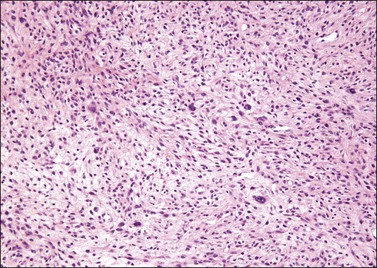
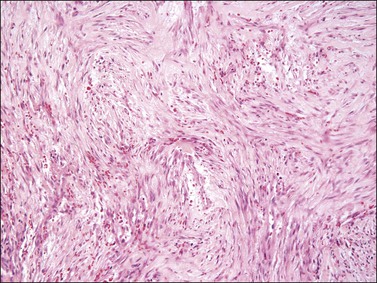
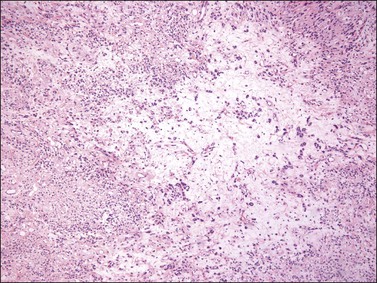
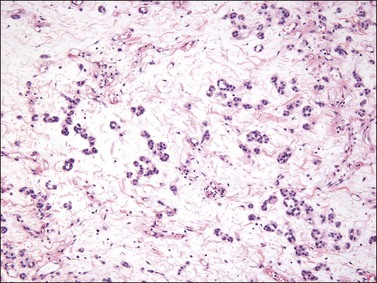
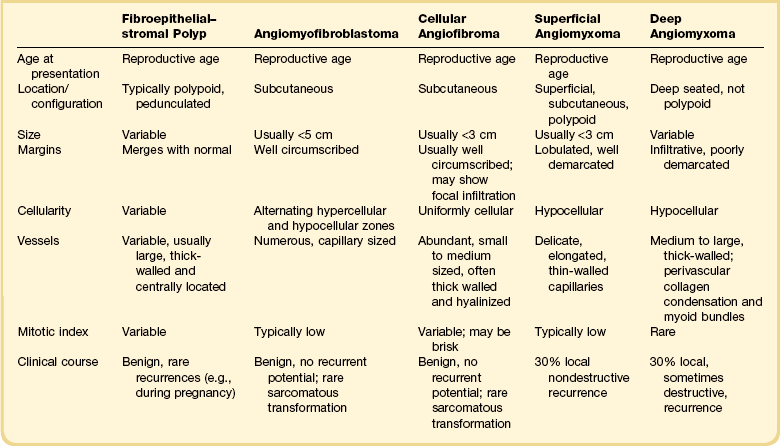
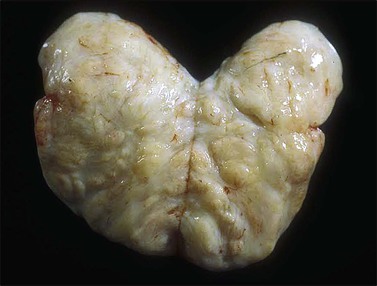
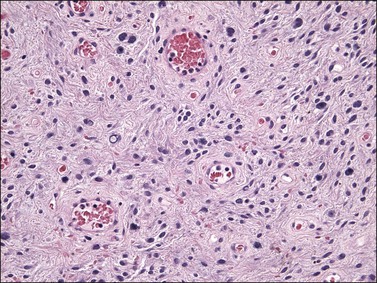
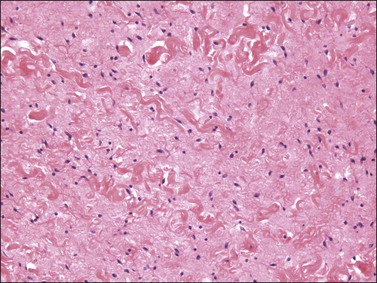
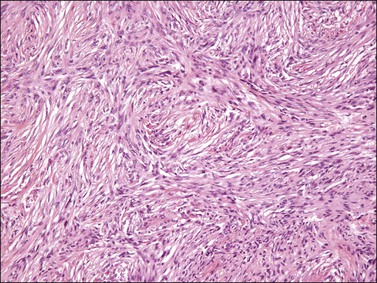
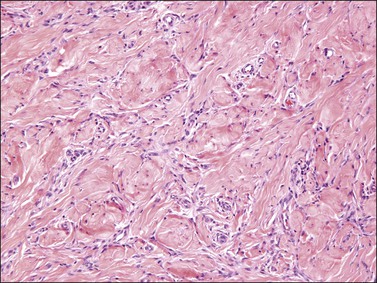
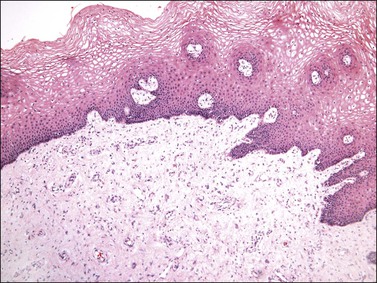
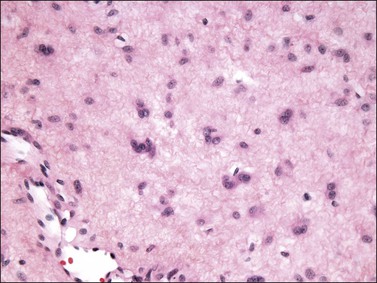
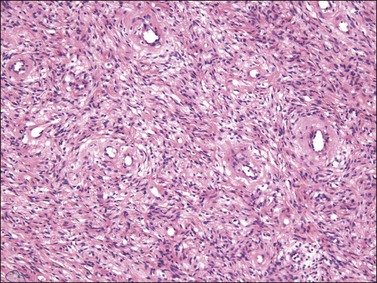
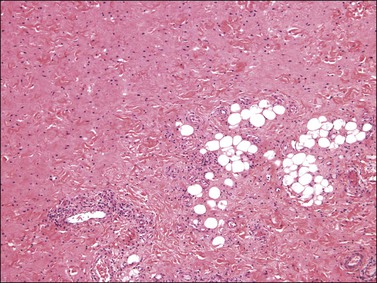
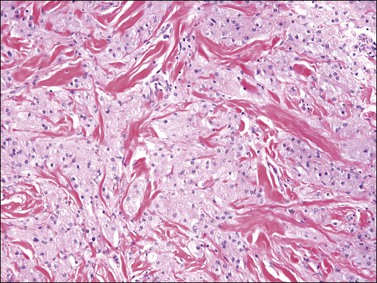
6 Fibroepithelial–stromal polyps, which are hormonally sensitive, most commonly occur in the vulvovaginal region of reproductive age women, often during pregnancy. They may, however, also occur in postmenopausal women on hormonal replacement therapy. Often, the polyps are incidental findings discovered during routine gynecologic examination. Symptoms, when present, may include bleeding, discharge, or the sensation of a mass. These lesions are characteristically polypoid or pedunculated, varying in size but usually less than 5 cm, and are typically solitary, although multiple polyps may occur and are usually associated with pregnancy. Evidence supporting that these lesions are hormonally driven, benign, reactive proliferations include: (1) their occurrence during pregnancy, during which they can be multiple and after which they can spontaneously regress; (2) their association with hormonal replacement therapy in postmenopausal women; and (3) expression of estrogen and progesterone receptors by the constituent stromal cells. Incomplete excision or continued hormonal stimulation (e.g., pregnancy) may be associated with recurrence.1–6 Gross examination typically reveals a polypoid mass with a central fibrovascular core covered by glistening squamous mucosa or skin (Figure 6.1). On occasion, multiple finger-like projections, which may clinically mimic a condyloma, are present. Histologically, these lesions exhibit: (1) a variably cellular spindle cell stroma most often located close to the surface epithelium with scattered stellate and multinucleate stromal cells; (2) a central fibrovascular core; and (3) overlying squamous epithelium or skin, which may exhibit varying degrees of hyperplasia (Figures 6.2 and 6.3). Figure 6.1 Fibroepithelial–stromal polyp. Lesions are typically a polypoid/pedunculated mass. (Courtesy of Dr. J. R. Lewin, Jackson, MS.) Figure 6.2 Fibroepithelial–stromal polyp. The lesion extends up to the epithelial interface without a clearly definable margin. Figure 6.3 Fibroepithelial–stromal polyp. Characteristic appearance of the stellate and multinucleate stromal cells. The stromal component has no clearly defined margin and extends up to the epithelial–submucosal interface. Similar to non-neoplastic vulvar stroma, the stromal cells of these polyps may be reactive for desmin, actin, vimentin, and estrogen and progesterone receptors. The most variable component of these lesions is the stroma, which may exhibit a significant degree of cellularity, nuclear pleomorphism, and mitotic activity, thereby mimicking a malignant