Rebecca M. Patton
Workplace Issues and Staff Safety
Increasingly there is recognition that patient and employee safety programs should be considered together instead of as two separate programs. The Joint Commission (TJC) recognizes synergy between patient safety and worker safety as instrumental in helping organizations to keep both their patients and healthcare workers safe (TJC, 2012a). If the goals of healthcare are to reduce the burden of illness, injury, and disability and to improve the health and functioning of patients, then unsafe working environments must be corrected in order to achieve these goals. Perioperative nurses play a critical role in making the workplace environment safer (Spratt et al, 2012). They strive daily to keep the operating room (OR) safe for patients, other members of the perioperative staff, and themselves.
Employers create a climate of safety for their employees and patients by providing a framework of institutional support. Factors that affect the safety climate include management commitment to safety, healthcare worker involvement in safety decisions, implementation of measures to reduce safety hazards in the work environment, opportunity for feedback on safety improvements, and individual accountability.
Yet even with strong institutional support, OR nurses and surgical technologists face daily challenges to their health and safety and the effectiveness with which they can do their jobs. Routine occupational activities, such as lifting patients and equipment, can cause back injuries and musculoskeletal disorders, and unsafe working environments can lead to occupational injuries from slips, trips, and falls. In addition, OR nurses and surgical technologists regularly face low-level but repeated exposure to numerous hazardous materials, including residues from medications, anesthetic gases, sterilization chemicals, radiation, latex, cleaning chemicals, and disinfection agents. Surgical team members also risk injuries from sharps and exposure to bloodborne pathogens, hazardous chemicals, and workplace violence. Risks specific to the perioperative environment are biologic, ergonomic, chemical, physical, psychosocial, and cultural.
Ergonomics
Perioperative nurses and surgical technologists routinely face a wide array of occupational hazards that place them at risk for work-related musculoskeletal injuries, a frequent and costly occupational issue in nursing (AORN, 2013). More than any other work-related injury or illness, musculoskeletal disorders (MSDs) are responsible for lost work time (Waters, 2010), the need for protracted medical care, and permanent disability among healthcare workers (ANA, 2008). Nurses are known to be at risk for work-related injuries, and many nurses accept musculoskeletal pain as part of their job, with 52% reporting musculoskeletal pain such as back pain (Hunter et al, 2010; Pompeii et al, 2009). The extent of musculoskeletal injuries among nurses should be no surprise, given that nurses lift and turn patients and move heavy equipment every day.
Studies of back-related workers’ compensation claims reveal that nursing personnel have high claim rates compared with other occupations (King, 2011). Back injuries affect approximately 38% of all nurses (ANA, 2008), and an estimated 12% of nurses who leave the profession each year do so because of back injuries (ANA, 2009).
The high incidence of MSDs among nurses is the cumulative effect of repeated patient handling events, often involving unsafe loads. OR nurses and surgical technologists often lift, transfer, or reposition patients on OR beds and transport vehicles, and assist with prepping with arms outstretched or bodies bent forward in awkward postures and positions. Several factors influence the level of ergonomic risk, including patient weight, transfer distance, extent of the workspace, instrument temperature, unpredictable patient behavior, and awkward positions such as stooping, bending, and reaching (Nelson et al, 2009).
Work in the perioperative environment particularly requires an unavoidable constant—moving and lifting large quantities of patient equipment and instrumentation daily. OR nurses and surgical technologists also face risk of injury by standing on floor lifts and platforms while holding instruments and equipment. An ergonomically healthier workplace can decrease or prevent injury to its workforce.
Safe Patient Handling and Movement
Concerted efforts to address workplace safety for perioperative nurses have been under way for some time. As early as 2005, ANA partnered with AORN, the National Institute for Occupational Safety and Health (NIOSH), and the James A. Haley Veterans Administration Medical Center (VAMC) in Tampa, Florida, to form the Workplace Safety Task Force. Its aim was to prepare a safe patient handling “algorithm” guidance document to support ergonomically healthy workplaces. The task force began by identifying high-risk tasks specific to perioperative nurses that specific ergonomic tools could address. These tasks included transferring patients on and off OR beds, repositioning patients on the OR bed, lifting and holding patients’ extremities, standing for long periods, holding retractors for long periods, lifting and moving equipment, and sustaining awkward positions. Using current ergonomic safety concepts, scientific evidence, and technology, such as safe patient handling equipment, the task force developed seven ergonomic tools, or algorithms, to guide workplace safety in the perioperative setting. These clinical tools are incorporated in AORN’s Safe Patient Handling Tool Kit (AORN, 2012).
