Otorhinolaryngologic Surgery
Troy J. DeRose
Otorhinolaryngology is the study and science of the human ear (oto), nose (rhino), and throat (laryngo). It is a specialty that continues to evolve as a result of cutting-edge technology; high-powered surgical microscopes; narrower, flexible endoscopes; computer imaging; wound care improvements; and navigation systems that communicate with radiologic imaging. Such advances yield significant gains in improving the health and surgical outcomes of patients with physical ailments of the head and neck. This chapter comprehensively and respectively reviews perioperative care of patients undergoing surgical procedures to the ear, nose, head, and neck.
Surgical Anatomy
External, Middle, and Inner Ear
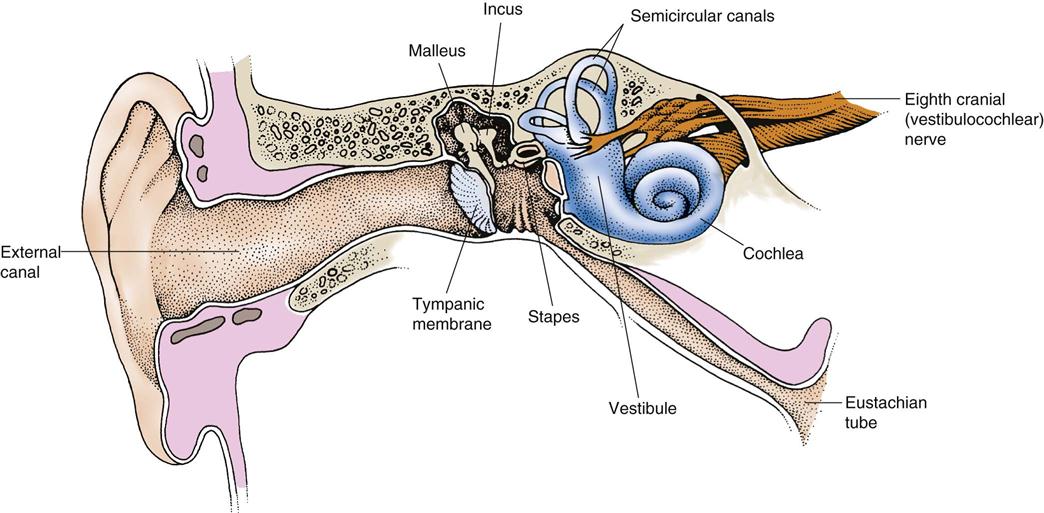
The ear is a sensory organ that identifies, localizes, and interprets sound as well as maintains equilibrium. Hearing is the sense by which sounds are appreciated. Referred to as the “watchdog of the senses,” hearing is the last sense to disappear when one falls asleep and the first to return when one awakens. The physical nature of sound results from the compression and rarefaction of pressure waves and moving molecules, but the sensations humans actually experience are the product of complex mechanical, electrical, and psychologic interactions in the ear and central nervous system. Three anatomic segments—the external ear, middle ear, and inner ear—work together to provide hearing and balance (Figure 19-1).
The external ear includes the auricle (or pinna) and external auditory canal, and is composed of cartilage covered with skin. The auricles are fixed in position and lie close to the head; they concentrate incoming sound waves and conduct them into the external auditory canal. Both ears provide stereophonic hearing that gives us very specific sound localization capabilities. Without binaural hearing, determining where sounds emanate can be difficult; this is a common problem for patients with unilateral or asymmetric hearing loss.
The external auditory canal, an S-shaped pathway leading to the middle ear, is approximately 2.5 cm in length in adults and shelters the tympanic membrane. Its skeleton of bone and cartilage is covered with very thin, sensitive skin. The canal lining is protected and lubricated with cerumen, a waxy substance secreted by sebaceous glands in the distal third of the canal. Cerumen helps to trap foreign material and has a mildly acidic pH that reduces bacterial levels in the outer ear.
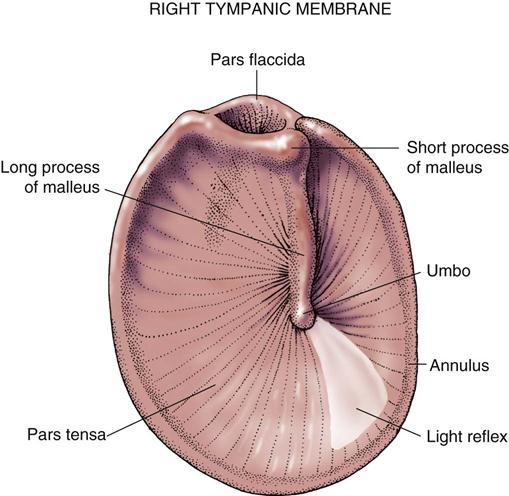
Located at the end of the external auditory canal is the tympanic membrane (eardrum) (Figure 19-2). It is a thin structure with three distinct layers: an outer squamous epithelial layer in continuity with the skin of the external ear canal, a fibrous middle layer for strength and support, and a medial mucous membrane layer that is continuous with the lining of the middle ear.
