DIAGNOSIS
Clinical Presentation
History
- Risk factor screening is a useful tool in the evaluation of patients with osteoporosis, as it allows the physician to recognize factors that can influence bone density and fracture risk (Table 3-1).
- Essential historical information includes the following:
- Height at age 30 years and any loss of height
- Medications, including heparin, thyroid medications, diuretics, hormone replacement/oral contraceptive pills (OCPs), phenytoin/phenobarbital, prednisone, calcium, calcitonin, vitamins, raloxifene, or bisphosphonates
- Dietary history, specifically calcium intake
- Fractures or falls as an adult
- Family history of fractures or osteoporosis
- Physical activity
- Menstrual history
- Pain and functional limitations of activities of daily living
Physical Examination
- A complete physical examination should be performed on each patient, with emphasis on accurate measurement of height and weight.
- A spinal examination should be included, noting evidence of kyphosis, pain, and muscle spasm.
- Gait stability and fall risk should be assessed including balance, proprioception, and muscle strength.
Diagnostic Testing
Laboratories
- Laboratory studies should be limited and directed by the history and physical examination.
- Fractures in relatively young postmenopausal women or those with BMD lower than expected for her age may necessitate a workup for secondary causes of osteoporosis.8
- Comprehensive biochemical profile provides a simple screen for secondary causes, such as calcium-phosphorus ratio for hyperparathyroidism, total protein-albumin ratio for myeloma, and screening for liver and kidney disease.
- Thyroid-stimulating hormone (TSH) should be measured in patients with symptoms of thyroid dysfunction or those who are receiving thyroid replacement.
- 25-Hydroxyvitamin D screens for body stores of vitamin D (desirable ≥30 ng/mL).
- Additional studies can be considered for those with very low bone mass or those who continue to lose bone despite antiresorptive therapy. These studies include parathyroid hormone (PTH) battery, 24-hour urine for calcium excretion, serum protein electrophoresis (SPEP), cortisol levels, estradiol levels in women, testosterone levels in men, screening for celiac disease, and bone biopsy (rarely required).
Imaging
- Bone densitometry has improved the diagnosis and treatment of osteoporosis. It allows the clinician to diagnose low bone mass before a fracture occurs. Bone mass measurement is an accurate predictor of fractures.9
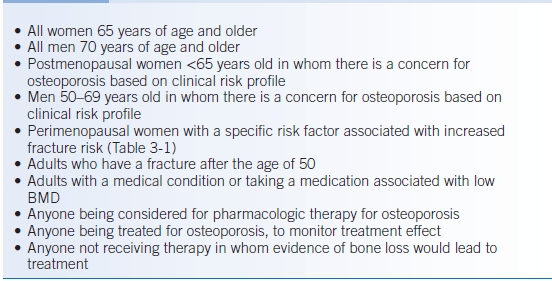
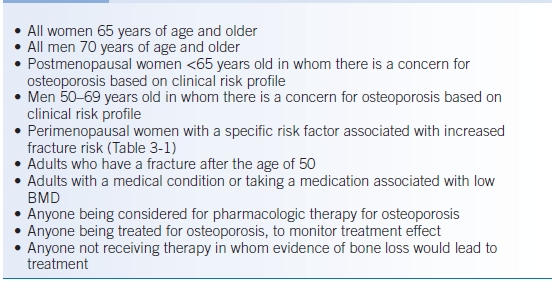
- The indications for bone mineral densitometry according to the Bone Mass Measurement Act of 1998 are presented in Table 3-2 and those of the National Osteoporosis Foundation (NOF) in Table 3-3.10
TABLE 3-2 Indications for Bone Mineral Densitometry, Bone Mass Measurement Act of 1998
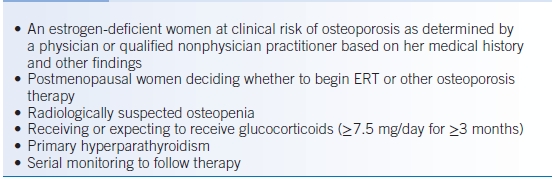
TABLE 3-3 National Osteoporosis Foundation Indications for Bone Mineral Density Testing
- All bone mass measurement techniques are valuable for making the diagnosis of osteoporosis and predicting fracture risk.
- The most widely available methods are single x-ray absorptiometry, dual x-ray absorptiometry (DXA), quantitative computed tomography, and ultrasound densitometry.