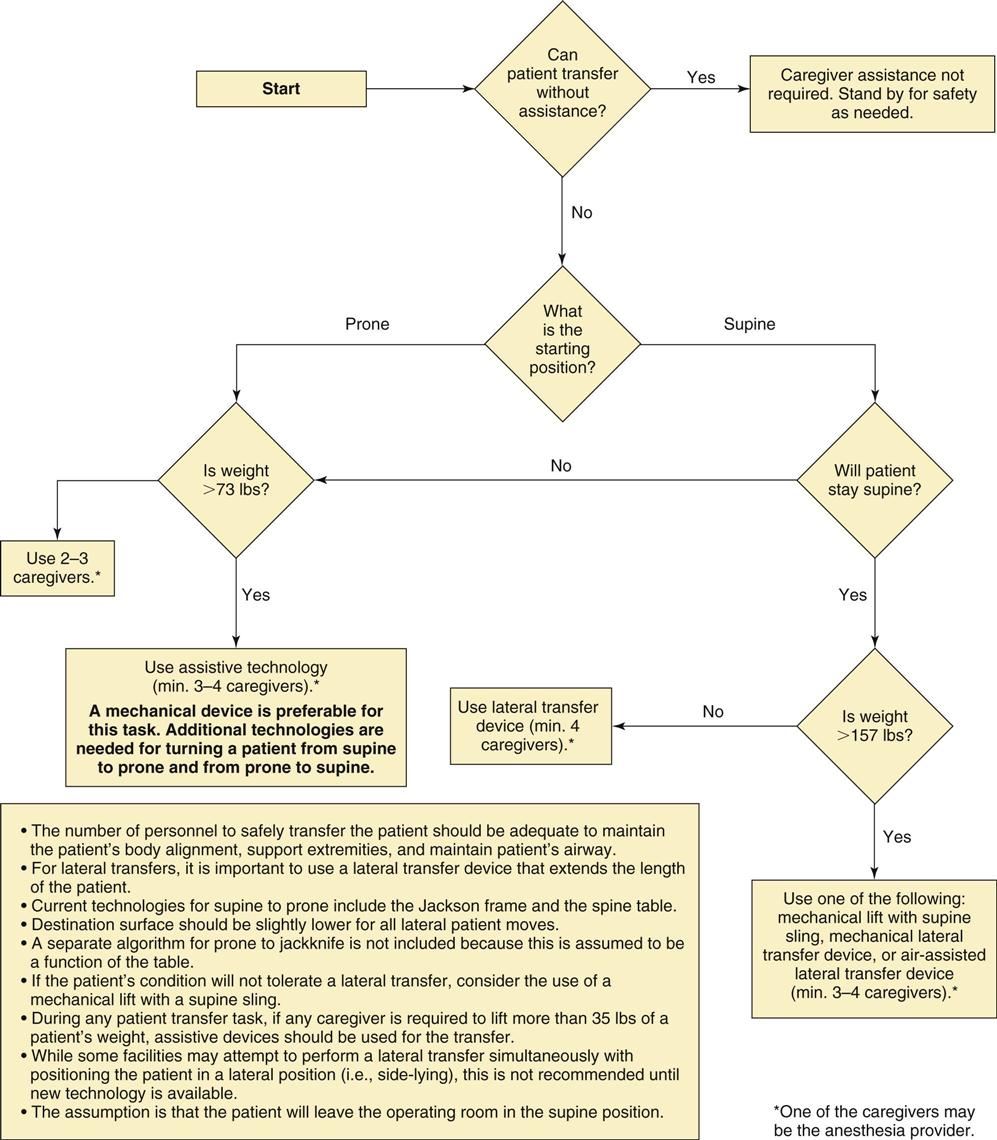
What is an algorithm? An algorithm is a set of rules for solving a problem in a finite number of discrete steps. In this case the algorithm is an ergonomic tool designed to help make decisions in performing various healthcare tasks. The tool directs the caregiver through a series of questions (diamond boxes in Figure 3-1) and provides optimal responses for action—specifically, whether assistive equipment should be used, what type of equipment would best support the task, and how many caregivers are needed to perform the task safely. The purpose of the algorithm is to standardize practice based on research and task analysis, rather than to allow each caregiver to rely solely on his or her own training and experience to make decisions.