The middle ear is filled with air, which flows from the nasopharynx through the eustachian tube. It is divided into three areas: the epitympanum (upper), mesotympanum (middle), and hypotympanum (lower). Posteriorly, the epitympanic portion of the middle ear communicates with the mastoid air cells of the temporal bone via the mastoid antrum. The mucous membrane of the middle ear is continuous with that of the pharynx and the mastoid cells, making it possible for infection to travel to the middle ear (otitis media) and mastoid cells (mastoiditis). The eustachian tube serves to aerate the air-filled spaces of the temporal bone and to equalize pressure in the middle ear with atmospheric pressure. It is normally closed at rest and actively opens during yawning, sneezing, or swallowing. A chain of three small articulated bones (ossicles) extends across the middle ear cavity and conducts vibrations (airborne sound waves) from the tympanic membrane across the middle ear into the oval window and the fluid-filled inner ear (Figure 19-3).
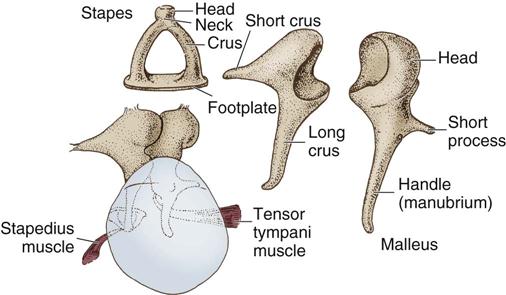
The malleus (hammer) consists of a head, neck, handle, and short process. The handle and short process are attached to the undersurface of the eardrum, and the head articulates with the body of the incus in the upper segment of the middle ear called the epitympanum or “attic.” The incus (anvil) consists of a body and long and short processes (see Figure 19-2). The distal end of the long process of the incus is called the lenticular process and articulates with the capitulum (head) of the stapes, which is the third, innermost bone. The stapes (stirrup) consists of a head, neck, anterior and posterior crura, and a mobile footplate that is secured to the oval window by an annular ligament. The movable joints between these ossicles contribute to a lever system that amplifies the received sound and transmits and converts vibrations from ambient air to the fluid of the inner ear.
The inner ear is protected from loud noise by the tensor tympani muscle, which draws the drum inward to increase tension and restricts its ability to vibrate, and the stapedius muscle, which contracts and tightens the stapes in the oval window to reduce the intensity of vibrations passing through the ossicles into the inner ear. The middle ear and mastoid are supplied with blood from the branches of the internal and external carotid artery systems.
The inner ear is a membranous, curved cavity located in the petrous portion of the temporal bone; it contains hair cell receptors that provide us with both hearing and balance. The inner ear consists of a bony labyrinth filled with a watery fluid (perilymph) that surrounds and bathes a membranous labyrinth filled with another fluid with distinct electrolyte characteristics, called the endolymph. The bony labyrinth includes the cochlea and the vestibular labyrinth.
The cochlea resembles a snail shell. It is divided into three compartments: the scala vestibuli, which is associated with the oval window; the scala tympani, which is associated with the round window; and the cochlear duct. The scala vestibuli and scala tympani are filled with perilymph, whereas the cochlear duct contains endolymph. On the basilar membrane of the cochlea lies the organ of Corti—the neural end organ for hearing. Its neuroepithelium projects thousands of hair cells that are set into motion by vibrations passing through the ossicles and oval window to the perilymph. The hair cells convert the mechanical energy of wave movement from vibration in the perilymph into electrochemical impulses. The vestibular labyrinth is composed of the utricle, the saccule, and three semicircular canals, referred to as the lateral, superior, and posterior canals. They are positioned at right angles to one another and are responsible for detecting angular acceleration that can be elicited with any head or body movement. Each canal contains a sense organ (crista) that responds to fluid movement in the endolymph, which triggers impulses in the vestibular branch of the acoustic nerve. Cristae are stimulated by angular accelerations and movements, such as head turning. The maculae of the utricle and saccule of the vestibular labyrinth are gravity oriented. Linear accelerations are detected by the utricle and saccule; they both have a mat of sensory cells (otoconia) imbedded in a gelatinous material covered with calcium deposits. The weight of these otoconia constantly orients us to the direction of gravity. Their inertia gives information about linear accelerations. The combined signals from the cristae of the semicircular canals and the sensory cells of the utricle and saccule provide a sense of balance and orientation in space. The internal auditory branches of the basilar artery supply the inner ear.
Nasal Anatomy
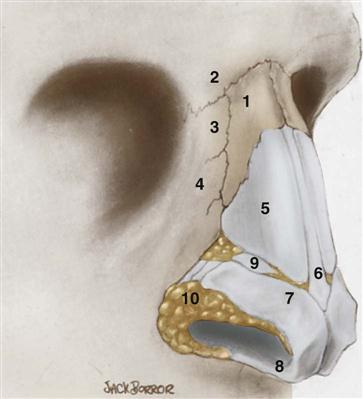
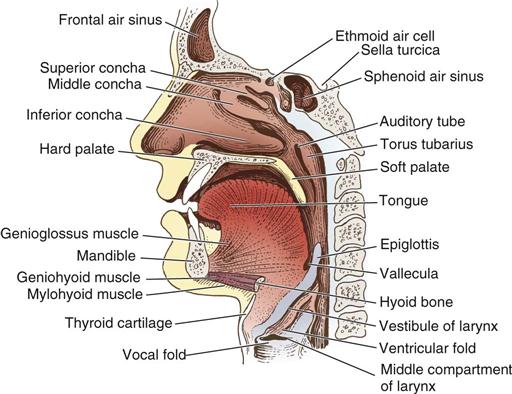
The nose is covered with skin and is supported internally by bone and cartilage. The two external nares provide openings for the passage of air through the nasal cavity. These openings contain internal hairs for the filtration of coarse particles that are sometimes carried by air. The nose is divided into the prominent external portion and the internal portion known as the nasal cavity (Figure 19-4). The chief purpose of the nose is to prepare air for use in the lungs.