- Techniques vary in terms of precision, cost, radiation exposure, and ability to follow changes over time.
- The most common method of measuring bone mass and currently the gold standard is DXA.
- For the diagnosis of osteoporosis, the bone density of a patient is compared with the mean young adult normal reference range (the T score).
- The WHO has developed diagnostic criteria for osteoporosis using T scores (Table 3-4)11:
TABLE 3-4 World Health Organization Criteria for the Diagnosis of Osteoporosis
Diagnostic guidelines developed for postmenopausal women.SD, standard deviation.
- A T score of −2.5 (2.5 standard deviations below the young-adult mean BMD) is defined as osteoporosis because more than half of osteoporotic fractures occur below that level.
- Z scores, which compare a patient’s BMD with that of age-matched controls, are also reported on bone mass measurement.
- If the Z score is more than two standard deviations below age-matched subjects, a cause other than age-related bone loss should be considered, and a secondary cause of osteoporosis should be sought.
- Serial BMD measurements can be used to monitor the effect of treatment or the clinical course of a specific medical condition.
- The usefulness of serial measurements is dependent on the precision error of the measuring device used.
TREATMENT
Medications
- Regardless of the specific therapy for the prevention or treatment of osteoporosis, all patients should receive adequate calcium and vitamin D, engage in regular weight-bearing exercise, and stop smoking.
- According to the NOF, treatment should be strongly considered in postmenopausal women and men aged 50 years or older with the following9:
- Hip or vertebral fracture
- T score of ≤ −2.5 at the femoral neck or spine (after appropriate evaluation to exclude secondary causes)
- Low BMD (T score of −1.0 to −2.5 at the femoral neck or spine) and a 10-year risk of hip fracture of ≥3% or a 10-year risk of any major osteoporotic fracture of ≥20% (based on the WHO FRAX algorithm, http://www.shef.ac.uk/FRAX, last accessed 2/20/14)
First Line
- Bisphosphonates
- For most patients, bisphosphonates are first-line therapy. All increase the BMD and reduce the risk of fractures.
- Bisphosphonates inhibit the action of osteoclasts.
- The bisphosphonates alendronate, risedronate, ibandronate, and zoledronic acid are approved for the prevention and treatment of osteoporosis.
- Orally administered bisphosphonates are poorly absorbed and therefore, should be taken first thing in the morning, on an empty stomach, with no liquid, food, or other medications taken for at least 30 minutes. Calcium supplements should not be taken for at least 1 hour afterwards.
- When taken orally, bisphosphonates may cause esophagitis. Therefore, patients should sit or stand for at least 30 minutes after taking the drug with at least 8 oz of water. If taken properly, tolerance is excellent.12 Less frequent administration may also improve gastrointestinal tolerability.13
- There may also be a link between the administration of bisphosphonates and osteonecrosis (avascular necrosis) of the jaw. The level of risk is not precisely known but is most likely very small. Risk factors appear to be high-dose IV administration, cancer, and dental procedures.14–18
- IV administration can result in flu-like symptoms (fever, arthralgias, myalgias, and headache) and transient hypocalcemia. The latter underscores the importance of calcium and vitamin D supplementation.
- The maximal duration of bisphosphonate therapy is uncertain. However, some recommend discontinuation of therapy or a drug holiday after 5 years.
- An increasing or stable BMD (generally measured every 2 years) is indicative of a positive treatment effect.
- Alendronate
- Alendronate has been shown to improve BMD in the spine by 8.8% and in the hip by 5.9% after 3 years of therapy.19 A meta-analysis of 11 randomized trials found after 3 years of ≥10 mg of alendronate, a 7.48% increase in BMD of the lumbar spine and 5.60% of the hip.20
- Women with osteoporosis treated with alendronate therapy for 3 years (2 years of 5 mg and 1 year of 10 mg) had a reduction in vertebral fractures by 47% and hip fractures by 51%.21 The above-mentioned meta-analysis found a pooled relative risk (RR) of fracture of 0.52 for vertebral fractures and 0.51 for nonvertebral fractures.20
- The recommended dosage for the treatment of osteoporosis in men and women is alendronate, 10 mg PO daily or 70 mg PO once weekly.22
- The dosage for the prevention of osteoporosis in postmenopausal women is 5 mg/day or 35 mg once weekly.