The ergonomic tools should be used in the context of an assessment and plan of care for each patient. The plan of care is designed to communicate decisions about safe patient handling practices among all staff likely to participate in these tasks.
Seven Ergonomic Tools for Safe Patient Handling and Movement
This section explains the seven ergonomic tools for safe patient movement and handling.
Ergonomic Tool #1: Lateral transfer from stretcher to and from the OR bed is shown in Figure 3-1. Lifting and moving patients occurs frequently in perioperative settings, with patients transferring to and from transport carts and the OR bed. Many patients completely or partially depend on help with moving because of sedation and/or anesthesia. Lifting and moving patients is a hazardous patient care activity. Fully 38% of all nurses have suffered injuries related to moving, lifting, or repositioning patients, and about one half of all nurses have experienced chronic pain that they associate with these activities (Waters et al, 2011a).
Ergonomic Tool #2: Positioning and repositioning the patient on the OR bed into and from the supine position. The surgical team often repositions patients once they are on the OR bed to provide appropriate exposure of the surgical site. They frequently lift and maneuver the patient while simultaneously placing a positioning device. Ergonomic Tool #2 provides guidelines for repositioning the patient in a safe manner (Waters et al, 2011b).
Ergonomic Tool #3: Lifting and holding legs, arms, and head for prepping in a perioperative setting. OR nurses often lift or hold patients’ limbs during skin prep. Ergonomic Tool #3 is a table that provides calculations to determine whether it is safe for only one caregiver to lift the weight of various limbs and the safe length of time the limbs can be lifted (Waters et al, 2011c).
Ergonomic Tool #4: Prolonged standing. This tool provides relief to OR nurses and surgical technologists who are often required to stand in one place for long periods during surgery. Prolonged standing can cause acute and chronic back, leg, and foot pain, as well as fatigue (Hughes et al, 2011).
Ergonomic Tool #5: Retraction. OR team members must sometimes hold retractors for long periods of time to expose the surgical site. This tool considers whether a self-retaining retractor can be used safely and, if not, how to determine an optimal working height and posture for the retracting team member (e.g., assistant in surgery, such as a physician’s assistant [PA] or registered nurse first assistant [RNFA]) (Spera et al, 2011).
Ergonomic Tool #6: Lifting and carrying supplies and equipment. Members of the OR team lift and carry many types of supplies, instrument trays, and equipment. This tool uses the NIOSH lifting index (described following) to predict the risk of back pain from lifting specific objects in the OR (Waters et al, 2011d).
Ergonomic Tool #7: Pushing, pulling, and moving equipment on wheels. This tool makes recommendations on the number of people required to safely push or pull equipment on wheels; it is especially useful for prescribing safe movement of hospital and OR beds (Waters et al, 2011e).
The use of assistive devices is recommended for situations where manual lifting puts the caregiver at substantial risk of injury. According to ANA’s Handle with Care campaign, the development of patient care ergonomics programs that include the use of assistive patient handling equipment and devices has essentially rendered “manual” patient handling unnecessary. A growing selection of equipment and devices is designed for the variety of patient handling tasks performed by nurses. Box 3-1 lists a number of such patient handling devices. Figure 3-2 illustrates a ceiling lift device in use in the OR.

NIOSH Lifting Equation
The recommendation to use lifting devices for moving patients arises from a body of research that demonstrates that mechanical lifting equipment, as part of a program to promote safe patient handling, can significantly reduce musculoskeletal injuries among healthcare workers. In 1981 NIOSH developed a lifting equation to calculate recommended weight limits for specified two-handed, manual lifting tasks (Waters, 2007). Although NIOSH did not originally recommend the equation for the lifting of humans, it has revised the equation and now recommends it for many patient lifting activities under certain conditions (e.g., when the patient can follow directions or when an estimate of the weight the caregiver must handle is possible). The revised NIOSH lifting equation (RNLE), promulgated in 1991, provides a mathematical equation to determine the recommended weight limit (RWL) and lifting index (LI) for selected two-handed manual lifting tasks. RWL is defined for a specific set of task conditions and represents the weight of the load that nearly all healthy workers can perform over a substantial period (e.g., up to 8 hours) without an increased risk of developing lifting-related low back pain.