The nasal bones and the frontal process of the maxilla form the upper portion of the external nose, and the lower portion is formed by a group of nasal cartilages and connective tissue covered with skin (Figure 19-5). The nostrils and the tip of the nose are shaped by the major alar cartilages. The nares are separated by the columella, which is formed by the lower margin of the septal cartilage, the medial parts of the major alar cartilages, and the anterior nasal spine, all of which are covered with skin. The nasal cavity is divided medially into right and left portions by the nasal septum.
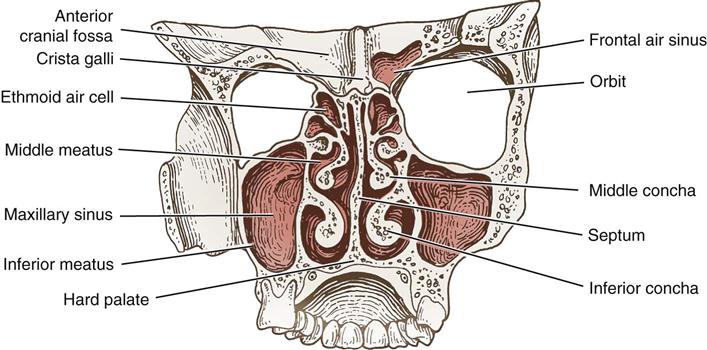
The nasal septum is composed of three structures: the nasal cartilage, the perpendicular plate of the ethmoid bone, and the vomer bone. The septum is covered by mucoperichondrium on either side that contains blood vessels and mucus-secreting cells. The rich blood supply warms and moistens the air, and the sticky mucus traps dust, pollen, and other small particles.
The nasal cavity communicates with the outside by its external openings, called the nares. The nares open into the nasopharynx through the choanae. The nasal cavity is also associated with each ear, sharing the torus tubarius (opening of the eustachian tube in the nasopharynx) with the paranasal sinuses (frontal, maxillary, ethmoidal, sphenoidal) through their respective orifices (meatus). The nasal cavity also communicates with the conjunctivae through the nasolacrimal duct. The nasal cavity is separated from the lingual cavity by the hard palate and soft palate (see Figure 19-4) and from the cranial cavity by the ethmoids. It is held together by periosteal covering over bone and by perichondrium, which extends over the cartilages. The turbinate bones of the nasal structure are arranged one above the other, separated by grooves that are composed of pseudostratified columnar ciliated respiratory epithelium. The turbinates act to increase the turbulence of airflow to humidify and regulate the temperature of air that is naturally inspired. This area is commonly referred to as the sphenoethmoidal recess and contains bony shelves known as the the superior, middle, and inferior meatus or turbinates (Figure 19-6).
The nasal sinuses serve as air spaces and communicate with the nasal cavity through the meatus. Anteriorly, on each side of the skull, the frontal sinus, the anterior ethmoidal sinus, and the maxillary sinus (antrum of Highmore) drain into the middle meatus; the posterior ethmoid and the sphenoid sinuses drain into the sphenoethmoidal recess (see Figure 19-6).
Throat Anatomy
Oral Cavity
The oral cavity is composed of the mouth and salivary glands. The mouth is formed by the cheeks, the hard palate, the mandible, and the tongue. It extends from the lips to the junction of the hard and soft palates. The portion of the mouth outside the teeth is the buccal cavity, and that on the inner side of the teeth is the lingual cavity. The hard palate forms the upper boundary of the oral cavity. The hard palate is formed by the maxilla and palatine bones. The mandible and floor of the mouth form the lower boundary of the oral cavity (Figure 19-7).
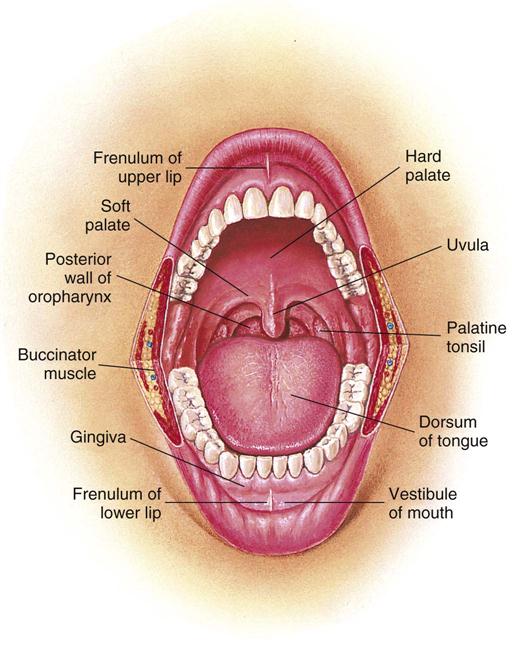
The salivary glands consist of three paired glands: the sublingual, the submandibular, and the parotid. They communicate with the mouth and produce saliva, which serves to moisten the mouth and initiate digestion of carbohydrates. The minor salivary glands exist in the submucosa of the cheeks, tongue, palates, and floor of the mouth, pharynx, lips, and paranasal sinuses.