process (Figure 6.4).7–10 These worrisome histologic features are particularly, but not invariably, present in polyps that occur during pregnancy (and account for the historical term ‘pseudosarcoma botryoides’).11 Pseudosarcomatous stromal polyps can be distinguished from a malignant process by the presence of stellate and multinucleate stromal cells near the epithelial–stromal interface, which are characteristically present in these polyps even in the most floridly pseudosarcomatous examples, and by the lack of an identifiable lesional margin. Fibroepithelial–stromal polyps are also readily distinguished from botryoid embryonal rhabdomyosarcoma as they are rare before puberty and lack both the characteristic hypercellular subepithelial (cambium) layer of sarcoma botryoides and specific markers of skeletal muscle differentiation.12 A benign, self-limiting myofibroblastic neoplasm characterized by MYH9-USP6 gene fusion that shows rapid growth and spontaneous regression.13–16 Similar to its counterparts elsewhere, nodular fasciitis involving the vulva is usually a well-circumscribed, unencapsulated mass that typically measures less than 3 cm in size. Histologically, it is a relatively well-circumscribed cellular proliferation of loosely arranged spindle cells set within a variably edematous or myxoid matrix that may exhibit microcystic change (Figure 6.5). The spindle cells, which are arranged in short interconnecting fascicles, have bipolar eosinophilic cytoplasmic processes with indistinct borders and ovoid nuclei with occasional nucleoli, imparting an overall appearance to the cells that has been likened to tissue culture fibroblasts. Scattered inflammatory cells, particularly lymphocytes, and extravasated red blood cells are commonly present. Osteoclast-like giant cells are also quite common. Immunohistochemically, the spindle cells are typically reactive for smooth muscle actin and negative for desmin. Nodular fasciitis is distinguished from a sarcoma, particularly leiomyosarcoma at this site, by the following: (1) lack of nuclear hyperchromasia or pleomorphism, (2) lack of necrosis, and (3) characteristic reactive ‘tissue culture’-like myofibroblastic growth pattern. Tumors are typically small (usually <5 cm), well demarcated, tan/white and may have a rubbery consistency (Figure 6.6). They are composed of plump, round to ovoid or spindle-shaped cells, set within a variably edematous to collagenous matrix with alternating zones of cellularity (Figure 6.7). These cells, which have moderate amounts of eosinophilic cytoplasm and round nuclei with fine chromatin and inconspicuous nucleoli, characteristically cluster around the prominent vascular component, which is composed of numerous delicate, thin-walled capillaries (Figure 6.8). Tumor cells may be binucleate or appear somewhat epithelioid. Mitotic activity is typically sparse and occasional cases may have an adipocytic component. The spindle cells are typically reactive for desmin and negative for actin. In postmenopausal patients, lesional cells may be desmin negative.17–22 Figure 6.6 Angiomyofibroblastoma. Well-demarcated, tan/white mass. (Courtesy of Professor