The concept behind the lifting equation is to start with a recommended weight that is considered safe for an ideal lift and then to reduce the weight as the task becomes more stressful (e.g., the distance of the load from the worker increases, the duration of the task increases, the type of handhold varies) (AORN, 2012). In general, the revised equation yields a recommended 35-pound maximum weight limit for use in patient handling tasks. When the weight to be lifted exceeds this limit, assistive devices should be used (Waters, 2007).
The formula produces a recommended weight limit that can be used to determine the lifting index. This lifting index may then be used to identify potentially hazardous lifting jobs or to compare the relative severity of two jobs for the purpose of selecting the better option. The equation has also been used to provide recommendations for lifting objects such as lead aprons, sterile packs, body positioning devices, and instrument pans or trays (AORN, 2012).
Slips, Trips, and Falls
Although slips, trips, and falls (STFs) may occur in many places throughout a hospital or ambulatory surgery center, the OR is of special focus here because it is where critical patient care occurs. An STF that disables a worker is expensive in terms of direct and indirect costs, but a disabling fall of an OR team member may adversely affect a patient as well. A fall in the OR can cause direct patient injury, disrupt the surgical procedure, contribute to surgical errors, and delay the current surgery as well as other scheduled surgeries while other staff attend to or replace the injured staff member (Brogmus et al, 2007).
STFs remain a leading cause of serious injury among hospital workers (Hughes, 2009), accounting for a large proportion of injuries to healthcare workers who lose time from work. Hospitals are responsible for STF incidence rates 67% higher than those in other U.S. private industries (Collins et al, 2008). STFs account for nearly 14% of all workers’ compensation costs (Brogmus et al, 2007). The average cost to an employer when a worker experiences a fall is $12,470 (Hughes, 2009).
STF Causes and Prevention
STFs arise from many factors, including wet floors, uneven floor surfaces, low-profile equipment and cords, cluttered or poorly lit walkways, and improper footwear. Historically, STF incidents largely appeared to be unpreventable, and blame has been laid more often than not on carelessness of the fall victim. Research has shown, however, that a comprehensive STF-prevention program can significantly reduce workers’ compensation claims. To a large degree, STFs are preventable (Collins and Bell, 2012).
Wet Floors.
In one 10-year study, STFs resulting from liquids (e.g., water; fluid; and slippery, greasy, and slick spots) were the most common cause (24%) of STF workers’ compensation claims (Bell et al, 2008). Planning to avoid wet spots, however, can reduce the rate of falls. Providing lids for all cups or other open containers being transported, for example, helps to avoid spills. Likewise, installing paper-towel holders in high-spill areas, such as near scrub sinks, nursing stations, and elevators, helps employees clean up spills easily and promptly (Hughes, 2009).
Wet floors should be signaled by placing highly visible “Caution: Wet Floor” signs, preferably 4 feet tall and with flashing lights, in areas that have been recently mopped (Hughes, 2009). Housekeeping staff should be equipped with beepers so that they can be quickly alerted to spill areas. In a NIOSH study, employees were able to call a housekeeping hotline to report a spill and were encouraged to use pop-up caution signs placed throughout the hospital to cover spills until housekeeping arrived. The hospital also purchased highly visible yellow absorption towels that employees could toss onto a spill until it was cleaned (Bell et al, 2008).
In the OR, liquids on the floor can make an otherwise slip-resistant surface hazardous (Brogmus et al, 2007). Using a dripless, brush-free gel solution for surgical hand scrubs minimizes water splashes. In addition, when used at the surgical site, gel-based skin preps are less likely to run than liquid prep solutions. They are also less likely to pool under patients or to drip and pool on the floor or OR bed.
Pads can be used to temporarily cover a spill that occurs in an OR because fluids spilled during surgery are hazardous (Hughes, 2009). Fluid solidifiers usually are composed of a granulated substance that can be sprinkled onto a spill or poured into a container with fluid. Fluid solidifiers absorb liquid and solidify the fluid into gel. Adding a fluid solidifier in a liquid medical-waste container or on a fluid spill on the floor serves to control fluid and to reduce the risk of slips and falls (Brogmus et al, 2007). Effective containment also includes adequate waste containers for the planned procedure and readily available waste-control supplies, including absorptive products.
Uneven Floor Surfaces.
Falls on the same level also occur at transition areas, such as from dry to wet, on uneven surfaces, or from one type of floor surface to another. Healthcare facilities should ensure that there are no uneven surfaces, including thresholds, on floors. In stairwells with potentially low visibility, the nosing on the top and bottom steps can be painted to provide visual cues.