The sublingual gland lies on the undersurface of the tongue beneath the mucous membrane on the floor of the mouth and the side of the tongue, on the inner surface of the mandible. The many tiny ducts of each gland separately enter the oral cavity on the sublingual fold.
The submandibular gland lies partly above and partly below the posterior half of the base of the mandible and on the mylohyoid and hyoglossus muscles. Its duct (Wharton duct) runs superficially beneath the mucosa of the floor of the mouth and enters the oral cavity behind the central incisors.
The parotid gland, the largest of the salivary glands, lies below the zygomatic arch in front of the mastoid process and behind the ramus of the mandible; it is divided into a superficial portion and a deep portion. The parotid duct (Stensen duct) pierces the buccal pad of fat and the buccinator muscle, finally opening into the oral cavity opposite the crown of the upper second molar tooth.
Pharynx
The pharynx extends from the posterior portion of the nose to the esophagus and larynx and serves as a channel for both the digestive and respiratory systems (Figure 19-8). It is composed of muscular and fibrous layers with a mucous membrane lining. It is approximately 13 cm long and lies anterior to the cervical vertebrae and posterior to the nasal and oral cavities. The pharynx is associated above with the sphenoid sinus and the basilar part of the occipital bone, and it joins the esophagus below. Seven cavities communicate with the pharynx: the two nasal cavities, the two tympanic cavities, the mouth, the larynx, and the esophagus. The pharynx comprises three groups of constrictor muscles. Each muscle fits within the one below, and each inserts posteriorly in the median line with its mate from the opposite side. The constrictor muscles provide constriction of the pharynx for swallowing. Between the origins of the constrictor muscle groups are the so-called intervals, through which ligaments, nerves, and arteries pass. The pharynx is divided anatomically into three sections: the nasopharynx, the oropharynx, and the hypopharynx.
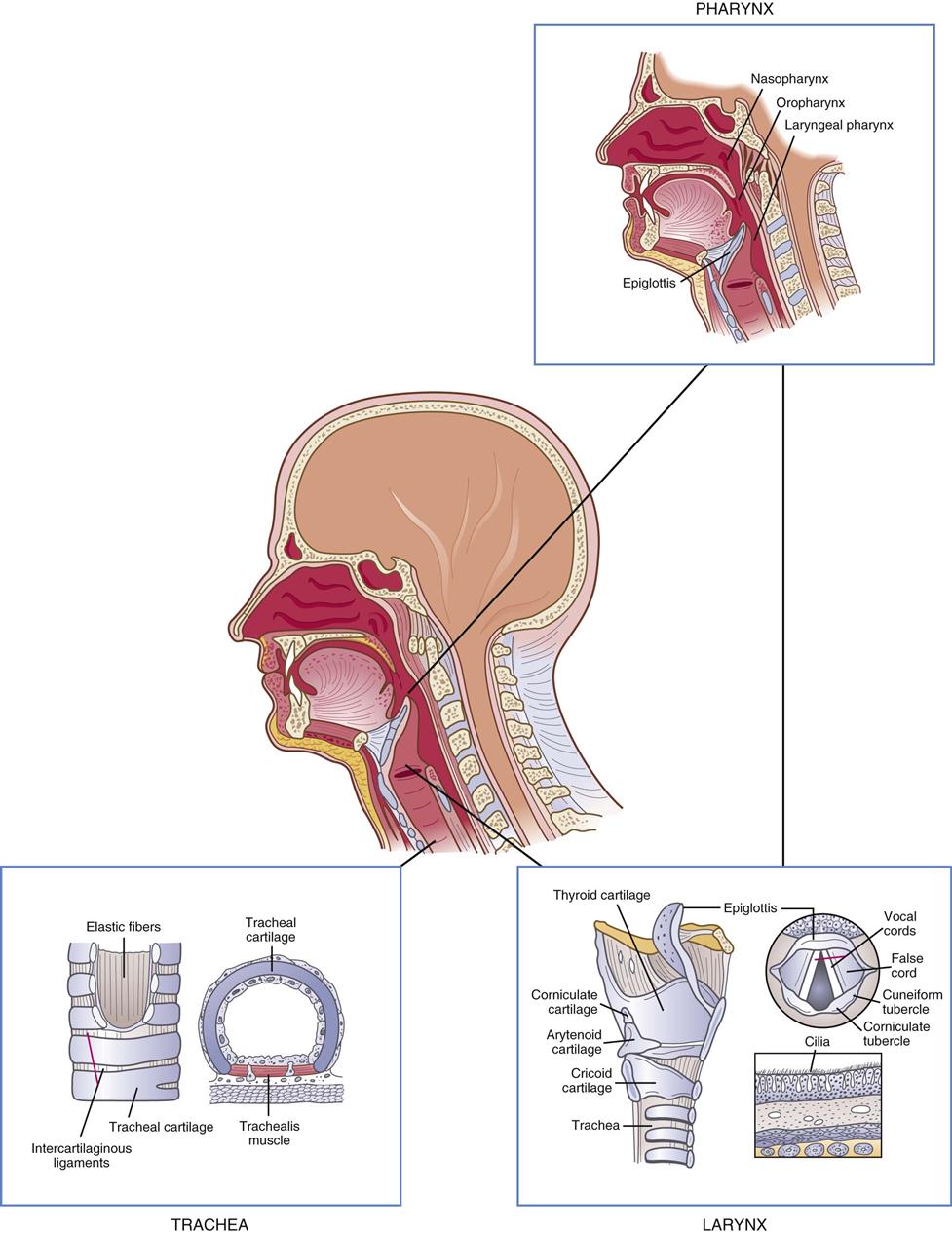
Nasopharynx.
