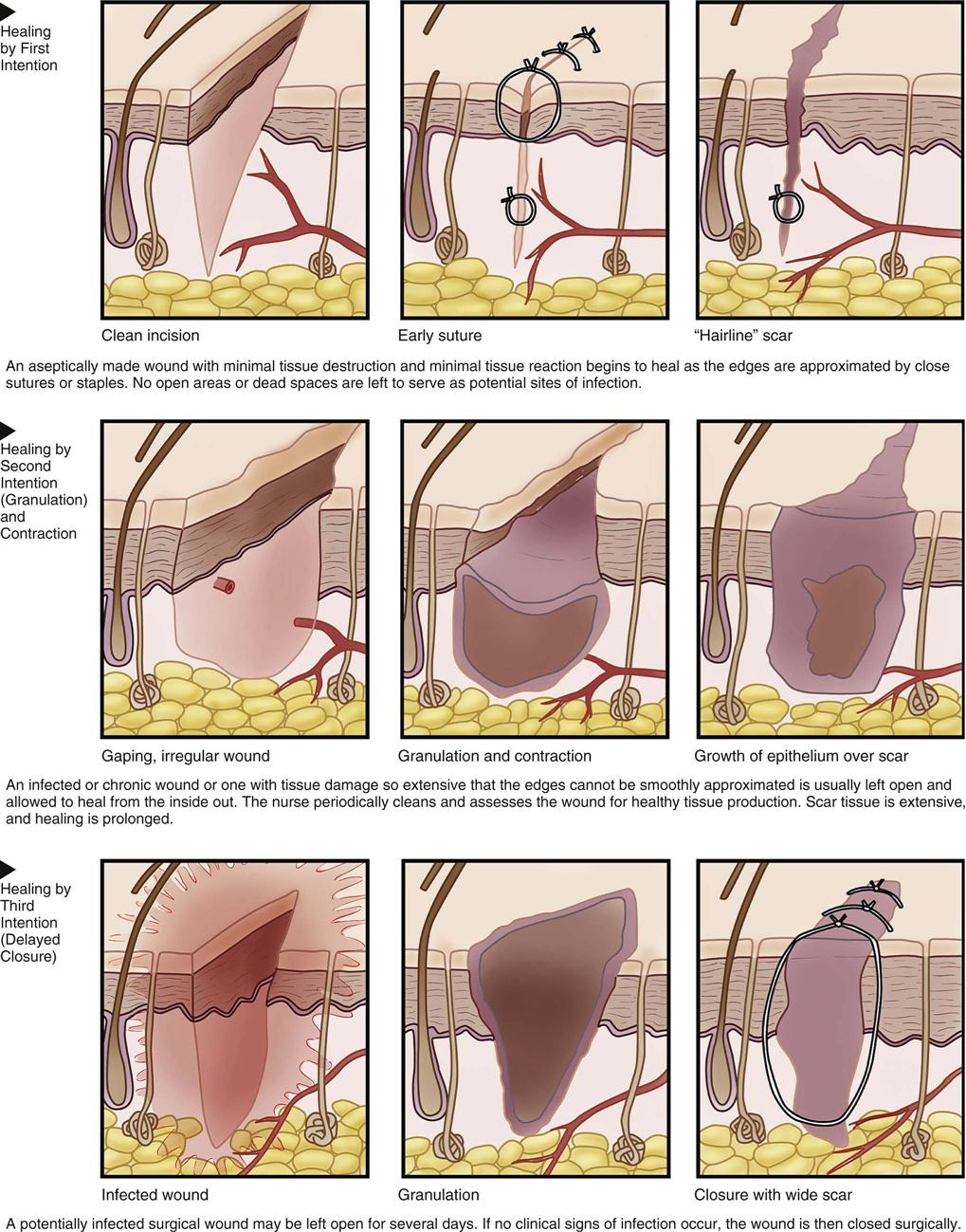
The amount of tissue loss, the existence of contamination or infection, and the degree of damage to tissue are some factors that determine the type of wound closure selected by the surgeon. The healing process is inherently related to whether the wound is closed or left open. This process occurs in one of three ways: primary intention, second intention (granulation and contraction), and third intention (delayed closure) (Figure 9-2).
Types of Wound Closure
Primary Intention
Healing through primary intention occurs when wounds are created aseptically, with a minimum of tissue destruction and postoperative tissue reaction. Wounds closed with sutures, staples, tape, or surgical adhesive applied as soon after the time of injury as possible fall into this category. When wounds are created under sterile conditions, healing is optimized and begins almost immediately. This type of healing is known as primary intention and occurs under the following conditions:
Second Intention (Granulation and Contraction)
When surgical wounds are characterized by tissue loss with an inability to approximate wound edges, healing occurs through second intention (see Figure 9-2). This type of wound is usually not closed; instead, it is allowed to heal from the inside toward the outer surface. In infected wounds this process allows the proper cleansing and dressing of the wound as healthy collagen tissue expands from the inside. The area of tissue loss gradually fills with granulation tissue, comprising fibroblasts and capillaries. Scar tissue is extensive because of the size of the tissue gap that must be closed. The scar is referred to as a cicatrix. Contraction of surrounding tissue also occurs. Consequently this healing process takes longer than primary intention healing. Healing by second intention is often seen in chronic wounds, dirty wounds, and traumatic wounds in which large areas of tissue are lost.