P. P. Saint-Maur, Paris, France.) Angiomyofibroblastoma is distinguished from aggressive angiomyxoma by its well-circumscribed margin, its prominent vascular component (which is typically composed of smaller caliber vessels), and its alternating zones of cellularity. As both tumors share a similar immunophenotype, distinction is based on morphologic differences (Table 6.1).23 Cellular angiofibroma is a rare benign stromal tumor that predominantly occurs in the vulva or perineum of middle-aged women (mean 54 years). Although initially described to occur exclusively at this site, they also occur in the inguinoscrotal region in men (so-called angiomyofibroblastoma-like tumor) and in extragenital sites (e.g., retroperitoneum, skin). In the vulva, they most commonly present as a relatively small (mean 2.7 cm) subcutaneous mass that is well circumscribed and painless. Cellular angiofibroma, if completely excised, behaves in a benign fashion with no recurrent potential. Incomplete excision may lead to regrowth of tumor; therefore, local excision with negative margins is adequate treatment. Very rare cases show sarcomatous transformation.24–29 On gross examination, cellular angiofibroma typically is gray-white and has a firm, rubbery consistency (Figure 6.9). Histologically, it is usually well circumscribed; however, focal infiltration into surrounding soft tissue may be present. These tumors are characteristically cellular, composed of the following: (1) short, intersecting fascicles of bland, spindle-shaped cells with ovoid nuclei and scant palely eosinophilic cytoplasm; (2) numerous small to medium sized, thick-walled, and often hyalinized blood vessels; and (3) admixed wispy collagen bundles (Figure 6.10). In approximately 25% of cases, a usually minor component of adipose tissue is present. Mitotic activity, although brisk in some cases, is usually infrequent while necrosis and nuclear pleomorphism are typically absent. On occasion, atypia may be present, most commonly in the form of scattered hyperchromatic multinucleated cells (Figure 6.11). Rarely, abrupt transition to a discrete sarcomatous component can occur, which may exhibit features of atypical lipomatous tumor, pleomorphic liposarcoma or pleomorphic sarcoma, not otherwise specified.29 The spindle cells of cellular angiofibroma are reactive for CD34 in 60% of cases, and less commonly reactive for smooth muscle actin (20%) and desmin (8%). Half of all cases show reactivity for estrogen and progesterone receptors. Keratin, epithelial membrane antigen, and S-100 protein are negative. Figure 6.10 Cellular angiofibroma. Numerous medium-sized, thick-walled vessels are surrounded by short intersecting fascicles of bland spindle cells. Cellular angiofibroma is distinguished from a smooth muscle tumor by its more prominent vascular component, shorter fascicular growth pattern, and relative lack of eosinophilic cytoplasm. Distinction from angiomyofibroblastoma is based on its uniform cellularity; larger, thick-walled, and hyalinized blood vessels; and spindle cells arranged in short intersecting fascicles (Table 6.1).30 Mammary type myofibroblastoma and cellular angiofibroma are both well-circumscribed