The nasopharynx lies posterior to the nasal cavity and extends over the soft palate. It communicates with the oropharynx through the pharyngeal isthmus, which is closed by muscular action during swallowing. Infection can spread from the nasopharynx to the middle ear through the eustachian tube.
Oropharynx.
The oropharynx lies posterior to the oral cavity and extends from the palate to the level of the hyoid bone. The tonsils are situated on each side of the oropharynx, lodged in a tonsillar fossa that is attached to folds of membrane-containing muscle. The palatine tonsils (a pair of oval structures) are the only lymphatic organs covered with stratified squamous epithelium. The lateral surface of each tonsil is usually covered with a fibrous capsule. The anterior and posterior tonsillar pillars join to form a triangular fossa, with the posterior lateral aspects of the tongue at its base. The lingual tonsils are lodged in each fossa. The adenoids, or pharyngeal tonsils, are suspended from the roof of the nasopharynx and consist of an accumulation of lymphoid tissue.
Hypopharynx.
The hypopharynx extends from the hyoid bone and empties into the esophagus posteriorly and the larynx anteriorly. The piriform sinuses are bound medially by the arytenoepiglottic fold and laterally by the thyroid cartilage and hypothyroid membrane. The fossae are involved in speech.
Larynx and Associated Structures
Larynx.
The larynx is a cartilaginous box that lies midline in front of the fourth, fifth, and sixth cervical vertebrae between the trachea and the root of the tongue, at the upper front part of the neck. The location of the larynx between the gastrointestinal (GI) and respiratory systems is strategic in protecting the airway during swallowing and breathing. The larynx has three main functions: as a passageway for respiration, as a valve to prevent aspiration, and as a vibratory source for vocalization.
The larynx can be divided into three portions: supraglottis (or upper portion above the true vocal cords), glottis (level of the true vocal cords), and subglottis (below the true vocal cords). The upper portion of the larynx is continuous with the pharynx above and includes the epiglottis, vallecula, and the laryngeal cartilages. Its lower portion joins the trachea. The skeletal structure provides for patency of the enclosed airway. The complex muscle action and arrangement of tissues within the larynx provide for closure of the lumen, to protect against trauma and entrance of foreign bodies, and for speech.
Laryngeal Cartilages.
The skeletal framework of the larynx consists of cartilages and membranes. Of the nine separate cartilages, three are single and six are arranged in pairs. The main cartilages of the larynx include the thyroid, the cricoid, the epiglottis, two arytenoid, two corniculate, and two cuneiform. The thyroid cartilage, or Adam’s apple, forms the anterior portion of the voice box. The cricoid cartilage is a complete cartilaginous ring that resembles a signet ring; it rests beneath the thyroid cartilage and supports the airway (see Figure 19-8). The epiglottis is a slightly curled, leaf-shaped, elastic, fibrous membrane that is attached in the midline to the upper border of the thyroid cartilage. The epiglottis helps protect the larynx during swallowing. Contraction of the cricothyroid muscle pulls the thyroid cartilage and the cricoid cartilage to tighten the vocal cords and close the glottis. The arytenoid cartilages, which rest above the signet-ring portion of the cricoid cartilage, support the posterior portion of the true vocal cords.
Laryngeal Ligaments.
The extrinsic ligaments of the larynx are those connecting: (1) the thyroid cartilage and epiglottis with the hyoid bone, and (2) the cricoid cartilage with the trachea. The intrinsic ligaments of the larynx are those connecting several cartilages of the organ to each other. They are considered the elastic membrane of the larynx.
The mucous lining of the larynx blends with fibrous tissue to form two folds on each side of the larynx. The upper set is known as the false vocal cords. The lower set is called the true vocal cords because they are concerned primarily with the speaking voice and protection of the lower respiratory channels against the invasion of food and foreign bodies. The region of the larynx at the true vocal cord level is called the glottis, a triangular space between the vocal cords. During swallowing, the rising action of the muscular larynx, the closure of the glottis, and the doorlike action of the epiglottis all serve to guide food and fluid into the esophagus.