Delayed Primary Closure or Third Intention
As the name delayed primary closure implies, this healing process occurs when approximation of wound edges is intentionally delayed by 3 or more days after injury or surgery (see Figure 9-2). These wounds may require debridement and usually require a primary and secondary suture line, such as when retention sutures are used. The conditions leading to a decision to delay closure are as follows:
Phases of Wound Healing
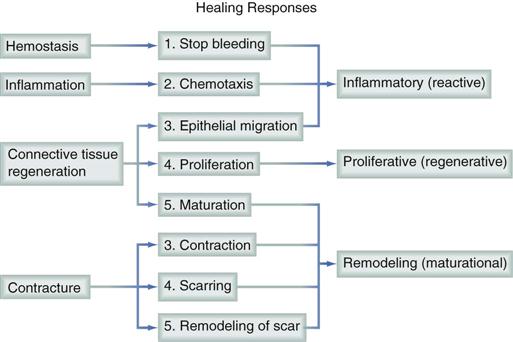
Wound healing is the effort of the injured tissue to return to normal integrity after injury. It is an intricate biologic process that occurs in three simultaneous yet overlapping phases: (1) inflammatory (also known as the reactive stage), (2) proliferative (also known as the regenerative stage), and (3) remodeling (also known as the maturational stage) (Leong and Phillips, 2012) (Figure 9-3).
Inflammatory Phase
In the inflammatory phase, an exudate containing blood, lymph, and fibrin begins to clot and loosely binds the cut edges together. Blood supply to the area increases, and the basic process of inflammation begins. Inflammation is a prerequisite to wound healing and is a vascular and cellular response to dispose of bacteria, foreign material, and dead tissue. Leukocytes increase in number to fight bacteria in the wound area and by phagocytosis help to remove damaged tissues. The severed tissue is quickly glued together by strands of fibrin and a thin layer of clotted blood, forming a scab. Plasma seeps to the surface to form a dry, protective crust. This seal helps to prevent fluid loss and bacterial invasion. During the first few days of wound healing, however, the seal has little tensile strength. The inflammatory phase normally lasts 1 to 4 days. The skin edges may appear mildly swollen and slightly red in this phase as a result of the inflammatory processes at work. Many chronic wounds “stall” at this phase.
Proliferative Phase
The proliferative phase, beginning within hours of the injury, allows new epithelium to cover the wound. Epithelial cells migrate and proliferate to the wound area, covering the surface of the wound to close the epithelial defect. Epithelialization also provides a protective barrier to prevent fluid and electrolyte loss and to reduce the incidence of infection. While reepithelialization takes place collagen synthesis and wound contraction are occurring. Contraction begins approximately 5 days after the wound onset and peaks at 2 weeks, gradually shrinking the entire wound. Granulation tissue forms under the edges of the incision and can be palpated as a hard ridge, which eventually resolves during the remodeling phase. Epidermal migration is limited to about 3 cm from the point of origin. Larger wounds may require skin grafting because of this limited epidermal migration. Collagen synthesis produces fiber molecules that crosslink to provide strength to the wound.
Remodeling Phase
Remodeling begins after approximately 2 to 4 weeks, depending on the size and nature of the wound. It may last 1 year or longer. During the remodeling phase, scar tissue formed during fibroplasia changes in bulk, form, and strength. Throughout normal wound healing, new collagen is produced while old collagen breaks down in a balanced fashion. This collagen turnover allows randomly deposited connective tissue to be arranged in linear and lateral orientation. As the scar ages, fibers and fiber bundles become more closely packed and form a crisscross pattern, ultimately creating the final shape of the wound. At best, the tensile strength of scar tissue is never more than about 80% of the tensile strength of nonwounded tissue.
Factors Affecting Wound Healing
Patients should be assessed for factors that may impair wound healing. Important factors in tissue repair and healing to consider are the patient’s age, physical status, preexisting conditions, nutritional status, oxygenation level, and overall recuperative power. The inflammatory response and oxygen tension depend on microcirculation to deliver components to the wound. Decreased oxygen tension to the wound area inhibits fibroblast migration and collagen synthesis, resulting in decreased tensile strength of the wound. Nutritional status also has a profound effect on healing because of the need for an adequate supply of protein necessary for the growth of new tissues. Protein also is required for the regulation of the osmotic pressure of blood and other body fluids and the formation of prothrombin, enzymes, hormones, and antibodies. Other nutritional essentials are water; vitamins A, C, B6, and B12; iron; calcium; zinc; and adequate calories. It is also important to maintain body temperature (normothermia) (Schwulst and Mazuski, 2012).
The most common cause of delayed wound healing in a surgical patient is SSI. Box 9-1 lists types of SSIs and defines criteria for classification. There are many possible causes of SSIs, including patient susceptibility to and severity of illness, microbial contamination by the patient’s microflora, and exogenous wound contamination from the operating room (OR) environment and personnel. Adherence to strict aseptic principles, careful observation of sterile technique, and thorough antimicrobial preparation of the patient and operative site are essential to minimize the risk of postoperative SSI. Perioperative personnel who are not scrubbed at the sterile field must maintain meticulous hand hygiene during the procedure to decrease the transmission of bacteria to the surgical field or the patient (Patient Safety).
Wound healing also can be impaired by poor surgical technique. Rough handling of tissue may cause trauma that can lead to bleeding and other conditions conducive to infection. Examples of surgical technique promoting wound healing include adequate hemostasis, precise cutting and suturing techniques, efficient use of time to minimize wound exposure to air, elimination of dead spaces, and minimal pressure from retractors and other instruments.
Additional factors affecting wound healing are the patient’s age, stress level, immunologic status, and smoking history. Preexisting conditions, such as diabetes, anemia, malnutrition, cancer, obesity, certain drug therapies (e.g., steroid therapy), and cardiovascular or respiratory impairments, also contribute to poor wound healing. Additional terms used in connection with wound healing are shown in Box 9-2.