Obstructed Pathways.
Pathways must be kept clear, particularly of low-profile equipment and cords that can be overlooked easily in patients’ rooms, hallways, ORs, or other care areas (Hughes, 2009). If possible, cords should not cross walkways; if this is impossible, cords should be covered or taped. Extension cords are also often found under desks and at nursing stations; where feasible, cord organizers, cord clamps, or retractable cord holders should be used to minimize these tripping hazards.
Keeping pathways clear is especially difficult in the OR, where multiple cables and cords are used in surgical procedures. Newer ORs are equipped with articulated ceiling-mounted booms that help keep cords off the floor and systems that integrate cables into the OR bed. Cords and cables in older ORs should be routed so that they do not stretch across walking paths, and they should be secured by bundling, taping, or braiding. Routing and securing cords makes it easier to check that all necessary cords are properly connected, and doing so makes it less likely that a patient will be injured or the procedure prolonged because someone trips on a cord (Brogmus et al, 2007).
Low-standing equipment and supplies are potential tripping hazards. These include buckets, rolling stools or stepstools, support structures for equipment, and supply containers. OR staff often has to navigate around intravenous (IV) tubing and poles. Consider marking mobile equipment such as stools with a bright color or a taped X to make them more visible and distinguishable from the floor. Also, even though protective and absorptive mats play a safety role, they too can pose a tripping hazard. Slip-resistant absorptive mats should be used, and soiled absorptive mats should be removed because a mat that is oversaturated can swell and become a slipping and tripping hazard.
Inadequate Lighting.
Lighting throughout the healthcare facility must be adequate to visualize pathways, particularly stairways, when supplies or other items are being carried (Hughes, 2009). Adequate lighting is of specific and critical importance in the OR. Advancements in surgical technology, such as in minimally invasive surgery (MIS), have increased the use of light-emitting diode (LED) monitors in the OR. This increasingly requires dimming general room lighting while leaving the surgical site highly illuminated. Not only does this leave the rest of the OR dimly lit, but also the high illumination on the surgical site makes adapting one’s vision to the dimmer room lighting more difficult. Dimmer lighting tends to heighten the risks of not seeing tripping hazards or fluids on the floor. High-quality monitors used during MIS have surface material that minimizes reflected light. Green filters on ambient lighting during MIS procedures minimize reflection of light off the monitors, provide some illumination for other perioperative team members, and reduce ocular fatigue.
Improper Footwear.
Improper footwear increases the risk of STFs. Lessons can be learned from industries, such as food service and commercial fishing, in which antislip footwear is standard (Hughes, 2009). In its recommended practices for surgical attire, AORN suggests that shoes worn in the OR should have closed toes and backs, low heels, nonskid soles, and meet Occupational Safety and Health Administration (OSHA) standards as well as the healthcare facility’s safety requirements (AORN, 2013).
Programmatic STF Prevention and Reduction
Given the diverse age, job duties, and experience of perioperative staff, an STF program is critical to create a safe work environment. During program development, each healthcare facility should conduct a hazard vulnerability analysis to study its unique hazards so they can be appropriately addressed in a workplace safety program that includes targeted STFs (Collins and Bell, 2009; Hughes, 2009).
A comprehensive prevention program can significantly reduce injuries. NIOSH researchers in one study compared injury rates and workers’ compensation costs for a 10-year period before, during, and after implementation of interventions; they found a 58% reduction in workers’ compensation claims for STFs in the postintervention period (Bell et al, 2008). One key component of a successful STF prevention program is to educate workers about the importance of STF prevention and to encourage every employee to take personal responsibility for eliminating STF hazards. Whether this involves personally cleaning spills or cordoning off an area to alert fellow employees while waiting for housekeeping staff to arrive, a successful STF program requires that all hospital staff share responsibility for prevention (Collins and Bell, 2012).
Sharps Safety and Bloodborne Pathogens
Scope and Significance of Problem
In the high-risk perioperative environment, healthcare workers routinely face exposure to bloodborne pathogens (BBPs) and percutaneous injuries (PIs). Each year an estimated 385,000 needlesticks and other sharps-related injuries occur in the United States (Delisio, 2012)—an average of more than 1000 sharps injuries daily (CDC, 2010b). The OR, with 23% for needlesticks (Jagger et al, 2010) and 33% of PIs, has the highest proportion of needlesticks and overall PIs relative to those sustained in all other hospital settings (Research Highlight). In a 2007 study, nurses working in the OR and/or other perioperative settings had sharp device injury rates double those of nurses in other specialties in the United States and Canada—255 and 569 injuries per 1000 per year, respectively (Clarke et al, 2007). Despite passage of the 2007 Needlestick Safety and Prevention Act, while nonsurgical sharps injuries declined, surgical sharps injuries increased (DeJohn, 2012; Jagger et al, 2010).