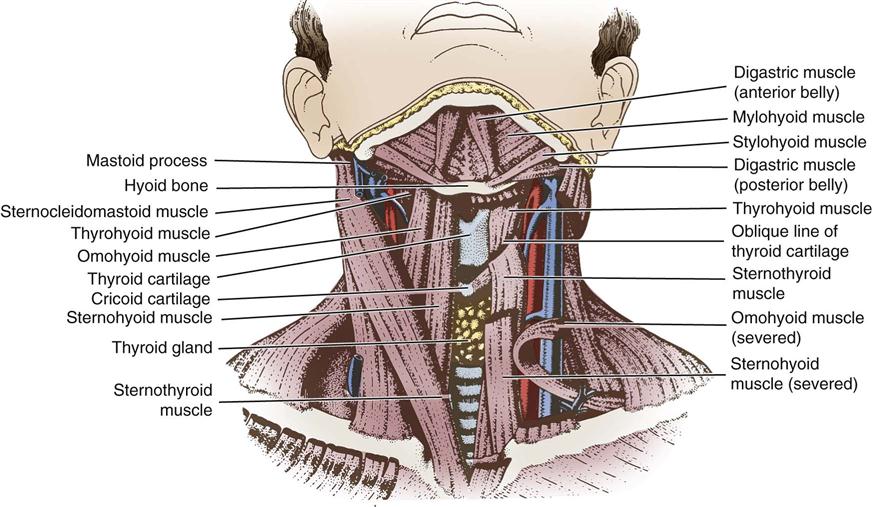
Laryngeal Muscles.
The laryngeal muscles perform two distinct functions: the extrinsic muscles (Figure 19-9) regulate the degree of tension on the vocal cords, and the intrinsic muscles open and close the glottis. The spoken voice also depends on the sphincter action of the soft palate, tongue, and lips. The muscle action of the larynx permits the glottis to close either voluntarily or involuntarily by reflex action. The closure of the inlet by this mechanism protects the respiratory passages. The closure of the glottis and the action of the vocal cords are precisely coordinated to produce the voice.
Trachea.
The trachea is a cartilaginous tube about 15 cm in length and 2 to 2.5 cm in diameter. It begins in the neck and extends from the lower part of the larynx, on a level with the sixth cervical vertebra, to the upper border of the fifth thoracic vertebra. It descends anteriorly to the esophagus, enters the superior mediastinum, and divides into right and left main bronchi. The trachea is composed of a series of C-shaped rings of hyaline cartilage. The posterior surface of the trachea is flattened rather than round because the cartilaginous rings are incomplete. The carina is a ridge on the inside of the bifurcation of the trachea. It is a landmark during bronchoscopy and separates the upper end of the right main branches from the upper end of the left main branches of the bronchi. Branches from the arch of the aorta—the brachiocephalic (innominate) and left common carotid arteries—are in close relation to the trachea. The cervical portion of the trachea is related anteriorly to the sternohyoid and sternothyroid muscles and to the isthmus of the thyroid gland.
Musculature of the Neck
A layer of deep cervical fascia surrounds the neck like a collar and is attached to the trapezius and sternocleidomastoid muscles. The sternocleidomastoid muscle extends from the upper part of the sternum and medial third of the clavicle to the mastoid process. The trapezius muscle extends from the scapula, the lateral third of the clavicle, and the vertebrae to the occipital prominence. The relationship of these muscles to each other and to the adjacent bone creates triangles used as anatomic landmarks.
The pretracheal fascia of the neck lies deep in the strap muscles (sternothyroid, sternohyoid, thyrohyoid, and omohyoid) and partially encloses the thyroid gland, trachea, and larynx. The pretracheal fascia is pierced by the thyroid vessels. It fuses with the front of the carotid sheath on the deep surface of the sternocleidomastoid muscle. The carotid sheath consists of a network of areolar tissue surrounding the carotid arteries and vagus nerve.
Laterally the carotid sheath is fused with the fascia on the deep surface of the sternocleidomastoid muscle; anteriorly it is fused with the middle cervical fascia along the lateral border of the sternothyroid muscle. Lying between the floor and roof of this triangular formation of muscles are the lymph glands and the accessory nerve. Arteries and nerves traverse and pierce this triangle.
Proximal Structures
Cranial Nerves
The trigeminal (fifth cranial) nerve supplies sensory innervation to the face, oral cavity, nose, nasal cavity, and maxillary sinuses. It provides motor innervation to the muscles of mastication.
The right and left facial (seventh cranial) nerves are responsible for all the movements of the facial muscles. Both nerves have a very complex and tortuous course from the brainstem to the motor endplates of the facial musculature. The facial nerve enters the internal auditory meatus along with the eighth (vestibulocochlear) cranial nerve and travels through the internal auditory canal, passing through the labyrinthine portion of the temporal bone to the geniculate ganglion, where it turns sharply and passes superior to the oval window. It then turns inferiorly through the mastoid and exits through the stylomastoid foramen. There are three primary branches of the facial nerve in the temporal bone: the greater superficial petrosal nerve controls lacrimation, the stapedial branch controls the stapedius muscle, and the chorda tympani nerve carries the taste sensation to the anterior two thirds of the tongue.
The vestibulocochlear (eighth cranial) nerve connects the inner ear to the brain through its brainstem nuclei and ascending neural pathways. The recurrent laryngeal branch of the vagus (tenth cranial) nerve is the important motor nerve of the intrinsic muscles of the pharynx and larynx.