tumors composed of short intersecting fascicles of bland, CD34-positive spindle cells within a collagenous stroma; however, the vascular component of the former is typically not as prominent but can show a similar degree of hyalinization. These tumors both have similar genetic changes with loss of 13q14 (FOX1A1) and thus likely represent tumors along a spectrum exhibiting varied cellularity and vascularity. A poorly circumscribed, hypocellular lesion composed of bland spindle cells within a variably edematous, myxoid, or collagenous matrix that usually occurs in prepubertal girls.31–32 Histologically, these tumors, which are located in submucosal or subcutaneous tissue, are poorly marginated with infiltration into surrounding tissue, including around adnexal structures and nerves, and into adipose tissue (Figure 6.12). In addition, there is no clear interface with the overlying epithelium. The lesion is hypocellular and composed of a patternless proliferation of bland, uniform spindle cells with ovoid nuclei and palely amphophilic cytoplasm set within a variably myxoid, edematous, or collagenous matrix (Figure 6.13). Small to medium sized vessels, some with mural thickening, are present. Mitotic activity is sparse and nuclear pleomorphism is absent. Lesional spindle cells are typically reactive for CD34 but are negative for smooth muscle actin, desmin, and S-100 protein. Figure 6.12 Prepubertal fibroma. The lesion is typically poorly marginated with infiltration into adipose tissue. Most commonly occurring on the limbs or trunk of adults, dermatofibroma occasionally involves vulvar skin. Although the clinical appearance is variable, most present as a flesh-colored papule, nodule, or plaque; however, some may be pigmented. The diagnosis may be suspected clinically by the presence of the so-called ‘dimpling’ sign; pinching of the tumor results in an inward dimpling of the lesion. Complete excision is usually not necessary unless the tumor shows unusual morphologic features (e.g., cellular, aneurysmal, plexiform, deeply infiltrative, or atypical variants) as these subtypes have locally recurrent potential. Following re-excision, very rare cases of these subtypes have been associated with regional lymph node or metastatic deposits in the lung; however, there are no morphologic indicators in the primary that would predict this biologic potential.33–43 Dermatofibroma exhibits a storiform proliferation of bland spindle cells with varying degrees of hyalinization of the dermal collagen, which is birefringent under polarized light (Figure 6.14). The tumor is relatively well circumscribed; however, entrapment of hyalinized bundles of dermal collagen by the spindle cells at the periphery of the tumor imparts a characteristic pseudoinfiltrative pattern (Figure 6.15). Another characteristic feature is the presence of overlying epidermal hyperplasia, which is common. A number of histologic variants are recognized (although these occur principally outside of the vulva) and include hemosiderotic, lipidized, aneurysmal (angiomatoid), atypical, epithelioid, plexiform, cellular, and deeply penetrating types. The spindle cells are often focally reactive for smooth muscle actin and negative for CD34, although the cellular variant may be reactive for CD34 at the periphery of the tumor. These lesions are often factor XIIIa positive, but most staining is in reactive dermal dendritic cells toward the periphery.33 Dermatofibroma can be distinguished from dermatofibrosarcoma protuberans, its main differential diagnostic consideration, by the following: (1) its lack of infiltration of adipose tissue (although this may be seen in the cellular and deeply penetrating variants), (2) presence of birefringent collagen under polarized light, (3) overlying epidermal hyperplasia, (4) tendency not to infiltrate around adnexal structures, and (5) lack of diffuse reactivity for CD34.43 Granular cell tumor is an uncommon neoplasm that typically arises in the skin and subcutaneous tissue of middle-aged adults with a slightly increased frequency in women. Tumors typically involve the head, neck, and trunk region, but may occasionally occur in the vulva, most often the labium majus. Patients usually present with a solitary, slowly growing, asymptomatic nodule that is often discovered incidentally on clinical examination. If present, symptoms may include pain, increased growth, and pruritus. Complete excision with clear margins is standard treatment, although these tumors seldom recur, even if incompletely excised. Malignant examples are rare.44–49 Granular cell tumors are composed of strands and nests of polygonal cells with abundant eosinophilic granular cytoplasm and small, centrally placed, hyperchromatic nuclei separated by thin fibrous septa (Figure 6.16). Although distinctive, the characteristic granular cytoplasmic change, which is due to the accumulation of lysosomes, is not specific for this tumor type and may be seen in other types of neoplasms, such as smooth muscle tumors. Although many granular cell tumors are relatively well circumscribed, nearly half may show poorly defined or infiltrative margins. Nests of tumor cells adjacent to or surrounding small nerves are common. In addition, the tumor is often associated with overlying pseudoepitheliomatous hyperplasia, which may be mistaken for a squamous neoplasm if the underlying granular cell tumor is overlooked. Granular cell tumors are reactive for S-100 protein, neuron-specific enolase, CD68, and NKI-C3. Figure 6.16 Granular cell tumor. Nests and cords of polygonal cells with abundant eosinophilic granular cytoplasm.
Vulvar Mesenchymal Neoplasms and Tumor-Like Conditions
Tumor-Like Conditions
Fibroepithelial–StromAl Polyp (Pseudosarcoma Botryoides)
Clinical Features
Pathology

Differential Diagnosis
Nodular Fasciitis
Definition
Pathology
Benign Neoplasms
Angiomyofibroblastoma
Pathology

Differential Diagnosis
Cellular Angiofibroma
Clinical Features
Pathology
Differential Diagnosis
Prepubertal Vulvar Fibroma
Definition
Pathology
Dermatofibroma (Fibrous Histiocytoma)
Clinical Features
Pathology
Differential Diagnosis
Granular Cell Tumor
Clinical Features
Pathology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Vulvar Mesenchymal Neoplasms and Tumor-Like Conditions
Only gold members can continue reading. Log In or Register to continue