- The dose for the treatment of corticosteroid-induced osteoporosis is 5 mg/day, except in postmenopausal women not receiving estrogen, for whom the recommended dosage is 10 mg/day.
- Alendronate has been shown to improve BMD in the spine by 8.8% and in the hip by 5.9% after 3 years of therapy.19 A meta-analysis of 11 randomized trials found after 3 years of ≥10 mg of alendronate, a 7.48% increase in BMD of the lumbar spine and 5.60% of the hip.20
- Risedronate
- Risedronate has been shown to improve BMD in the spine by 4% to 6% and in the hip by 1% to 3%.23
- The Vertebral Efficacy with Risedronate Trial (VERT) showed a 41% to 49% reduction in spinal fractures and a 39% reduction in nonvertebral fractures.23,24 Women aged 70 to 79 years with confirmed osteoporosis had a 40% reduction in hip fractures with 5 mg/day.25
- A meta-analysis of eight randomized trials found, after at least 1 year of 5 mg risedronate, an increase in BMD of 4.54% for the lumbar spine and 2.75% for the femoral neck. The RR of fracture after at least 1 year of ≥2.5 mg of risedronate was 0.64 for vertebral fractures and 0.73 for nonvertebral fractures.26
- Recommended dosage for treatment and prevention of postmenopausal osteoporosis is risedronate, 5 mg PO daily. The dose for the prevention and treatment of corticosteroid-induced osteoporosis is 5 mg/day, or 35 mg once weekly,27 or 75 mg on 2 consecutive days a month,28 or 150 mg once monthly.29
- Risedronate has been shown to improve BMD in the spine by 4% to 6% and in the hip by 1% to 3%.23
- Ibandronate
- Ibandronate daily or intermittently has also been shown to significantly increase BMD and decrease fractures.30–33
- The recommended dosage of ibandronate is 150 mg monthly.34,35
- Ibandronate can also be administered IV, 3 mg every 3 months.36,37 This regimen may be effective for those who cannot tolerate oral administration or who cannot follow oral dosing precautions.
- Ibandronate daily or intermittently has also been shown to significantly increase BMD and decrease fractures.30–33
- Zoledronic Acid
- IV zoledronic acid is approved for the treatment and prevention of osteoporosis.
- Both once-yearly and intermittent administration increase BMD38 and reduce the risk of vertebral (70%) and hip fractures (41%).39
- If given within 90 days after repair of a hip fracture, zoledronic acid reduces the risk of new fractures (35%) and improves survival (28%).40
- The recommended dosage for treatment of osteoporosis is 5 mg IV over at least 15 minutes annually. For prevention of osteoporosis, the recommended dose is 5 mg IV every 2 years.
- Zoledronic acid also has indications for hypercalcemia of malignancy, multiple myeloma, and bone metastases from solid tumors.
- IV zoledronic acid is approved for the treatment and prevention of osteoporosis.
- Raloxifene
- Raloxifene is a selective estrogen receptor (ER) modulator. It inhibits the loss of BMD but does not cause endometrial hyperplasia.
- In the Multiple Outcomes of Raloxifene Evaluation (MORE) trial, 7,705 women were assigned to receive placebo or raloxifene at 60 or 120 mg. Treatment with raloxifene increased the BMD of the femoral neck and spine by 2.1% to 2.3% and 2.5% to 2.6%, respectively, compared with placebo.41,42 During the 4-year continuation of a subset of MORE subjects (Continuing Outcome Relevant to Evista, CORE), differences in BMD between raloxifene and placebo were maintained.43
- Vertebral fractures were reduced by 30% to 50%.41,42,44
- No data support reduction in nonvertebral fractures at this time.41–44
- The MORE trial revealed a 70% reduction in the development of invasive breast cancer in patients who were treated with raloxifene and had no effect on the endometrium.45 The Raloxifene Use for The Heart (RUTH) trial demonstrated a 43% reduction in invasive breast cancer.46 During the combined MORE/CORE 8 years, there was a 66% reduction in invasive breast cancer and a 76% reduction in ER-positive invasive breast cancer.47 There was no change in the incidence of ER-negative invasive breast cancer.
- Total serum cholesterol and low-density lipoprotein cholesterol levels decreased significantly without change in high-density lipoprotein or triglyceride levels. Raloxifene 60 mg daily reduced the total cholesterol level by 6.4% and the low-density lipoprotein level by 10.1%.48
- Raloxifene does not appear to have a significant effect on the risk of coronary events.46,49
- The risk of venous thromboembolism with raloxifene may be elevated: MORE trial RR 2.1 to 3.1, CORE study RR 2.17, and RUTH trial hazard ratio (HR) 1.44.41,46,47,49,50 The risk is probably less than that seen with tamoxifen.51
- In the RUTH trial, raloxifene was associated with an increased risk of fatal stroke (HR 1.49) but not with total stroke or all-cause mortality.46
- Other side effects include hot flashes and leg cramps.
- The recommended dosage of raloxifene for prevention and treatment is 60 mg daily.
- Calcitonin
- Salmon or human calcitonin can be given as an SC injection or as a nasal spray.
- BMD increases by 1% to 2% in patients who are treated with 200 IU calcitonin nasal spray daily.
- The Prevent Recurrence of Osteoporotic Fracture (PROOF) trial showed a reduction in vertebral fractures by 36% with the nasal spray in women who were 5 years postmenopausal with vertebral fractures. However, 59% of participants withdrew prematurely; therefore, results of this study should be interpreted cautiously. No significant reduction in hip fractures occurred.52
- A meta-analysis showed a reduction in vertebral fractures (RR 0.46) and nonvertebral fractures (RR 0.52).53
- Most consider calcitonin less effective than bisphosphonates.
- Calcitonin has an analgesic effect when given as treatment for compression fractures.54
- Recommended dosage for the treatment of women >5 years postmenopausal with low bone mass is one spray (200 IU) in one nostril daily. The patient should alternate nostrils each day. The SC dose is 100 IU/day.
- Parathyroid Hormone
- PTH is considered to be an “anabolic” treatment, in that it stimulates bone formation rather than acting as an antiresorptive.
- Intermittent PTH administration, as opposed to chronic elevations (as seen with chronic kidney disease or primary hyperparathyroidism), stimulates the maturation of osteoblasts and, therefore, bone formation. The explanation for this incongruity is not fully understood.
- PTH affects trabecular bone more than cortical bone and qualitatively improves trabecular architecture.
- PTH is usually given as recombinant human PTH amino acids 1 to 34, known as teriparatide. Intact PTH is also effective.55
- In the Fracture Prevention Trial (FPT) of 1,637 postmenopausal women with a prior vertebral fracture randomized to placebo or 20 or 40 μg teriparatide daily, BMD increased in the spine and hip but not in the radial shaft.56
- After a median treatment period of 21 months in the FPT, there was significant reduction in vertebral fractures (RR 0.31 to 0.35) and nonvertebral fractures (RR 0.46 to 0.47).56 BMD increases before fracture reduction occurs.
- Side effects include hypercalcemia, nausea, headache, leg cramps, and dizziness.
- Animal studies suggest an increased risk of osteosarcoma. Teriparatide should not be given to patients with existing risk factors for osteosarcoma such as Paget disease, skeletal radiation therapy, or a history of bone malignancy.
- The recommended dosage of teriparatide is 20 μg subcutaneously daily for a maximum of 2 years.
- A bisphosphonate is typically given after completion of teriparatide.57 However, concurrent administration of alendronate does not produce an additive effect and may actually reduce the effects of PTH.58
- Estrogen Replacement Therapy (ERT)
- Estrogen therapy (ET) has been shown to slow down bone loss following menopause or to increase it by as much as 6%.59
- Since the publication of the Women’s Health Initiative (WHI) findings (excess coronary events, strokes, pulmonary emboli, and invasive breast cancer) and the availability of other effective drugs, ET is no longer considered appropriate for first-line therapy for the prevention and treatment of osteoporosis.60
- Dosing is discussed in the “Menopause” section below.
- Denosumab
- Denosumab is a human monoclonal antibody to receptor activator of nuclear factor kappaB ligand (RANKL), an osteoclast differentiating factor. It inhibits osteoclast formation, thereby decreasing bone resorption and increasing BMD.
- Denosumab is approved for treatment of osteoporosis in postmenopausal women at high risk of fracture.
- In the FREEDOM Trial, 7,868 women aged 60 to 90 with osteoporosis were randomly assigned denosumab or placebo every 6 months for 36 months. Denosumab reduced the risk of vertebral fracture by 68%, the risk of hip fracture by 40%, and the risk of nonvertebral fracture by 20%.61
- Recommended dosing is 60 mg subcutaneously every 6 months.
Lifestyle/Risk Modification
Smoking cessation and alcohol intake reduction are important for those with or at risk for osteoporosis.
Diet
- Diet therapy is essential in the prevention and treatment of osteoporosis.
- Calcium supplementation alone has a small positive effect on BMD.62
- Calcium intake for postmenopausal women should be 1,200 mg/day.
- Examples of the elemental calcium content of various foods include the following: 8-oz glass of milk contains 300 mg, 1 oz of Swiss cheese contains 270 mg, and 1 cup of cooked broccoli contains 100 mg.63
- Eating calcium-fortified foods should be encouraged.
- Calcium supplements: Calcium carbonate is acceptable for most patients. It is cheap and has relatively few side effects. Guidelines for calcium supplementation:
- Calcium is best absorbed in small amounts; consider dividing the daily dose if >500 mg.
- Synthetic calcium supplements are optimal. Oyster shell calcium, dolomite, and bone meal can contain heavy metal contaminants.64
- Vitamin D (800 to 1,000 IU PO daily) is beneficial for patients with osteoporosis. Ambulatory men and women older than the age of 65 years who were given calcium carbonate and vitamin D had a significant reduction in nonvertebral fractures.65 Patients with significant hypovitaminosis D require more aggressive repletion.
Activity
Exercise, including weight-bearing and muscle-strengthening exercise, should be encouraged in patients with osteoporosis as allowed by their functional status. <make this reference 115>
SPECIAL CONSIDERATIONS
Management of Corticosteroid-Induced Osteoporosis
- Skeletal effects of corticosteroids include decreased BMD and increased fracture risk and are related to dose and duration of therapy.
- Daily prednisone doses of ≥7.5 mg/day can result in significant bone loss. Lower doses can also have an effect on bone metabolism. Alternate-day regimens have not been shown to be superior.
- Bone densitometry should be considered for any patient who is presently receiving corticosteroids or if long-term therapy is initiated.
- Patients who are on corticosteroids should maintain adequate calcium (1,500 mg/day) and vitamin D (800 IU) intake.
- Weight-bearing exercise should be encouraged.
- Alendronate has been shown to prevent bone loss in patients receiving corticosteroids and to reduce the risk of fractures in postmenopausal women on corticosteroids.66,67
- Risedronate and zoledronic acid are similarly effective.68–71
- Calcitonin may preserve bone loss, but it has not been shown to prevent fractures in the setting of corticosteroid treatment.72,73
- Teriparatide may be more effective than alendronate in patients who have osteoporosis and have received corticosteroids for at least 3 months.74
Management of Osteoporosis in Men
- If a male patient presents with a fracture that is associated with mild-to-moderate trauma, BMD testing should be performed, and a search for secondary causes of bone loss should be considered.
- Evaluation should look for risk factors for osteoporosis including drugs that could affect BMD, such as corticosteroids or anticonvulsants; history of alcohol ingestion (>100 g/day); or nicotine use.
- Appropriate laboratory studies should be done including SPEP, complete blood cell count, calcium, phosphate, albumin, creatinine, alkaline phosphatase, PTH battery, TSH, free testosterone, 25-hydroxyvitamin D, 24-hour urine collection for calcium and creatinine excretion, and cortisol levels.
- Causes of hypogonadism, such as Klinefelter syndrome, hyperprolactinemia, anorexia nervosa, and hemochromatosis, should also be considered. Bone biopsy may be needed if no etiology is found.
- As with female patients, sufficient calcium and vitamin D is important. Patients should be encouraged to stop smoking and drinking alcohol.
- If a secondary cause is found, it should be treated.
- Hypogonadism is a relatively common cause, and testosterone replacement increases BMD.75–77 Alendronate has been shown to maintain BMD and prevent fractures in men with osteoporosis, vertebral fracture (odds ratio [OR] 0.44) and nonvertebral fracture (OR 0.60).78
- Risedronate has been shown to reduce vertebral fractures and increase the bone mass in men treated with corticosteroids.79–82
- Teriparatide has also been shown to be effective in men.83–85
PATIENT EDUCATION
- Patient education is essential for the prevention and treatment of osteoporosis particularly with regard to fall prevention. Patients at risk should be instructed to:
- Look for and remove throw rugs, loose carpets, slippery floors, cords and wires, or anything that can cause a patient to slip.
- Inspect home for unstable furniture or clutter that can obstruct mobility.
- Ensure adequate lighting, especially at night.
- Have grab bars installed for the toilet and place a nonslip surface in the shower.
- Wear properly fitting shoes.
- Have irregular sidewalks and uneven surfaces repaired and have accumulated ice or snow removed.
- Look for and remove throw rugs, loose carpets, slippery floors, cords and wires, or anything that can cause a patient to slip.
- Correct vision and hearing problems.
- Eliminate causes of postural hypotension if possible. Otherwise, advise patients to get up slowly.
- Hip protectors may reduce hip fractures in nursing home patients.86,87 Acceptance of and adherence to hip protectors is relatively low.
Menopause
GENERAL PRINCIPLES
- The menopausal transition period is typified by variation in menstrual cycle length and eventual skipped periods.
- Menopause is the cessation of menstrual periods, defined retrospectively after 12 months of amenorrhea.
- The average age of menopause is 50 to 51 years.88
- With ovarian failure, follicle-stimulating hormone and luteinizing hormone levels rise and estradiol levels fall.
- Other causes of amenorrhea and menopausal symptoms should be considered including excessive weight loss, concurrent medical illnesses, pregnancy, thyroid disease, pituitary disease, and medications.
DIAGNOSIS
Clinical Presentation
- Symptoms associated with menopause include the following:
- Irregular bleeding
- Hot flashes/night sweats
- Sleep disturbance
- Vaginal dryness/itching/dyspareunia
- Sexual dysfunction
- Urinary incontinence
- Mood changes (inconsistent degree of association)
- Irregular bleeding
- Menopausal symptoms typically last for a few months but can persist for several years.88
- Hot flashes affect approximately 75% of menopausal women. They occur most frequently at night and are due to estrogen deficiency. It is believed that estrogen withdrawal lowers the temperature set point in the hypothalamus to reduce the body thermostat. As a result, vasodilatation of the vessels in the hands and upper body occurs so that the heat in the central organs is lost at the periphery.89
- Hot flashes are not synonymous with estrogen deficiency.
- Other causes of hot flashes should be considered, such as pheochromocytoma, carcinoid, pregnancy, thyroid disease, and panic disorder.
- Hot flashes are not synonymous with estrogen deficiency.
- Long-term effects in the postmenopausal period include osteoporosis and increased cardiovascular disease risk.
Diagnostic Testing
- Diagnostic testing is generally unnecessary.
- As noted, follicle-stimulating hormone and luteinizing hormone levels are high and estradiol levels are low.
- Other tests may be indicated to rule out other possible causes of amenorrhea.
TREATMENT
- Hot flashes
- Estrogen therapy (ET)
- ET is the most effective treatment.88,90,91
- However, the results of the WHI and the Heart and Estrogen/progestin Replacement Study (HERS) have greatly called into question the advisability of long-term (i.e., greater than approximately 5 years) or chronic indefinite ET, specifically with regard to combined estrogen and progestin treatment.60,92 It is important to recognize that the direct applicability of these studies to all menopausal women is somewhat tenuous.93
- ET is the most effective treatment.88,90,91
- Quality of life is also a very important consideration.94
- The balance of risks and benefits appears to be more favorable for women who have had a hysterectomy receiving estrogen-only treatment in comparison with women with a uterus receiving combined estrogen-progestin treatment.
- On balance, short-term (i.e., less than approximately 2 to 3 years) administration of the lowest effective dose of estrogen is a viable option for women with moderate-to-severe vasomotor symptoms who have no history of cardiovascular disease, breast cancer, endometrial cancer, or venous thromboembolism.91,93,94
- Low-dose estrogen therapies include 0.3 mg oral conjugated estrogen, 0.25 to 0.5 mg micronized 17β-estradiol, and 0.025 mg transdermal 17β-estradiol patch.93 Higher doses may be necessary in some patients for symptom control.
- A progestin must be added in women with an intact uterus.95
- Low-dose (i.e., containing 20 μg of ethinyl estradiol) OCPs are also a reasonable option for women less than approximately 50 years old.
- ET can generally be tapered off gradually after a year or two. Some women may have recurrent hot flashes.
- Other side effects of estrogen include abdominal bloating, cramps, breast tenderness, hypertriglyceridemia (oral estrogen only), breakthrough bleeding, weight changes, enlargement of benign tumors of the uterus, dry eyes, and skin changes.
- Side effects of progestins include breakthrough bleeding, edema, weight changes, rash, insomnia, and somnolence.
- The balance of risks and benefits appears to be more favorable for women who have had a hysterectomy receiving estrogen-only treatment in comparison with women with a uterus receiving combined estrogen-progestin treatment.
- Other treatments
- Simple environmental changes, including keeping the room cool and dressing in layers, may make hot flashes more tolerable.
- Serotonin reuptake inhibitors (SSRIs, e.g., paroxetine and fluoxetine) and serotonin-norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine) are effective for vasomotor symptoms but not as much as ET.88,91,96
- Gabapentin appears to be effective at reducing the frequency of hot flashes.88,91,97 Doses up to 900 mg/day may be required. Common side effects of gabapentin include dizziness/unsteadiness and fatigue/somnolence.
- Studies regarding clonidine are of fairly low quality and conflicting.88,96
- The effectiveness of soy foods, soy extracts, red clover extracts, and black cohosh is questionable.88,91,96,98,99
- Simple environmental changes, including keeping the room cool and dressing in layers, may make hot flashes more tolerable.
- Estrogen therapy (ET)
- Genitourinary symptoms
- Vaginal atrophy presents with dyspareunia, vaginal dryness, itching, and irritation. Oral and vaginal estrogen is useful for symptoms associated with vaginal atrophy. Systemic effects of vaginal estrogen are probably quite low. Concomitant progestin therapy is not necessary for women with a uterus receiving topical vaginal estrogen.
- The terminal urethra is embryonically related to the vagina. As it becomes thinner, there is more risk of infection and incontinence. Dysuria without evidence of infection is due to the thinning of the epithelium, allowing urine in close contact with the sensory nerves. Also, the normal urethral pressures created by the urethra and surrounding tissues are decreased. Topical estrogen in some studies has been shown to reduce the incidence of urinary tract infections.88,100
- Vaginal atrophy presents with dyspareunia, vaginal dryness, itching, and irritation. Oral and vaginal estrogen is useful for symptoms associated with vaginal atrophy. Systemic effects of vaginal estrogen are probably quite low. Concomitant progestin therapy is not necessary for women with a uterus receiving topical vaginal estrogen.
Cervical Cancer Screening
- Widespread screening with cervical cytology has dramatically reduced the incidence of and mortality from cervical cancer over the last three decades. Half of the women in the United States with invasive cervical carcinoma have never had a Pap smear, and another 10% have not had a Pap smear in 5 years.101
- Risk factors for developing cervical cancer include cigarette smoking, multiple sexual partners, early onset of sexual activity, history of sexually transmitted infection, increasing parity, prolonged use of OCPs, immunocompromise, and HIV infection.102,103
- Human papillomavirus (HPV) is the causative agent in almost all cases of cervical cancer. There are 15 to 18 subtypes of HPV that are considered “high risk” for causing cervical cancer. HPV-16 and 18 account for approximately 70% of all cases.102
- Cervical cancer screening with the Pap smear is recommended for all women who have a cervix. The American Cancer Society (ACS), United States Preventative Services Task Force (USPSTF), American Society for Colposcopy and Cervical Pathology (ASCCP), and American College of Obstetrics and Gynecology (ACOG) recently updated their joint guidelines for cervical cancer screening.
- Screening should begin at 21 years regardless of sexual history.
- ACOG, ASCCP, USPSTF, and ACS recommend the following:
- For women aged 21 to 29, cervical cytology screening alone is recommended every 3 years.
- Women aged 30 to 65 and older with negative results on three consecutive cervical cytology tests may be screened with cervical cytology and HPV cotesting every 5 years. Cytology alone every 3 years is also acceptable.
- Women aged >65 years do not require screening after adequate negative prior screening results.
- Women with a history of CIN 2, CIN 3, or adenocarcinoma in situ should continue routine age-based screening for at least 20 years.
- Women who have undergone hysterectomy for benign indications with previous history of advanced cervical dysplasia do not require screening.102,104,105
- For women aged 21 to 29, cervical cytology screening alone is recommended every 3 years.
- Cervical intraepithelial neoplasias are usually divided into categories based on cytologic grades. The Bethesda system is the currently recognized reporting system. Included in this system is the pathologist’s interpretation of the smear, including the presence of benign cellular changes, evidence of cellular atypia, or both. Infectious processes such as Trichomonas, Candida, Actinomyces

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