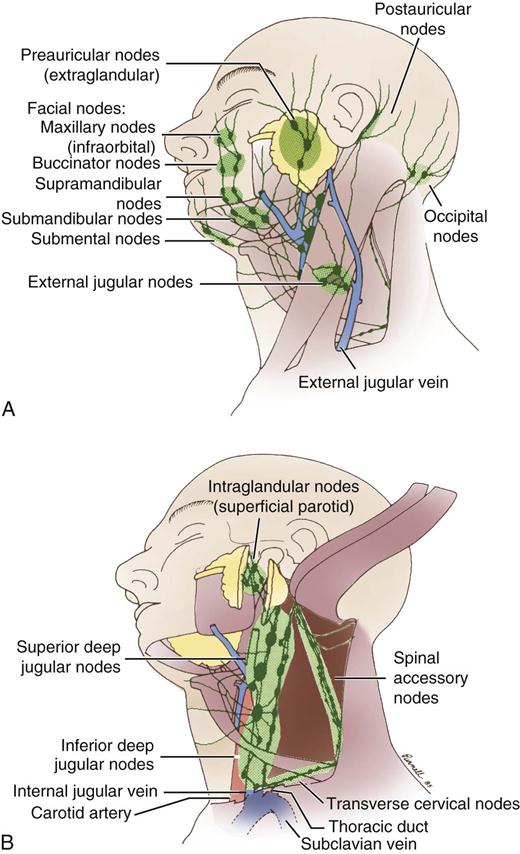
Lymphatic System
The lymphatic system serves both immunologic and circulatory functions. Interstitial fluid, which may contain bacteria, viruses, or tumor cells, is returned to the blood circulation through the lymphatic channels. As the lymph nodes trap the foreign matter, the nodes may become enlarged, infected, or the focus of metastatic cancer (Figure 19-10).
The nasal cavity, the paranasal sinuses, and the pharynx drain into the retropharyngeal nodes. The mouth, lips, and external nose are drained by the submandibular nodes. The lymphatics of the tip and lateral aspects of the tongue drain to the submental nodes, and the posterior tongue lymphatics drain to the cervical nodes.
The lymphatic drainage of the neck can be divided into superficial and deep nodes (Figure 19-11). Lymph nodes of the neck can be further classified into subzones. Level Ia nodes are submental nodes; level Ib nodes are submandibular nodes. Level IIa nodes are upper jugular nodes anterior to cranial nerve IX. Level IIb nodes are upper jugular nodes posterior to cranial nerve IX. Level III nodes are middle jugular nodes. Level IV nodes are lower jugular nodes. Level Va nodes are posterior triangle nodes of the spinal accessory group, and level Vb nodes are posterior triangle nodes of the transverse cervical artery and supraclavicular group. Level VI nodes are anterior tracheal nodes. Level VII nodes are superior mediastinum nodes.
Perioperative Nursing Considerations
Assessment
Assessment is a systematic and intentional process of collecting and interpreting data concerning a patient’s health history and status with diagnoses related to the head and neck. Familiarity with otorhinolaryngologic conditions is essential for effective patient assessment. Information obtained helps develop nursing diagnoses, which direct nursing plans, interventions, and evaluation. A nursing preoperative assessment is usually obtained either in person during scheduled preoperative evaluation or by telephone before the day of surgery. The perioperative nurse should review this assessment as well as the physician’s evaluation to prepare for patient care in the operating room (OR). The assessment should include a review of the following:
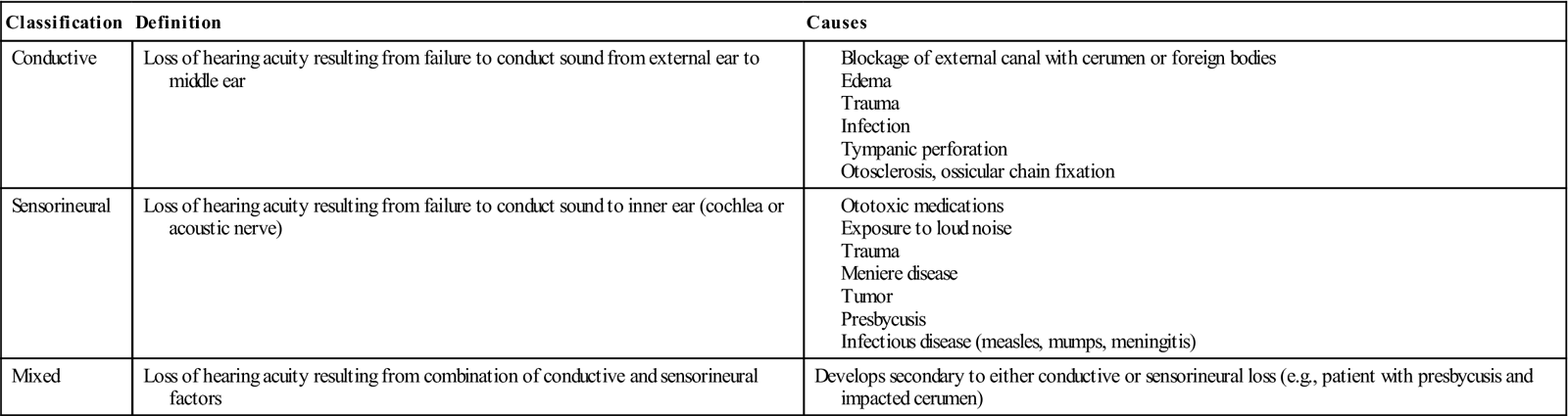
• Communication status. Approximately 17% (36 million) of American adults report some degree of hearing loss severe enough to cause problems with communication and about 2 to 3 of every 1000 children in the United States are born deaf or hard-of-hearing (National Institute on Deafness and Other Communication Disorders [NIDCD], 2010). Hearing loss may be classified as conductive, sensorineural, or mixed (Table 19-1). Nurses must determine the best way to communicate with the patient who is hard-of-hearing (Evidence for Practice). Patients who are unable to speak because of vocal cord dysfunction must be provided an alternate means of communication (e.g., pen and paper, erasable board). Nurses must assess for adaptive responses—lip reading, sign language, written communication—and the effect of the patient’s communication status on daily life (e.g., inability to hear traffic, alarms, or telephone; inability of voice to be heard because of hoarseness; voice volume issues; reluctance to communicate).
• Allergies. Note allergic reactions to medications, foods, or latex.
• Medication history. Note medications taken by the patient for the presenting condition and any other diagnosed medical condition. Medications should include prescription medications; over-the-counter medications; vitamins; herbals; nutraceuticals; ototoxic drugs, including salicylates, aminoglycosides, furosemide, streptomycin, quinine, and ethacrynic acid; or any chemotherapy. Ensure key participants in the patient’s care are aware of the medication history (Ambulatory Surgery Considerations).
• Patient’s knowledge and understanding of the surgical procedure. Note questions and provide answers, or ask surgeon to clarify information for the patient (Patient-Centered Care). Review equipment and care (e.g., suctioning, packing, drains) that will be part of the postoperative regimen and possible communication deficits related to the procedure (e.g., inability to speak after laryngeal procedures, decreased hearing after otologic procedures).
TABLE 19-1
In addition to standard office diagnostic procedures performed by the surgeon, several other tests may be performed before the patient arrives in the OR. Study results of most significance to the perioperative team that should be available in the OR are listed under laboratory data in Appendix A. Radiology studies are described as follows.
Computed Tomography (CT).
CT scans are radiographic studies that visualize structures by producing serial sections, many times clinically referred to as “cuts,” through planes of the head and neck. CT imaging provides visualization of bone, soft tissue, and adjacent intracranial and extracranial pathologic conditions. Intravenous (IV) injection of iodine contrast agents produces visual enhancement of some anatomic structures and pathologic tissues, including highly vascularized tumors. CT is the study of choice to assess intratemporal bone pathologic conditions and to evaluate the paranasal sinuses and adjacent structures. It is also used in the assessment of the oral cavity and neck.
Magnetic Resonance Imaging (MRI).
MRI is an imaging modality using powerful magnetic and radiofrequency waves to reproduce cross-sectional images of the human body without exposing the patient to ionizing radiation. On an MRI scan, fat and fluid produce high-intensity signals, which appear as bright areas, whereas bone and air emit weak signals and appear as darkened areas. MRI is often used with CT imaging in a complementary fashion when evaluating lesions in and around bone for a variety of head and neck conditions, including tumors in the oral cavity, external auditory canal, middle ear, and mastoid.
Audiogram.
Patients scheduled for otologic surgery may have undergone evaluation of their hearing through audiograms to determine whether they have normal hearing, conductive hearing loss, or sensorineural hearing loss (see Table 19-1). Two types of audiometric testing—pure tone and speech audiometry—are performed on patients with suspected hearing loss.
Nursing Diagnosis
Nursing diagnoses related to the care of patients undergoing otorhinolaryngologic surgery might include the following:
Outcome Identification
Outcomes identified for the selected nursing diagnoses could be stated as follows:
• The patient will be able to identify factors that cause anxiety and verbalize an ability to cope.
• The patient will demonstrate effective breathing patterns.
• The patient will experience a sense of self-worth and self-respect.
• The patient will establish an effective communication method with staff and family.
Planning
The development of a plan of care is based on the preoperative assessment, nursing diagnoses, expected outcomes, and the surgery being performed. Patients undergoing otolaryngologic procedures may have special communication needs that must be considered in planning effective care. The perioperative nurse should determine the best way to communicate with patients who have hearing deficits or impaired vocalization. Information given to the patient should be reinforced as needed throughout the perioperative experience. The OR environment must be quiet and free of any loud noise. Intraoperative noises, such as those from suction, electrosurgical units (ESUs), and other equipment, should be explained to the locally anesthetized patient before they are generated. This will help avoid startling the patient and adversely affecting the success of the surgery. Patients receiving local anesthetics need to remain still during the procedure, so providing for comfort measures becomes especially important. The room temperature should be regulated at a comfortable setting, and the patient should be adequately covered to maintain normal body temperature.
Preparation of the OR includes checking the availability and functional capacity of suction, the surgeon’s headlight and light source, and the ESU. It is essential that the x-ray view box is in working order and appropriately located so that scans may be easily viewed by the surgeon during the procedure. In endoscopic cases the navigation tower and monitor should be rolled to the head of the table and tested to ensure proper functioning of the light source for the camera wands and suction. If the surgeon plans on video-recording the case, assurance that the video recorder is adequately working is needed before the start of the case.
A Sample Plan of Care for a patient undergoing otorhinolaryngologic surgery is shown on pages 637-638.