Although the hepatitis B virus (HBV), the hepatitis C virus (HCV), and the human immunodeficiency virus (HIV) are the pathogens most commonly transmitted during patient care, injuries from needles and other sharp devices used in healthcare and laboratory settings are associated with the transmission of approximately 20 different pathogens (CDC, 2010b). In one study of the prevalence of BBPs in an urban, university-based general surgical practice, testing revealed that 38% of all operations involved patients infected with a BBP: 26% were infected with HIV, 4% with HBV, 35% with HCV, and 17% with both HIV and HCV (Davis, 2006). The risk of transmission after a needlestick or sharps injury is estimated to be 6 to 30 out of every 100 people for HBV, 3 to 10 out of every 1000 people for HCV, and 1 out of every 300 people for HIV.
Exposure to bloodborne pathogens occurs during all phases of the perioperative process, although cuts or needlestick injuries are more likely during the intraoperative phase of patient care. Risk of a sharps injury increases during more invasive, longer procedures that result in higher blood loss. Fatigue resulting from working extended hours coupled with the fast pace of the perioperative environment may also contribute to increased risk of PIs (AORN, 2013). Other factors that may contribute to surgical PIs include frequent handling of sharp instruments and items, prolonged contact with open surgical sites, presence of relatively large quantities of blood, unsafe needle handling techniques (passing needles and using sharp rather than blunt needles), and failure to use a neutral zone for passing sharps between perioperative team members).
Although injuries from hollow-bore needles constitute the majority of percutaneous injuries in the healthcare field overall, the pattern of injuries inside the OR is somewhat different. Suture needle injuries (SNIs) are by far the predominant cause of PIs in the surgical setting. They account for as many as 77% of PIs (AORN, 2013) and are a primary cause of occupational exposure to BBPs among OR professionals.
Box 3-2 provides information on bloodborne pathogens and legislation.
Preventing Injuries During Surgery
Surgery involves precise, regimented actions that require planning, communication, and teamwork. Using these same elements can mitigate inherent hazards associated with sharp devices in the perioperative setting (AORN, 2013). AORN has developed a list of risk-reduction strategies that OR nurses can use to protect themselves from exposure injuries in surgery. Care in setting up the surgical work area includes placement of sharp items, constant awareness of the location of sharps and other sterile team members during surgery, and careful disposal of sharps after surgery. Such care contributes to ensuring a safe surgical environment for all participants. These risk-reduction strategies appear in the following sections.
Safe Handling Practices for Surgical Sharps.
Observing safety precautions during all phases of surgery, from setup to cleanup, reduces the number of injuries and exposures for all OR personnel.
During preparation for surgery:
• Use neutral or hands-free techniques for passing sharp items, instead of passing hand to hand.
• Give verbal notification when passing a sharp device.
• Be aware of other sterile team members in and near the area when handling a sharp device.
• Keep track of, and account for, all sharp items throughout the procedure.
• Keep hands away from the surgical site when sharp items are in use (e.g., suturing, cutting).
• Inspect the surgical setup used during the procedure for sharps.
• Transport reusable sharps in a closed, secure container to the designated cleanup area.
• Inspect the sharps container for overfilling before discarding disposable sharps in it.
• Do not place hands or fingers into a container to dispose of a device.
The Neutral Zone.
The neutral zone has been defined as a location on the surgical field where sharps are placed in a predesignated sterile basin or tray or on a magnetic pad, from which the surgeon or assistant can retrieve them (AORN 2013; Burns, 2009). After use, the items are placed back in the neutral zone, and the scrub person retrieves them. This technique eliminates hand-to-hand passing of sharps between the surgeon and the scrub person, so that no two individuals touch the same sharp at the same time. Thus its name, the “hands-free technique” (HFT). Because it reduces the chance of accidental needle punctures and cuts, both the American College of Surgeons (ACS) and AORN recommend use of the neutral zone to transfer sharps as a risk-mitigating strategy (IHWSC, 2010).
The following suggestions make valuable use of the neutral zone:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree